Gestational trophoblastic disease
Jump to navigation
Jump to search
Gestational trophoblastic disease (abbreviated GTD), also gestational trophoblastic neoplasia (abbreviated GTN), includes choriocarcinoma and hydatidiform moles.
Overview
Most common
Overview of gestational trophoblastic disease:
| Type of mole | Gross | Nuclear atypia | Chorionic villi | IHC | DNA content | Micrographs |
|---|---|---|---|---|---|---|
| Complete mole | "snowstorm" | +/- ? | yes, all abnormal | p57(KIP2) -ve | Paternal, diploid | complete mole + intermed. trophoblast (WC), complete mole (WC) |
| Partial mole | grape-like clusters |
+/- | large villi, villi with cisterns, villi with cytotrophoblastic inclusions |
p57(KIP2) +ve | Maternal & paternal, tripoid | partial mole (utah.edu) |
| Choriocarcinoma | haemorrahagic, necrotic | marked | none | beta-hCG +ve | ? | choriocarcinoma (webpathology.com) |
More comprehensive overview
Benign abnormal looking placenta:
- Placental site nodule (PSN).
- Exaggerated placental site (EPS).
Abnormal fertilization:
Tumours:
- Invasive mole.
- Choriocarcinoma.
- Placental site trophoblastic tumour (PSTT).
- Epithelioid trophoblastic tumour (ETT).
Entities
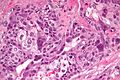
Choriocarcinoma
Main article: Choriocarcinoma
Hydatidiform moles
General
- Significance: increased risk for choriocarcinoma (in complete moles).
- Non-neoplastic proliferation.
Etymology:
- Hydatid is literally watery vesicle.[1]
Types
- Partial mole - see partial mole.
- Complete mole - see complete mole.
Extent:
- Invasive mole - not a subtype.
- Within uterine muscle +/- vessels.
Microscopic
Hydropic changes:
| Entity | Chorionic villi (outline) | Cisterns | Blood vessels | Nucleated RBCs | p57 / Ki-67[2] staining ‡ | Ploidy | Micrograph |
|---|---|---|---|---|---|---|---|
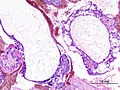
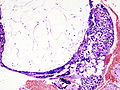
| Complete mole | bizarre; often not ovoid; fissures/slit-like gaps | well-developed | canalicular (thin walled) / few (???) | rare | -ve / ~70% | diploid / tetraploid | [1], [2], [3], [4] |
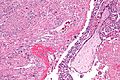
| Partial mole | jagged, still quasi ovoid | poorly developed / small | present | common | +ve / ~70% | triploid | [5], [6] |
| Hydropic abortus | smooth | poorly developed / small | common | common | +ve / ~20% | diploid | [7] |
Note:
- ‡ The amount of Ki-67 staining varies considerably based on what one reads. Chen at al.[3] suggest 25% versus 5% for partial mole versus hydropic abortus.
Mole versus normal
- Moles have large chorionic villi with edema and abnormal blood vessels.[4]
Non-molar versus partial versus complete - short version
Features:[5]
- Non-molar pregnancy: polar proliferation of trophoblastic tissue.
- Partial mole: Norwegian fjord periphery, circumferential or multifocal trophoblastic proliferation, fetal parts.
- Complete mole: grapes grossly, large villi with round borders.
IHC
- p57(KIP2) - the gene is strongly paternally imprinted and the paternal copy is inactived; its expression is from the maternal gene.
Molecular
- The type of mole can be determined by cytogenetics.[8]
Partial hydatidiform mole
- AKA partial mole.
General
Genetics:
- Usually triploid (e.g. 69XXY).
Microscopic
Features:
- Abnormal chorionic villi.
- Villi too large (>0.1 mm ?).
- Villi with cisterns.
- Contain fluid in the centre, i.e. are "hydropic".
- Villi with cytotrophoblastic inclusions.
