Endometrium
The endometrium is typically biopsied because of abnormal bleeding. Endometrial hyperplasia and endometrial carcinoma are dealt with in separate articles. An overview of gynecologic pathology is in the gynecologic pathology article.
Indications for endometrial biopsy
Abnormal bleeding:
- Abnormal uterine bleeding (AUB).
- Dysfunctional uterine bleeding, abbreviated DUB, is diagnosed if other causes of bleeding are excluded.
- DUB may get a D&C if they fail medical management.[1]
- Post-menopausal bleeding.
Other indications:[2]
- Products of conception - dealt with in a separate article.
- Dating of endometrium - infertility work-up.
Normal microscopic findings
Endometrium - consists of:
- Epithelium (endometrial glands).
- Stroma (endometrial stroma).
In endometrial biopsies:
- Endocervical glands are commonly seen, as is endocervical mucous.
- This is 'cause the gynecologist scrapes some off on the way in or out.
Glandular telescoping
- Considered an artifact of tissue processing, i.e. normal.[3]
Image:
Endocervical epithelium verus endometrial epithelium
Table
| Feature | Endometrial | Endocervical | Tubal metaplasia |
|---|---|---|---|
| Cytoplasmic staining | usu. hyperchromatic +/-vacuoles | clear or light eosinophilic | hyperchromatic |
| Nuclear-to-cytoplasm ratio | moderate to high (1:2) | low (often 1:3) | high (1:1) |
| Surface features | villi | ||
| Associated stroma | cellular, hyperchromatic | inflamed, less cellular | variable |
List
Endocervical:
- Less hyperchromatic.
- Nuclei round & small.
- Cell borders usually well-defined.
Endometrial:
- More hyperchromatic.
- Nuclei columnar.
Tamoxifen effects
Inadequate endometrial biopsy
- Endometrial biopsies often have scant tissue.
- This is normal in post-menopausal women.
- Ideally, the biopsy should have some endometrial stroma.
- Without stroma it is not possible to assess the gland-to-stroma ratio.
Sign out
No stroma
ENDOMETRIUM, BIOPSY: - VERY SCANT STRIPPED NON-PROLIFERATIVE COLUMNAR EPITHELIUM, PROBABLY FROM THE LOWER UTERINE SEGMENT. - NO DEFINITE ENDOMETRIAL STROMA, SEE COMMENT. - STRIPPED ENDOCERVICAL EPITHELIUM AND ENODOCERVICAL MUCOSA WITHIN NORMAL LIMITS. - MUCOUS. COMMENT: A re-biopsy should be considered within the clinical context.
ENDOMETRIUM, BIOPSY: - VERY SCANT STRIPPED EPITHELIUM PROBABLY FROM THE LOWER UTERINE SEGMENT. - NO DEFINITE ENDOMETRIAL STROMA. - SCANT STRIPPED ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS. - SMALL FRAGMENTS OF DETACHED BENIGN SQUAMOUS EPITHELIUM. COMMENT: A re-biopsy should be considered within the clinical context.
ENDOMETRIUM, BIOPSY: - FRAGMENTS OF DETACHED SQUAMOUS EPITHELIUM AND DETACHED NON-PROLIFERATIVE ENDOMETRIAL GLANDS. - ASSESSMENT LIMITED AS VERY SCANT ENDOMETRIAL STROMA IS PRESENT.
ENDOMETRIUM, BIOPSY: - ENDOMETRIUM: STRIPS OF EPITHELIUM, NON-PROLIFERATIVE. - ENDOCERVIX: SCANT BENIGN EPITHELIUM. - EXOCERVIX: SCANT BENIGN EPITHELIUM. - OTHER: TUBAL METAPLASIA.
ENDOMETRIUM, BIOPSY: - STRIPS OF NON-PROLIFERATIVE ENDOMETRIUM. - SCANT BENIGN ENDOCERVICAL EPITHELIUM. - SCANT BENIGN SQUAMOUS EPITHELIUM. - TUBAL METAPLASIA.
ENDOMETRIUM, BIOPSY: - STRIPS OF BENIGN ENDOMETRIAL EPITHELIUM/TUBAL METAPLASIA, NON-PROLIFERATIVE. - SCANT BENIGN ENDOCERVICAL EPITHELIUM. - RARE SQUAMOUS METAPLASTIC CELLS.
