Leiomyosarcoma
Jump to navigation
Jump to search
Leiomyosarcoma is a malignant tumour of smooth muscle. It is seen in various places including the uterus and skin.
| Leiomyosarcoma | |
|---|---|
| Diagnosis in short | |
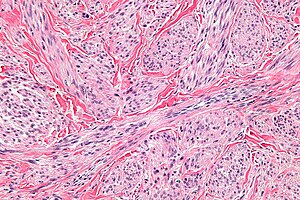 Leiomyosarcoma. H&E stain. | |
|
| |
| LM | fasciclar arrangement (characteristic of smooth muscle), features of malignancy (usually need 2 of 3): † (1) nuclear atypia, (2) tumour cell necrosis, (3) mitoses - variable & definitions suffer from HPFitis |
| Subtypes | major: spindled leiomyosarcoma (leiomyosarcoma NOS), epithelioid leiomyosarcoma, myxoid leiomyosarcoma; minor: leiomyosarcoma with prominent intravascular growth, leiomyosarcoma with osteoclast-type cells, leiomyosarcoma with clear cells, leiomyosarcoma with xanthoma-type cells |
| LM DDx | pleomorphic undifferentiated sarcoma, atypical fibroxanthoma (skin only), EBV-associated smooth muscle tumour, carcinosarcoma, smooth muscle tumour of uncertain malignant potential (STUMP), endometrial stromal sarcoma, atypical leiomyoma (symplastic leiomyoma) |
| Gross | "fleshy" appearance, necrosis, large size |
| Site | uterus, skin, others |
|
| |
| Syndromes | hereditary leiomyomatosis and renal cell cancer |
|
| |
| Prevalence | uncommon |
| Prognosis | poor |
General
- Poor prognosis - usually.
- In locally advanced/metastatic disease (arising from the uterus) the median survival is 12-14 months.[1]
- Do not (generally) arise from leiomyomas.
- Often singular, i.e. one tumour; unlike leiomyomas (which are often multiple).
- May be a part of hereditary leiomyomatosis and renal cell cancer.
Note:
- Skin leiomyosarcoma do so well it has been proposed to no longer refer to them as sarcomas.[2]
Gross
Features:
- "Fleshy" appearance.
- Necrosis.
- Large size.
- Often singular, i.e. one lesion; leiomyomata are often multiple.
Microscopic
Features:
- Usually a cellular lesion.
- Fasciclar arrangement:
- Whorled look at low power.
- Groups of spindle cells cut peripendicular to their long axis adjacent to groups of spindle cells cut in the plane of their long axis.
- Features of malignancy (usually need 2 of 3): †
- Nuclear atypia.
- Tumour cell necrosis.
- Should be patchy/multifocal.
- Zonal necrosis is suggestive of vascular cause.
- Should be patchy/multifocal.
- Mitoses - key feature - definitions suffer from HPFitis:
- +/-Heterologous elements, e.g. malignant cartilage or bone.[4]
Notes:
- † In deep soft tissue. 1 of 3 criteria is considered enough.[5]
- Leiomyosarcoma de facto trumps other sarcomas.[4]
- Mitotic rate seems to be a relatively weak predictor; modest rate may be malignant and a high rate benign.[6]
DDx:
- Pleomorphic undifferentiated sarcoma.
- EBV-associated smooth muscle tumour - rare, immunoincompetent individuals.
- Carcinosarcoma.
- Smooth muscle tumour of uncertain malignant potential (STUMP).
- Endometrial stromal sarcoma.
- Atypical leiomyoma.
Images
Uterine:
Cutaneous:
www:
Subtypes
Major variants:[7]
- Spindled leiomyosarcoma (leiomyosarcoma NOS) - see above.
- Epithelioid leiomyosarcoma.
- Myxoid leiomyosarcoma.
Minor variants:[7]
- Leiomyosarcoma with prominent intravascular growth.
- Leiomyosarcoma with osteoclast-type cells.
- Leiomyosarcoma with clear cells.
- Leiomyosarcoma with xanthoma-type cells.
Epithelioid leiomyosarcoma
Features:[3]
- >50% epithelial appearance.
- >=5 mitoses/HPF - definition suffers from HPFitis.
Image:
Myxoid leiomyosarcoma
Features:[3]
- >=2 mitoses/HPF - definition suffers from HPFitis.
- May have minimal nuclear atypia.
IHC
Features:
- Positive for SMC markers.
- Desmin - present in all three types of muscle.
- H-caldesmon.
- Smooth muscle myosin.
- CD10 -ve.
- May be +ve.[7]
- Some use in the context of uterine lesions -- CD10 +ve in endometrial stromal sarcoma.
Others:[7]
- ER, PR, AR +ve -- 30-40% of the time.
- CD117 +ve/-ve.
- p53 +ve.
- MIB1 high.
- Kertins usu. -ve -- more often +ve in epithelioid variant.
Sign out
SKIN LESION, LEFT SHOULDER (SUTURE AT 12 O'CLOCK), WIDE EXCISION: - LEIOMYOSARCOMA, MARGINALLY EXCISED. -- PLEASE SEE TUMOUR SUMMARY. - DERMAL SCAR.
See also
References
- ↑ Hadoux, J.; Morice, P.; Lhommé, C.; Duvillard, P.; Balleyguier, C.; Haie-Meder, C.; Gouy, S.; Uzan, C. et al. (Sep 2013). "[Uterine leiomyosarcoma: epidemiology, pathology, biology, diagnosis, prognosis and treatment].". Bull Cancer 100 (9): 903-15. doi:10.1684/bdc.2013.1801. PMID 24004576.
- ↑ 2.0 2.1 Kraft S, Fletcher CD (April 2011). "Atypical intradermal smooth muscle neoplasms: clinicopathologic analysis of 84 cases and a reappraisal of cutaneous "leiomyosarcoma"". Am. J. Surg. Pathol. 35 (4): 599–607. doi:10.1097/PAS.0b013e31820e6093. PMID 21358302.
- ↑ 3.0 3.1 3.2 3.3 3.4 Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 281. ISBN 978-0443069208.
- ↑ 4.0 4.1 Anh Tran, T.; Holloway, RW. (Sep 2012). "Metastatic leiomyosarcoma of the uterus with heterologous differentiation to malignant mesenchymoma.". Int J Gynecol Pathol 31 (5): 453-7. doi:10.1097/PGP.0b013e318246977d. PMID 22833086.
- ↑ URL: http://surgpathcriteria.stanford.edu/softsmoothmuscle/soft_tissue_leiomyosarcoma/differentialdiagnosis.html. Accessed on: 10 May 2013.
- ↑ Guo, L.; Liu, T.; Huang, H. (Oct 1996). "[Reappraisal of the pathological criteria for uterine leiomyosarcoma].". Zhonghua Bing Li Xue Za Zhi 25 (5): 266-9. PMID 9388868.
- ↑ 7.0 7.1 7.2 7.3 Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 284. ISBN 978-0443069208.