Squamous cell carcinoma of the skin
| Squamous cell carcinoma of the skin | |
|---|---|
| Diagnosis in short | |
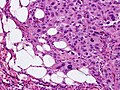
 Squamous cell carcinoma. H&E stain. | |
| Subtypes | many see squamous cell carcinoma |
| LM DDx | inverted follicular keratosis, Paget disease of the breast, eccrine carcinoma, atypical fibroxanthoma, malignant melanoma, leiomyosarcoma, basal cell carcinoma (for basaloid squamous cell carcinoma), porocarcinoma, pseudoepitheliomatous hyperplasia |
| IHC | CK5/6 +ve, p63 +ve, K903 +ve, Ber-EP4 -ve, S-100 -ve |
| Gross | scaly patch or nodule, +/-ulceration |
| Staging | squamous cell carcinoma of the skin staging |
| Site | skin - usu. sun exposed areas |
|
| |
| Associated Dx | actinic keratosis, solar elastosis |
| Clinical history | old age, +/-immunosuppression, +/-immunodeficiency |
| Prevalence | common |
| Prognosis | fairly good, may metastasize |
| Clin. DDx | other skin tumours |
Squamous cell carcinoma of the skin is a common malignant neoplasm of the skin.
It is abbreviated skin SCC, SCC of the skin, and SCC of skin.
The general topic of squamous cell carcinoma, also squamous carcinoma, is dealt with in the squamous cell carcinoma article.
General
Precursor:[1]
- Actinic keratosis (solar keratosis).
- Clinical: yellow-brown scaly, patches, sandpaper sensation.
Risk factors:[1]
- Sun exposure.
- Immune suppression (e.g. organ transplant recipients).
Notes:
- Keratoacanthoma.
- Some don't believe this entity exists.
- These people sign this entity as low grade squamous cell carcinoma, keratoacanthoma type.[2]
- Some don't believe this entity exists.
Gross
Features:[3]
- Scaly patches/nodules.
- Usu. erythematous.
- +/-Ulceration.
- "Keratin" plugs appearance.
Notes:
- Typically sun exposed areas.
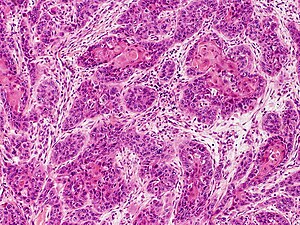
Microscopic
High risk features - for SCC of the skin:[4]
- Primary site is ear or lip.†
- Clark level IV/V = reticular dermis or deeper.
- >=2 mm thickness -- measured from granular layer (stratum granulosum) or ulcer base to deepest aspect.
- Lymphovascular invasion.
- Perineural invasion.
- Poorly differentiated.
Note:
- † The words used are "hair-bearing lip" - but there is considerable confusion about this as the AJCC manual contradicts itself.[5]
DDx:
- Inverted follicular keratosis.
- Bowen disease.
- Malignant melanoma.
- Paget disease of the breast.
- Eccrine carcinoma.
- Basal cell carcinoma for basaloid squamous cell carcinoma.
- Porocarcinoma.
- Pseudoepitheliomatous hyperplasia.
Grading
- G1 - well differentiated - easily recognizable as squamous, abundant keratinization.
- G2 - moderately differentiated - keratinization focal (typically limited to keratin pearls, individual cells or horn cysts).
- G3 - poorly differentiated - difficult to establish as squamous.
- G4 - undifferentiated or anaplastic.
Images
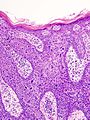
Bowen disease
Bowen disease is squamous cell carcinoma in situ of the skin.
- Its histomorphologic appearance may be similar to Paget disease of the breast/Extramammary Paget disease, Toker cell hyperplasia and melanoma.
- IHC is used to separate the entities definitively.
Histologic DDx of Bowen disease:
- Benign Toker cell hyperplasia.
- Malignant melanoma.
- Paget disease of the breast.
- Eccrine carcinoma.
Images
IHC
Bowen's disease panel:
- CK5/6 +ve.[6]
- Usu. -ve in Paget disease of the breast/Extramammary Paget disease.
- S100 -ve, HMB-45 -ve.
- Both typically +ve in melanoma.
- CEA -ve[7] (+ve in Paget disease of the breast/Extramammary Paget disease, -ve in Toker cells).
- CK7 -ve.
- Toker cells CK7 +ve.[8]
Others:
Staging
Tumour stage
| T stage | Criteria | Comment |
|---|---|---|
| T1 | <=2 cm and less than two high-risk factors | see microscopic for list of high-risk factors |
| T2 | >2 cm and less than two high-risk factors or two or more high-risk factors | see microscopic for list of high-risk factors |
| T3 | tumour into nearby bone - maxilla, mandible, orbit, temporal bone | uncommonly seen by pathology |
| T4 | tumour into axial skeleton or appendicular skeleton or perineural invasion of skull base | basically never seen by pathology |
Sign-out
Invasive SCC - small
Scalp Lesion, Excision: - INVASIVE SQUAMOUS CELL CARCINOMA, well-differentiated. -- Margins NEGATIVE for carcinoma in situ and NEGATIVE for malignancy. --- Closest margin (deep margin): 4 mm. -- Maximal tumour dimension: 1.2 cm. -- NEGATIVE for lymphovascular invasion. -- NEGATIVE for perineural invasion. - Extensive solar elastosis.