Proliferative without definite stroma
ENDOMETRIUM, BIOPSY: - FRAGMENTS OF DETACHED SQUAMOUS EPITHELIUM, ENDOCERVICAL EPITHELIUM AND FOCALLY PROLIFERATIVE ENDOMETRIAL GLANDS. - ASSESSMENT LIMITED AS NO DEFINITE ENDOMETRIAL STROMA IS PRESENT.
No endometrium
ENDOMETRIUM, BIOPSY: - SPECIMEN INADEQUATE; NO ENDOMETRIUM IDENTIFIED. - ONE VERY TINY FRAGMENT OF ENDOCERVICAL MUCOSA WITHOUT APPARENT PATHOLOGY.
No tissue
ENDOMETRIUM, BIOPSY: - NO TISSUE IDENTIFIED ON MICROSCOPY.
Overview
A simple approach
Low power
- Decide whether you are looking at endometrium.
- Is the gland-to-stroma ratio normal?
- 1:3 is normal.
- If the gland-to-stroma ratio is increased... think complex endometrial hyperplasia.
- If the glands are fused to one another or cribriform... think endometrial carcinoma.
- Glands round?
- Round is normal.
- Irregular - may be seen in secretory phase endometrium, menses, disordered proliferative endometrium (focal), simple endometrial hyperplasia (diffuse).
- Glands pseudostratified?
- Pseudostratified glands are normal in the proliferative phase endometrium, hyperplasias, malignancy.
- Balls of cells?
- Blue - likely menstrual (stromal condensation).
- Pink - consider leiomyoma, squamous morules (associated with endometrial hyperplasia, endometrioid endometrial carcinoma, may be benign).
High power
- Mitoses present in the glands?
- Present in the proliferative phase, hyperplasias, malignancies.
- Mitoses present in the stroma?
- Present in the proliferative phase, hyperplasias, malignancies.
- Mucous present in the glands?
- Present in the secretory phase.
- Inflammatory cells present?
- Some are normal during menses.
Tabular summary
| Diagnosis | Key feature (low power) | Additional features | DDx | Other | Image |
|---|---|---|---|---|---|
| Proliferative phase endometrium | round spaced pseudostratified glands | mitoses in glands and stroma | disordered proliferative phase, simple endometrial hyperplasia, complex endometrial hyperplasia | normal | Image |
| Secretory phase endometrium | irregular glands with secretions or simple glands with vacuoles | decidual changes (nucleus central, eosinophilic cytoplasm, well-defined cell borders) | normal | Image |
Normal endometrium
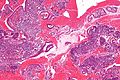
Proliferative phase endometrium
- Abbreviated PPE.
General
- Day 1-13 in the protypical menstrual cycle of 28 days.
- May be day 5-13 - if the menstruation is not included.
- "Exodus" pattern is a term used to describe exfoliation of endometrial cells during the proliferative phase.
- On pap tests this is associated with the classic double contoured balls of endometrial epithelium and stroma.
Note:
- Proliferative phase = follicular phase.
- Gynecologists prefer the ovarian descriptor, i.e. follicular phase; pathologists go by what they see, i.e. proliferative endometrium.
- When the patient is >40 years, some advocate the use of the term proliferative type endometrium (instead of the term proliferative endometrium).[4]
Microscopic
Features:[3]
- Glands:
- Straight, tubular, composed of tall pseudostratified columnar cells - key feature.
- Mitotic figures - key feature. †
- Stroma:
- Cellular stroma (spindle cells).
- Mitoses.
- Usually harder to find than in the glands.
Notes:
- † McCluggage says one shouldn't call PPE without mitoses, as some pseudostratification can be seen in atrophic endometrium.[3]
- There is no guidance on how hard one should look. VL suggests searching ~ 10 mm^2 with the 20x objective. This represents approximately ~ 10 fields of view with a microscope that has a 22 mm eye piece.
- Significant negatives:
- No vacuolation.
- No mucus secretion.
- Inflammation (neutrophils, rare plasma cell) & stromal breakdown common early in the proliferative phase.[5]
DDx:
- Endometrial polyp.
- Disordered proliferative endometrium.
- Endometrial hyperplasia:
- Secretory phase endometrium, early - >=50% of gland have subnuclear vacuoles and >=50% of cells in the glands have subnuclear vacuoles.[6]
Images:
Sign out
ENDOMETRIUM, BIOPSY: - PROLIFERATIVE PHASE ENDOMETRIUM.