- Cytotrophoblast in the core of a villus (normally it is only at the surface of the villus).
- May have fetal parts, such as nucleated RBCs.
- Trophoblastic proliferation.
- Without atypia.[9]
- "Norwegian fjord periphery"[5] - jagged border / irregular sawtooth-like periphery.
- Complete moles tend to have a smooth border
DDx:
- Complete hydatidiform mole.
- Placental mesenchymal dysplasia.
- Hydropic abortus - see products of conception and chorionic villi.
Images:
IHC
Features:[10]
- Ki-67 ~ 25+/-5% of cytotrophoblasts and intermediate trophoblasts.
- Hydropic abortus ~ 5+/-1%.
- p53 ~ 22+/-12% of cytotrophoblasts and intermediate trophoblasts.
- Hydropic abortus ~ 5+/-3%.
Complete hydatidiform mole
General
Epidemiology:
- May precede choriocarcinoma[11] ~ 1-2% risk.
Genetics:
- Diploid - most are 46XX.
- Male derived, i.e. arise from DNA in sperm; empty egg fertilized.
Gross/Radiology
Image:
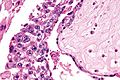
Microscopic
Features:
- No normal villi.
- No fetal parts seen.
- Very rarely nucleated RBCs.
Images
Invasive hydatidiform mole
General
- This is not a distinct subtype - see hydatidiform mole.
Microscopic
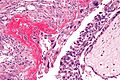
Features:
- Chorionic villi - abnormal +/- normal.
- Trophoblastic cells within uterine muscle +/- vessels - key feature.
DDx:
- Choriocarcinoma - lack chorionic villi, usu. hemorrhagic.
Images
Entities - intermediate trophoblast
| Entity | Key feature | Other histologic features | IHC | DDx | Other | Image |
|---|---|---|---|---|---|---|
| Placental site nodule (PSN) | paucicellular, hyaline material | no mitotic activity | p16 -ve, MIB1 low | EPS, squamous carcinoma | post-partum | (ijpmonline.org) |
| Exaggerated placental site (EPS) | abundant intermediate trophoblasts - between muscle | no mitotic activity | MIB1 ~0% | PSTT, PSN | post-partum | Image? |
| Placental site trophoblastic tumour (PSTT) | abundant cytoplasm - not clear, dyscohesive | +/-multinucleation | MIB1 high, p63 -ve, CD146 +ve | EPS, choriocarcinoma | Other? | (webpathology.com) |
| Epithelioid trophoblastic tumour (ETT) | nests of cells in hyaline stroma | eosinophilic cytoplasm, central nucleus | MIB1 low, p63 +ve, CD146 -ve | squamous carcinoma | Other? | (webpathology.com) |
| Choriocarcinoma | polygonal cells with clear cytoplasm (cytotrophoblasts) | multinucleated cells with smudged nuclei (syncytiotrophoblasts), no chorionic villi | beta-hCG +ve, p63 +ve | invasive hydatidiform mole, PSTT | elevated beta-hCG (serum); not intermediate trophoblast derived. | (webpathology.com) |
Placental site nodule
- Abbreviated PSN.
Main article: Placental site nodule
Exaggerated placental site
- Abbreviated EPS.
- Previously known as syncytial endometritis.[15]
Main article: Exaggerated placental site
Placental site trophoblastic tumour
- Abbreviated PSTT.
- Malignant counterpart of exaggerated placental site (abbreviated EPS).
General
- Derived from intermediate trophoblast.
- Follows pregnancy.
- May be associated with nephrotic syndrome[16] with granular IgM staining.[17]
Clinical:
- Raised (serum) beta-hCG - but usually not has high as in choriocarcinoma.
- Prognosis dependent on time of diagnosis from last pregnancy.
- <48 months = good prognosis.[18]
Microscopic
Features:
- Large cells:
- Nuclear pleomorphism.