Invasive SCC - large
Skin Lesion, Mid-Back, Excision: - Invasive SQUAMOUS CELL CARCINOMA, moderately differentiated. - Margins NEGATIVE for carcinoma in situ and NEGATIVE for malignancy. -- Closest margin: > 10 mm. -- TNM stage: pT2 pN0. - Extensive solar elastosis. - Two benign lymph nodes (0/2). - Please see synoptic report.
Block letters
SKIN, SITE, BIOPSY: - MODERATELY-DIFFERENTIATED INVASIVE SQUAMOUS CELL CARCINOMA, SEE COMMENT. - NEGATIVE FOR LYMPHOVASCULAR INVASION. - NEGATIVE FOR PERINEURAL INVASION. COMMENT: The nearest margin (lateral margin) is 1 mm. The tumour is 9 mm in maximal dimension.
SKIN LESION, SITE, EXCISION: - INVASIVE SQUAMOUS CELL CARCINOMA, MODERATELY-DIFFERENTIATED. -- TUMOUR GREATEST DIMENSION: ___ CM. -- TUMOUR THICKNESS: ___ MM. -- LATERAL MARGINS: NEGATIVE FOR IN SITU CARCINOMA AND INVASIVE CARCINOMA. -- DEEP MARGIN: NEGATIVE FOR INVASIVE CARCINOMA. -- NEAREST MARGIN: 1 MM, LATERAL MARGIN. -- NEGATIVE FOR LYMPHOVASCULAR INVASION. -- NEGATIVE FOR PERINEURAL INVASION. - EXTENSIVE SOLAR ELASTOSIS.
SKIN, SITE, BIOPSY: - INVASIVE SQUAMOUS CELL CARCINOMA, SEE TUMOUR SUMMARY. TUMOUR SUMMARY: Histologic type: squamous cell carcinoma, type not otherwise specified. Histologic grade: moderately differentiated. Greatest dimension: ___ cm. Tumour thickness: ___ mm. Peripheral margin: negative for invasive carcinoma and in situ carcinoma. Deep margin (invasive component): negative for invasive carcinoma. Closest margin: deep margin, ___ mm. Lymphovascular invasion: not identified. Perineural invasion: not identified.
Bowen's disease
SKIN LESION, RIGHT EAR, BIOPSY: - SQUAMOUS CELL CARCINOMA IN SITU (BOWEN'S DISEASE), INCOMPLETELY EXCISED. COMMENT: Complete excision of the lesion is recommended.
SKIN LESION, CHEST, EXCISIONAL BIOPSY: - SQUAMOUS CELL CARCINOMA IN SITU (BOWEN'S DISEASE), COMPLETELY EXCISED. - SOLAR ELASTOSIS, MILD.
Micro
The sections show hair bearing skin. The squamous epithelium has full thickness changes including an increased nuclear-cytoplasmic ratio, loss of polarity, and nuclear hyperchromasia. Mitoses are seen in the upper third of the epithelium. Nucleoli are not apparent. No atypical cells are seen in the dermis. Parakeratosis overlies the abnormal keratinocytes. Solar elastosis is present. No melanocytic nests are identified.
Alternate
The sections show hair bearing skin. The squamous epithelium has full thickness changes including increased nuclear-cytoplasmic ratio, nuclear enlargement, loss of polarity, and nuclear hyperchromasia. Mitotic figures are easily identified.
No atypical cells are seen in the dermis; however, the epidermis is thickened. The dermal epidermal interface has a smooth contour. No paradoxical differentiation is identified. Inflammation at the dermal epidermal junction is minimal. Parakeratosis overlies the normal keratinocytes. The lesion is completely excised in the plane of section. Dermal scarring is present.
See also
References
- ↑ 1.0 1.1 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1180. ISBN 978-1416031215.
- ↑ RS. 17 May 2010.
- ↑ Stulberg, DL.; Crandell, B.; Fawcett, RS. (Oct 2004). "Diagnosis and treatment of basal cell and squamous cell carcinomas.". Am Fam Physician 70 (8): 1481-8. PMID 15526735.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/SkinSquamousCell_11protocol.pdf. Accessed on: 29 March 2012.
- ↑ Buethe, D.; Warner, C.; Miedler, J.; Cockerell, CJ. (2011). "Focus Issue on Squamous Cell Carcinoma: Practical Concerns Regarding the 7th Edition AJCC Staging Guidelines.". J Skin Cancer 2011: 156391. doi:10.1155/2011/156391. PMC 2990020. PMID 21151529. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2990020/.
- ↑ Pereira, TC.; Share, SM.; Magalhães, AV.; Silverman, JF. (Jan 2011). "Can we tell the site of origin of metastatic squamous cell carcinoma? An immunohistochemical tissue microarray study of 194 cases.". Appl Immunohistochem Mol Morphol 19 (1): 10-4. doi:10.1097/PAI.0b013e3181ecaf1c. PMID 20823766.
- ↑ URL: http://emedicine.medscape.com/article/1101235-workup#a0721. Accessed on: 2 September 2011.
- ↑ Nofech-Mozes, S.; Hanna, W.. "Toker cells revisited.". Breast J 15 (4): 394-8. doi:10.1111/j.1524-4741.2009.00743.x. PMID 19601945.
- ↑ Yu, L.; Galan, A.; McNiff, JM. (Oct 2009). "Caveats in BerEP4 staining to differentiate basal and squamous cell carcinoma.". J Cutan Pathol 36 (10): 1074-176. doi:10.1111/j.1600-0560.2008.01223.x. PMID 19187107.