ENDOMETRIUM, BIOPSY: - PROLIFERATIVE PHASE ENDOMETRIUM. - ENDOCERVICAL MUCOSA AND STRIPPED ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS.
Not quite normal
ENDOMETRIUM, BIOPSY: - EARLY SECRETORY PHASE ENDOMETRIUM. - FOCUS OF CROWDED PROLIFERATIVE GLANDS, SEE COMMENT. COMMENT: There is a small focus of crowded and irregular proliferative glands without cytologic atypia. The possibility of a polyp is considered but the vessels and polyp-type stroma are lacking. Suggest clincal follow up with a consideration of a repeat biopsy in 3 to 6 months to rule out a hyperplastic lesion.
Post-menopausal
ENDOMETRIUM, BIOPSY: - PROLIFERATIVE TYPE ENDOMETRIUM. -- NEGATIVE FOR HYPERPLASIA. -- NEGATIVE FOR MALIGNANCY.
Micro
The sections show endometrium with proliferative glands without significant dilation or irregularity of shape. The gland-to-stroma ratio is within normal limits. Mitotic activity is mild. No nuclear atypia is apparent.
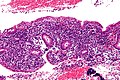
Secretory phase endometrium
- Abbreviated SPE.
General
- Secretory phase = luteal phase.
- Gynecologists prefer the ovarian descriptor, i.e. luteal phase; pathologists go by what they see, i.e. Secretions in the (endometrial) glands.
Gross
- Thickened endometrium.
Microscopic
Early secretory phase
Features - post-ovulatory day 1-5:[8]
- Glands: secretory vacuoles.
- First basal to the epithelial nuclei (infranuclear vacuoles).
- Then apical to the epithelial nuclei (supranuclear vacuoles).
- Mitoses may be present - common when vacuoles are subnuclear.
Mid secretory phase
Features - post-ovulatory day 6-8:[8]
- Glands: Mucus in glands.
- Stroma: Edema (empty space around the glands).
Late secretory phase
Features - post-ovulatory day 9-12:[8]
- Stroma:
- Spiral arterioles.
- Predecidual changes -- mnemonic NEW:
- Nucleus central.
- Eosinophilic cytoplasm key feature (may be subtle to the novice).
- Well-defined cell borders.
Premenstrual
- Stroma: neutrophils, scattered lymphocytes, stromal balls ("blue balls"); "stromal condensation".
- Glands: apoptosis at the base of the gland.[9]
Notes:
- Stromal condensation (stromal balls) - premenstrual - stromal cells tightly packed together; nuclei molded together like in small cell tumours.[10]
- Gland-to-stroma ratio is increased in late secretory phase and menstruation.[11]
- Endocervical epithelium (ECE) has a morphology similar to the epithelium of secretory phase endometrium (SPE):
- ECE - grey foamy appearing cytoplasm.
- SPE - eosinophilic cytoplasm.
- Most useful feature to differentiate ECE and SPE is the accompanying stroma.
DDx:
- Endometrial hyperplasia with secretory changes.
- Endometrium with hormonal changes.
- Proliferative phase endometrium - may have some changes of secretory endometrium; <50% of gland have subnuclear vacuoles or <50% of cells in the glands have subnuclear vacuoles.[6]
Image:
Sign out
ENDOMETRIUM, BIOPSY: - SECRETORY PHASE ENDOMETRIUM.
With additional stuff
ENDOMETRIUM, BIOPSY: - SECRETORY PHASE ENDOMETRIUM. - SCANT ENDOCERVICAL MUCOSA WITHIN NORMAL LIMITS.
ENDOMETRIUM, BIOPSY: - SECRETORY PHASE ENDOMETRIUM. - ENDOCERVICAL MUCOSA AND STRIPPED ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS.
ENDOMETRIUM, BIOPSY: - SECRETORY PHASE ENDOMETRIUM. - BENIGN SUPERFICIAL EXOCERVICAL EPITHELIUM. - SCANT BENIGN ENDOCERVICAL EPITHELIUM.
Menstrual endometrium
General
- Technically part of the proliferative phase or follicular phase.
Microscopic
Features:
- Non-proliferative endometrium.
- Apoptotic cells common.[12]
- Tightly packed cellular balls of stromal cells with nuclear moulding.
- Known as "blue balls".
