Peutz-Jeghers polyp
Peutz-Jeghers polyp, abbreviated PJP, is an uncommon hamartomous gastrointestinal polyp. It is usually associated with Peutz-Jeghers syndrome.
| Peutz-Jeghers polyp | |
|---|---|
| Diagnosis in short | |
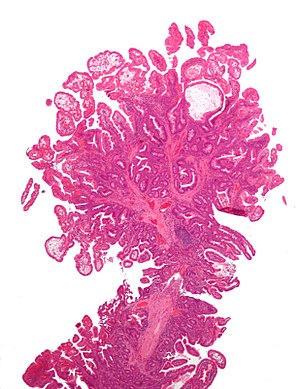 Peutz-Jeghers polyp. H&E stain. | |
|
| |
| LM | polyp with branching or thickened muscularis mucosae, benign epithelium, and lamina propria |
| Molecular | STK11 mutation |
| Site | colon, small bowel, stomach, others |
|
| |
| Syndromes | Peutz-Jeghers syndrome |
|
| |
| Clinical history | family history of cancer - esp. gastrointestinal and breast |
| Prognosis | benign lesion; suggests increased malignancy risk |
| Clin. DDx | other gastrointestinal polyps |
| Peutz-Jeghers polyp | |
|---|---|
| External resources | |
| EHVSC | 10180 |
General
Epidemiology
- Peutz-Jeghers syndrome is autosomal dominant.
- Altered gene: STK11.
Clinical
Features:[3]
- Melanocytic macules.
- Lips, buccal mucosa, and digits.
- Multiple Peutz-Jeghers polyps.
Increased risk of various neoplasms - primarily:
- Breast and gastrointestinal cancer.[4]
- Others tumours:[5]
- Granulosa cell tumour.
- Sertoli cell tumour - esp. with calcification.
Microscopic
- Frond-like polyp with all three components of mucosa:
- Muscosal epithelium (melanotic mucosa, goblet cells).
- Lamina propria.
- M. mucosae.
Notes:
- Frond = leaflike expansion.[6]
- The key is "thick" smooth muscle bundles - if one is lucky one sees branching.[7]
- "Thick" ~= thickness of muscularis mucosae.
- The key is "thick" smooth muscle bundles - if one is lucky one sees branching.[7]
DDx:
- Hyperplastic polyp of the stomach - should not have thickened muscle.
- May be confused with PJP as branching may not be apparent.
Images
IHC
- Chromogranin A - increased staining in relation to background; increased enterochromaffin cells.[8]
Sign out
Duodenum
POLYPS, DUODENUM, EXCISION: - PEUTZ-JEGHERS POLYPS (x2) WITH BRUNNER'S GLANDS. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Colon
POLYP, COLON (40 CM), EXCISION: - PEUTZ-JEGHERS POLYP. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
See also
References
- ↑ 1.0 1.1 Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 859. ISBN 0-7216-0187-1.
- ↑ 2.0 2.1 Bronner, MP. (Apr 2003). "Gastrointestinal inherited polyposis syndromes.". Mod Pathol 16 (4): 359-65. doi:10.1097/01.MP.0000062992.54036.E4. PMID 12692201. http://www.nature.com/modpathol/journal/v16/n4/full/3880773a.html.
- ↑ URL: http://www.ncbi.nlm.nih.gov/omim/175200. Accessed on: 13 July 2010.
- ↑ Beggs AD, Latchford AR, Vasen HF, et al. (July 2010). "Peutz-Jeghers syndrome: a systematic review and recommendations for management". Gut 59 (7): 975–86. doi:10.1136/gut.2009.198499. PMID 20581245.
- ↑ URL: http://www.ncbi.nlm.nih.gov/omim/175200. Accessed on: 22 December 2010.
- ↑ URL: http://dictionary.reference.com/browse/frond. Accessed on: 26 July 2011.
- ↑ C. Streutker. 26 July 2011.
- ↑ Krstić, M.; Katić, V.; Stojnev, S.; Mihailović, D.; Mojsilović, M.; Radovanović, Z.; Zivković, V.. "Peutz-Jeghers syndrome: quantitative study on enterochromaffin cells in hamartomatous intestine polyps.". Srp Arh Celok Lek 141 (9-10): 602-7. PMID 24364221.