Lymphangioleiomyomatosis
Jump to navigation
Jump to search
Lymphangioleiomyomatosis, abbreviated LAM, is a rare lung pathology that predominantly afflicits women of childbearing age.
| Lymphangioleiomyomatosis | |
|---|---|
| Diagnosis in short | |
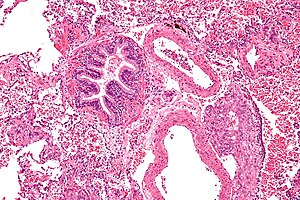 Lymphangioleiomyomatosis. H&E stain. | |
|
| |
| Synonyms | lymphangiomyomatosis |
|
| |
| LM | spindle cells with small nuclei + larger epithelioid cells with clear cytoplasm and round nuclei, cyst formation, thick arterial walls |
| IHC | HMB-45 +ve, ER +ve, PR +ve, SMA +ve |
| Site | lung - see medical lung diseases |
|
| |
| Syndromes | tuberous sclerosis |
|
| |
| Clinical history | almost always women of childbearing age, recurrent pneumothorax |
| Symptoms | dyspnea |
| Prevalence | very rare |
| Radiology | bullae/thin walled cysts distributed in all lung fields, lymphadenopathy |
| Clin. DDx | eosinophilic granuloma, usual interstitial pneumonia, emphysema |
| Treatment | medical therapy, lung transplantation |
It is also known as lymphangiomyomatosis.
General
- Clinical: dyspnea, recurrent pneumothorax.
- May be an indication for lung transplantation.
- Non-neoplastic muscle proliferation versus tumour that can metastasize.[1]
Notes:
- Considered to be a PEComa.
Clinical DDx:[2]
- Pulmonary Langerhans cell histiocytosis.
- Lymphocytic interstitial pneumonia (LIP).
- Pulmonary amyloidosis.
- Birt–Hogg–Dubé syndrome.
Treatment:[3]
- Bronchodilators - symptomatic treatment.
- mTOR inhibitors. (???)
- Transplantation.
Epidemiology
- Associated with angiomyolipomas.[4]
- Associated with tuberous sclerosis[4] - abnormality in same gene (TSC2).
- Usually affects women - primarily in childbearing years; case reports of LAM in men - usu. with TSC.[5]
- Rare.
Gross/Radiology
- Bullae/thin walled cysts - distributed in all lung fields.
- Lymphadenopathy.
Radiologic DDx (of cysts):
- Eosinophilic granuloma - associated with smoking.
- Usual interstitial pneumonia (UIP).
- Emphysema.
Microscopic
Features:[6]
- Spindle cells with small nuclei + larger epithelioid cells with clear cytoplasm and round nuclei.
- Cyst formation.
- Thick arterial walls.
Images
www:
IHC
- HMB-45 +ve.
- ER +ve.
- PR +ve.
- SMA +ve.
See also
References
- ↑ Taveira-DaSilva, AM.; Pacheco-Rodriguez, G.; Moss, J. (Mar 2010). "The natural history of lymphangioleiomyomatosis: markers of severity, rate of progression and prognosis.". Lymphat Res Biol 8 (1): 9-19. doi:10.1089/lrb.2009.0024. PMID 20235883.
- ↑ Xu, KF.; Lo, BH. (2014). "Lymphangioleiomyomatosis: differential diagnosis and optimal management.". Ther Clin Risk Manag 10: 691-700. doi:10.2147/TCRM.S50784. PMID 25187723.
- ↑ Vlachostergios, PJ.; Rad, BS.; Karimi, K.; Apergis, G. (Oct 2014). "Angiomyolipomas, Renal Cell Carcinomas and Pulmonary Lymphangioleiomyomatosis.". J Clin Diagn Res 8 (10): MJ01. doi:10.7860/JCDR/2014/9733.5021. PMID 25478388.
- ↑ 4.0 4.1 http://emedicine.medscape.com/article/299545-overview
- ↑ Schiavina, M.; Di Scioscio, V.; Contini, P.; Cavazza, A.; Fabiani, A.; Barberis, M.; Bini, A.; Altimari, A. et al. (Jul 2007). "Pulmonary lymphangioleiomyomatosis in a karyotypically normal man without tuberous sclerosis complex.". Am J Respir Crit Care Med 176 (1): 96-8. doi:10.1164/rccm.200610-1408CR. PMID 17431222.
- ↑ http://emedicine.medscape.com/article/299545-diagnosis