- Tightly packed cellular stromal cells known as "stromal condensation".
- Inflammation, esp. neutrophils.
DDx:
Images
www:
Sign out
ENDOMETRIUM, BIOPSY: - CONSISTENT WITH MENSTRUAL ENDOMETRIUM: -- STRIPPED NON-PROLIFERATIVE ENDOMETRIAL GLANDS. -- BALLS OF CONDENSED ENDOMETRIAL STROMA. -- ABUNDANT NEUTROPHILS AND BLOOD.
ENDOMETRIUM, BIOPSY: - CONSISTENT WITH MENSTRUAL PHASE ENDOMETRIUM: -- NON-PROLIFERATIVE ENDOMETRIAL GLANDS WITH NEUTROPHILS AND APOPTOSIS. -- BALLS OF CONDENSED ENDOMETRIAL STROMA. -- BLOOD.
Specific entities/abnormalities
Arias-Stella reaction
- Benign atypical endometrial changes associated with chorionic tissue -- may be seen in a completely normal pregnancy and misdiagnosed as a malignancy.[13]
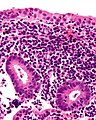
Endometritis
General
- Usually post-delivery or post-instrumentation, e.g. previous biopsy.
- May be spontaneous, e.g. tuberculous endometritis.
Microscopic
Acute endometritis
Features:
- Neutrophils clusters (>5 PMNs) in the:
- Endometrial stroma.
- Within uterine glands.
Notes:
- Neutrophils are normal in the context of menses.
Image:
Chronic endometritis
Features:[14]
- Plasma cells with in the endometrial stroma - key feature.
- Usually superficial/close to the luminal aspect.
- Lymphocytic infiltrate - usu. marked.
- May form lymphoid aggregates - low power finding.
Other findings:[14]
- +/-Necrosis.
- Edema - common.
- Hemorrhage.
Notes:
- One plasma cell is not enough to call it.
DDx:
- Mentrual endometrium - endometrial stromal condensation.
Images
www:
- Chronic endometritis (webpathology.com).
- Chronic endometritis (webpathology.com).
- Tuberculous endometritis (webpathology.com).
Sign out
ENDOMETRIUM, BIOPSY: - CHRONIC ENDOMETRITIS.
Benign endometrial polyp
- Uterine polyp redirects here.
- Abbreviated BEP.
- AKA endometrial polyp.
General
- Very common.
- May be a cause of menorrhagia (heavy & long menses).
Gross
- Polypoid mass in the endometrial cavity.
Gross DDx:
- Secretory phase endometrium.[3]
- Pedunculated leiomyoma.
Microscopic
Features - diagnostic criteria:[3]
- Large blood vessels (muscular) - key feature.
- Fibrotic stroma - key feature.
- Polypoid shape - epithelium on three sides.
- May not be seen... as polyp is fragmented on removal.
Glandular changes common:[3]
- Endometrial glands may be out of phase with surrounding endometrium.
- Often proliferative.
- +/-Cystic dilation of glands/unusual shapes
- Simple endometrial hyperplasia should not be diagnosed in a polyp!
- +/-Focal gland crowding.
Notes:
- Apparently benign polyps should be examined closely at the surface for in situ & invasive malignancies.
- Stroma often cellular.
DDx:
- Adenofibroma.
- Cervical polyp - have endocervical mucosa.
- Lower uterine segment - have endocervical epithelium and lack the thick-walled blood vessels.[3]
- Endometrial carcinoma - esp. serous carcinoma of the endometrium.
Sign out
Non-proliferative
ENDOMETRIUM, CURETTAGE: - BENIGN ENDOMETRIAL POLYP.
ENDOMETRIUM ("POLYPS"), REMOVAL:
- BENIGN ENDOMETRIAL POLYPS WITH CYSTIC GLANDULAR DILATION AND
WITHOUT APPARENT PROLIFERATIVE ACTIVITY.
Suggestive of polyp
ENDOMETRIUM, CURETTAGE: - POLYPOID NONPROLIFERATIVE ENDOMETRIUM WITH FOCALLY PROMINENT SMALL BLOOD VESSELS AND FIBROUS STROMA, SUGGESTIVE OF BENIGN POLYP. - NEGATIVE FOR HYPERPLASIA AND NEGATIVE FOR MALIGNANCY.