- Cytoplasm:
- Abundant.
- Solid, i.e. not vesicular.
- Light basophilic, not clear - key feature.
- NC ratio ~ normal.
- +/-Multinucleated cells.
- Ectatic blood vessels.
Note:
- No chorionic villi.
- If villi are present... it is probably a hydatidiform mole.
DDx:
- Exaggerated placental site - EPS has near zero Ki-67.
- Choriocarcinoma - choriocarcinoma biphasic.[20]
Images:
IHC
Features:[21]
- CD146 +ve.
- p63 -ve.
- Ki-67 ~14+/-7%.
- Choriocarcinoma ~69+/-20%.
Epithelioid trophoblastic tumour
- Abbreviated ETT.
General
- Often in endocervix.
- Malignant counterpart of placental site nodule or PSN.
Clinical:
- Vaginal bleeding.
- Elevated beta-hCG.
Gross
Features:[22]
- Solid mass.
- Flesh-like appearance.
Image:
Microscopic
Features:[23]
- Architecture: nests in hyaline matrix.
- Cytoplasm: abundant, eosinophilic.
DDx:
- Invasive squamous cell carcinoma.
Images:
IHC
Features:[24]
- Cyclin E +ve (nuclear).
- p16 -ve.
- +ve (nuclear) in squamous cell carcinoma of the cervix.
Others:
- HMCK -ve.
- SCC +ve.
Note:
- p63 not useful... +ve in both SCC and ETT.
See also
- Hydatid disease - due to Echinoccus spp. such as E. granulosus.
- Chorionic villi.
- Ectopic pregnancy.
- Placenta.
- Arias-Stella reaction - benign atypical changes of the endometrium associated with trophoblastic tissue.
References
- ↑ URL: http://dictionary.reference.com/browse/hydatid.
- ↑ URL: http://www.ihcworld.com/_newsletter/2003/focus_mar_2003.pdf. Accessed on: 28 May 2011.
- ↑ Chen, Y.; Shen, D.; Gu, Y.; Zhong, P.; Xie, J.; Song, Q. (Mar 2012). "The diagnostic value of Ki-67, P53 and P63 in distinguishing partial Hydatidiform mole from hydropic abortion.". Wien Klin Wochenschr 124 (5-6): 184-7. doi:10.1007/s00508-011-0119-4. PMID 22218717.
- ↑ URL: http://pathologyoutlines.com/placenta.html#hydatgeneral.
- ↑ 5.0 5.1 Howat, AJ.; Beck, S.; Fox, H.; Harris, SC.; Hill, AS.; Nicholson, CM.; Williams, RA. (Jul 1993). "Can histopathologists reliably diagnose molar pregnancy?". J Clin Pathol 46 (7): 599-602. PMID 8157742. Cite error: Invalid
<ref>tag; name "pmid8157742" defined multiple times with different content - ↑ Merchant SH, Amin MB, Viswanatha DS, Malhotra RK, Moehlenkamp C, Joste NE (February 2005). "p57KIP2 immunohistochemistry in early molar pregnancies: emphasis on its complementary role in the differential diagnosis of hydropic abortuses". Hum. Pathol. 36 (2): 180–6. doi:10.1016/j.humpath.2004.12.007. PMID 15754295.
- ↑ 7.0 7.1 Fukunaga, M. (Dec 2002). "Immunohistochemical characterization of p57(KIP2) expression in early hydatidiform moles.". Hum Pathol 33 (12): 1188-92. doi:10.1053/hupa.2002.129421. PMID 12514787.
- ↑ http://jcp.bmjjournals.com/cgi/reprint/51/6/438.pdf
- ↑ URL: http://pathologyoutlines.com/placenta.html#incompletemole. Accessed on: 9 August 2011.