Proliferative
ENDOMETRIUM, CURETTAGE: - BENIGN ENDOMETRIAL POLYP WITH PROLIFERATIVE ACTIVITY.
Note:
- It is useful to comment on whether non-polypoid endometrium is proliferative (if present), esp. in menopausal women.[3]
Polyp with disordered proliferative phase in the background
ENDOMETRIUM, BIOPSY: - BENIGN ENDOMETRIAL POLYP WITH PROLIFERATIVE GLANDS AND FOCAL GLAND DILATION. - SUSPICIOUS FOR A BACKGROUND OF DISORDERED PROLIFERATIVE PHASE ENDOMETRIUM, SEE COMMENT. - STRIPPED BENIGN ENDOCERVICAL EPITHELIUM. COMMENT: The endometrium sampled is proliferative with focal gland dilation throughout. The features of a polyp (large muscular blood vessels, fibrous stroma and polypoid fragments of endometrium) are only focally present, suggesting there is a background of disordered proliferative phase endometrium. Clinical correlation is suggested.
Anovulatory endometrium
General
- May be used as a synonym for disordered proliferative phase.[15]
Microscopic
Features:
- Shedding:
- Stromal condensation.
- Apoptotic endometrial epithelium.
- Non-proliferative glands.
DDx:
Sign out
ENDOMETRIUM, CURETTAGE: - NON-PROLIFERATIVE ENDOMETRIUM WITH SMALL ROUND GLANDS AND SHEDDING, SEE COMMENT. - BENIGN ENDOCERVICAL MUCOSA. - NEGATIVE FOR HYPERPLASIA. - NEGATIVE FOR MALIGNANCY. COMMENT: The changes are suggestive of anovulatory bleeding.
Disordered proliferative endometrium
- Abbreviated DPE.
- AKA endometrium with disordered proliferative phase.
- AKA disordered proliferative phase.
General
- Association: anovulation.
- Benign - can be grouped with normal.[16]
Treatment:
Image:
Microscopic
Features:[18]
- Proliferative type endometrium with:
- Cystic dilation of glands focally that do not have (glandular) secretions - key feature.
- Glands >2x normal size - usually 3-4x normal.
- Irregular shape, e.g. gland contour has inflection points.
- Greater than fours glands involved (dilated).
- Cystic dilation of glands focally that do not have (glandular) secretions - key feature.
- +/-Stromal condensation -- balls of stromal tissue, aka "blue balls" (due to breakdown of endometrium).
DDx:
- Proliferative phase endometrium.
- Simple endometrial hyperplasia without atypia - architectural atypia diffuse.
- Benign endometrial polyp.
Notes:
- Proliferative phase endometrium:
- Glands: straight, tubular, tall pseudostratified columnar cells, mitotic figures, NO vacuolation, NO mucus secretion, abundant mitoses.
- Stroma: cellular, stroma (spindle cells), mitoses.
- Eosinophilic syncytial metaplasia - common.
- Features: abundant eosinophilic cytoplasm, mild nuclear atypia +/-loss of nuclear stratification, no mitoses).
Images
www:
Sign out
ENDOMETRIUM, BIOPSY: - DISORDERED PROLIFERATIVE ENDOMETRIUM.
With endocervix
ENDOMETRIUM, BIOPSY: - DISORDERED PROLIFERATIVE ENDOMETRIUM. - BENIGN ENDOCERVICAL MUCOSA.
Waffle a bit
ENDOMETRIUM, BIOPSY: - COMPATIBLE WITH DISORDERED PROLIFERATIVE ENDOMETRIUM (FRAGMENTS OF PROLIFERATIVE ENDOMETRIUM WITH EVIDENCE OF SHEDDING AND VERY RARE GLAND DILATION). - VERY SCANT STRIPPED ENDOCERVICAL EPITHELIUM WITHOUT APPARENT PATHOLOGY. - NEGATIVE FOR ENDOMETRIAL HYPERPLASIA. - NEGATIVE FOR MALIGNANCY.
Micro
The sections show a well-sampled endometrium. Mitotic figures are identified within the glands and stroma. Irregular, moderately enlarged glands are seen (only) in one of several fragments; most of the endometrial glands are round, regular and small.
No stromal condensation is apparent. No secretions are in the glands.
There are no back-to-back glands. No nuclear atypia is apparent. No thick-walled blood vessels are apparent.
Endometrial changes of oral contraception
| Endometrial changes of oral contraception | |
|---|---|
| External resources | |
| EHVSC | 10170 |
- Endometrium with hormonal changes and OCP endometrium redirect here.
- AKA oral contraceptive effect.
General
- Very common.
- Most pills a mix of progesterone and estrogen.
- The progesterone is what generates the characteristic appearance -- that is similar to pregnancy.
Microscopic
Features:[20]
- Inactive glands (round/ovoid glands, simple cuboidal epithelium, no mitoses).
- Stroma decidualized -- mnemonic NEW:
- Nucleus central.
- Eosinophilic cytoplasm.
- Well-defined cell borders.
DDx:
- Endometrial hyperplasia with secretory changes - proliferative activity.
- Secretory phase endometrium - glandular changes of the secretory phase (cytoplasmic vacuolization), secretions in the glands.
Image
Sign out
ENDOMETRIUM, BIOPSY: - NON-PROLIFERATIVE ENDOMETRIAL GLANDS WITH STROMAL DECIDUALIZATION, CONSISTENT WITH EXOGENOUS HORMONES.
OCP effect and shedding endometrium
ENDOMETRIUM, ASPIRATION: - ENDOMETRIUM WITH NONPROLIFERATIVE ENDOMETRIAL GLANDS AND STROMAL DECIDUALIZATION, COMPATIBLE WITH EXOGENOUS HORMONES. - EVIDENCE OF ENDOMETRIAL SHEDDING (BALLS OF CONDENSED STROMA ASSOCIATED NEUTROPHILS, AND BLOOD). - NEGATIVE FOR HYPERPLASIA AND NEGATIVE FOR MALIGNANCY.
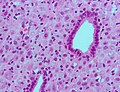
Atrophic endometrium
- Inactive endometrium redirect here.
General
- Endometrium of normal postmenopausal women.
- Menopause typically happens at around 50 years old.
- Very common diagnosis.
- Atrophy may be associated with bleeding and therefore biopsied to rule-out hyperplasia and malignancy.
Gross
- Thin endometrium.
Microscopic
Features:
- Glands - small columnar cells:
- Moderate quantity of eosinophilic cytoplasm.
- Ovoid (palisaded) nuclei +/- nuclear pseudostratification.[3]
- Eosinophilic cytoplasm.
- No mitoses.
- Architecture:
- +/-Cystic dilation.
Notes:
- If a woman is truly postmenopausal, mitoses in the glandular epithelium is pathologic until demonstrated otherwise.
- The exceptions are benign endometrial polyp, uterine prolapse, and possibly inflammation (e.g. the person has had several biopsy attempts and was seeded with pathogens).
DDx:
- Proliferative phase endometrium - esp. if there is pseudostratification.
- Serous carcinoma of the endometrium.
Images:
Sign out
ENDOMETRIUM, BIOPSY: - NON-PROLIFERATIVE ENDOMETRIUM. - BENIGN SQUAMOUS EPITHELIUM WITH METAPLASTIC CHANGE. - SCANT ENDOCERVICAL MUCOSA WITH REACTIVE CHANGES.
ENDOMETRIUM, BIOPSY: - NON-PROLIFERATIVE ENDOMETRIUM. - BENIGN STRIPPED ENDOCERVICAL EPITHELIUM. - NEGATIVE FOR HYPERPLASIA AND NEGATIVE FOR MALIGNANCY.
Micro
The sections show small fragments of endometrium. The gland-to-stroma ratio is normal. The glands are small and round, and have a pseudostratified epithelium.
Mitotic figures are not identified within the glands or stroma. No stromal condensation is apparent. No secretions are in the glands. No nuclear atypia is apparent.
Scant benign endocervical tissue (stripped epithelium and mucosa) is present.
Limited stroma
ENDOMETRIUM, BIOPSY: - STRIPPED NONPROLIFERATIVE ENDOMETRIAL EPITHELIUM; NO APPRECIABLE STROMA PRESENT. - SCANT ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS. - MINUTE FRAGMENTS OF SQUAMOUS EPITHELIUM WITHOUT APPARENT PATHOLOGY.
ENDOMETRIUM, BIOPSY: - SCANT STRIPPED NON-PROLIFERATIVE ENDOMETRIAL EPITHELIUM. - VERY SMALL FRAGMENT OF ENDOMETRIAL STROMA. - TUBAL METAPLASTIC EPITHELIUM.