- ↑ Chen, Y.; Shen, D.; Gu, Y.; Zhong, P.; Xie, J.; Song, Q. (Mar 2012). "The diagnostic value of Ki-67, P53 and P63 in distinguishing partial Hydatidiform mole from hydropic abortion.". Wien Klin Wochenschr 124 (5-6): 184-7. doi:10.1007/s00508-011-0119-4. PMID 22218717.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1111. ISBN 0-7216-0187-1.
- ↑ URL:http://www.jultrasoundmed.org/cgi/content/abstract/18/9/589. Accessed on: 27 July 2010.
- ↑ Abike, F.; Temizkan, O.; Payasli, A.; Avsar, F.; Karahan, N.; Baspinar, S. (Jan 2008). "Postmenopausal complete hydatidiform mole: a case report.". Maturitas 59 (1): 95-8. doi:10.1016/j.maturitas.2007.10.005. PMID 18162339.
- ↑ McDonald, TW.; Ruffolo, EH. (Feb 1983). "Modern management of gestational trophoblastic disease.". Obstet Gynecol Surv 38 (2): 67-83. PMID 6300738.
- ↑ URL: http://www.webpathology.com/image.asp?case=565&n=7. Accessed on: 22 May 2014.
- ↑ Bonazzi, C.; Urso, M.; Dell'Anna, T.; Sacco, S.; Buda, A.; Cantú, MG. (Aug 2004). "Placental site trophoblastic tumor: an overview.". J Reprod Med 49 (8): 585-8. PMID 15457847.
- ↑ Komatsuda, A.; Nakamoto, Y.; Asakura, K.; Yasuda, T.; Imai, H.; Miura, AB. (May 1992). "Case report: nephrotic syndrome associated with a total hydatidiform mole.". Am J Med Sci 303 (5): 309-12. PMID 1580319.
- ↑ 18.0 18.1 Schmid, P.; Nagai, Y.; Agarwal, R.; Hancock, B.; Savage, PM.; Sebire, NJ.; Lindsay, I.; Wells, M. et al. (Jul 2009). "Prognostic markers and long-term outcome of placental-site trophoblastic tumours: a retrospective observational study.". Lancet 374 (9683): 48-55. doi:10.1016/S0140-6736(09)60618-8. PMID 19552948.
- ↑ Baergen, RN.; Rutgers, JL.; Young, RH.; Osann, K.; Scully, RE. (Mar 2006). "Placental site trophoblastic tumor: A study of 55 cases and review of the literature emphasizing factors of prognostic significance.". Gynecol Oncol 100 (3): 511-20. doi:10.1016/j.ygyno.2005.08.058. PMID 16246400.
- ↑ URL: http://www.webpathology.com/image.asp?n=3&Case=588. Accessed on: 1 January 2012.
- ↑ Shih, IM.; Kurman, RJ. (Jan 1998). "Ki-67 labeling index in the differential diagnosis of exaggerated placental site, placental site trophoblastic tumor, and choriocarcinoma: a double immunohistochemical staining technique using Ki-67 and Mel-CAM antibodies.". Hum Pathol 29 (1): 27-33. PMID 9445130.
- ↑ 22.0 22.1 Fadare, O.; Parkash, V.; Carcangiu, ML.; Hui, P. (Jan 2006). "Epithelioid trophoblastic tumor: clinicopathological features with an emphasis on uterine cervical involvement.". Mod Pathol 19 (1): 75-82. doi:10.1038/modpathol.3800485. PMID 16258513.
- ↑ 23.0 23.1 URL: http://www.webpathology.com/image.asp?case=589&n=2. Accessed on: 15 August 2011.
- ↑ Mao, TL.; Seidman, JD.; Kurman, RJ.; Shih, IeM. (Sep 2006). "Cyclin E and p16 immunoreactivity in epithelioid trophoblastic tumor--an aid in differential diagnosis.". Am J Surg Pathol 30 (9): 1105-10. doi:10.1097/01.pas.0000209854.28282.87. PMID 16931955.