Micro
The sections show stripped endometrial epithelium and stripped tubal-type epithelium. No mitotic activity is identified. No nuclear atypia is apparent. A small fragment of definite endometrial stroma is present. The gland-to-stroma ratio cannot be assessed due to the limited stroma.
Endometrial hyperplasia
Can be thought of as a precursor lesion for endometrial carcinoma.
It comes in two main flavours:
- Simple.
- Complex.
Each flavour may or may not have nuclear atypia.
Endometrial carcinoma
Endometrial cancer is the most common gynecologic malignancy (in the USA).[21]
See also
References
- ↑ URL: http://emedicine.medscape.com/article/257007-treatment. Accessed on: 15 July 2010.
- ↑ Mazur, Michael T.; Kurman, Robert J. (2005). Diagnosis of Endometrial Biopsies and Curettings: A Practical Approach (2nd ed.). Springer. pp. 1. ISBN 978-0387986159.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 McCluggage, WG. (Aug 2006). "My approach to the interpretation of endometrial biopsies and curettings.". J Clin Pathol 59 (8): 801-12. doi:10.1136/jcp.2005.029702. PMID 16873562. Cite error: Invalid
<ref>tag; name "pmid16873562" defined multiple times with different content Cite error: Invalid<ref>tag; name "pmid16873562" defined multiple times with different content Cite error: Invalid<ref>tag; name "pmid16873562" defined multiple times with different content - ↑ GAG. January 2009.
- ↑ Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 197. ISBN 978-0443069208.
- ↑ 6.0 6.1 Mazur, Michael T.; Kurman, Robert J. (2005). Diagnosis of Endometrial Biopsies and Curettings: A Practical Approach (2nd ed.). Springer. pp. 14. ISBN 978-0387986159.
- ↑ URL: http://www.cytochemistry.net/microanatomy/medical_lectures/oviduct_and_uterus.htm. Accessed on: 23 October 2012.
- ↑ 8.0 8.1 8.2 Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 237. ISBN 978-0470519035.
- ↑ TC. 22 June 2009.
- ↑ GAG. 6 Oct 2009.
- ↑ URL: http://www.pathologyoutlines.com/topic/uteruspatternapproach.html. Accessed on: 6 December 2012.
- ↑ Spencer, SJ.; Cataldo, NA.; Jaffe, RB. (May 1996). "Apoptosis in the human female reproductive tract.". Obstet Gynecol Surv 51 (5): 314-23. PMID 8744416.
- ↑ Arias-Stella, J. (Jan 2002). "The Arias-Stella reaction: facts and fancies four decades after.". Adv Anat Pathol 9 (1): 12-23. PMID 11756756.
- ↑ 14.0 14.1 Tawfik, O.; Venuti, S.; Brown, S.; Collins, J. (1996). "Immunohistochemical characterization of leukocytic subpopulations in chronic endometritis.". Infect Dis Obstet Gynecol 4 (5): 287-93. doi:10.1155/S1064744996000555. PMC 2364507. PMID 18476109. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2364507/.
- ↑ URL: http://www.surgpath4u.com/caseviewer.php?case_no=382. Accessed on: 9 May 2013.
- ↑ Sherman, ME.; Ronnett, BM.; Ioffe, OB.; Richesson, DA.; Rush, BB.; Glass, AG.; Chatterjee, N.; Duggan, MA. et al. (Jul 2008). "Reproducibility of biopsy diagnoses of endometrial hyperplasia: evidence supporting a simplified classification.". Int J Gynecol Pathol 27 (3): 318-25. doi:10.1097/PGP.0b013e3181659167. PMID 18580308.
- ↑ 17.0 17.1 Ely, JW.; Kennedy, CM.; Clark, EC.; Bowdler, NC.. "Abnormal uterine bleeding: a management algorithm.". J Am Board Fam Med 19 (6): 590-602. PMID 17090792. http://www.jabfm.org/content/19/6/590.full.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1080 and 1082. ISBN 0-7216-0187-1.
- ↑ URL: http://www.glowm.com/index.html?p=glowm.cml/section_view&articleid=235. Accessed on: 11 December 2012.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1082. ISBN 0-7216-0187-1.
- ↑ Lu KH (April 2009). "Management of early-stage endometrial cancer". Semin. Oncol. 36 (2): 137–44. doi:10.1053/j.seminoncol.2008.12.005. PMID 19332248.