Difference between revisions of "Peripheral nerve sheath tumours"
Jump to navigation
Jump to search
Jensflorian (talk | contribs) (→Perineurioma: pic + facts) |
Jensflorian (talk | contribs) (→Palisaded encapsulated neuroma: +pictures) |
||
| Line 95: | Line 95: | ||
*Abbreviated ''PEN''. | *Abbreviated ''PEN''. | ||
*[[AKA]] ''palisaded and encapsulated neuroma''. | *[[AKA]] ''palisaded and encapsulated neuroma''. | ||
*[[AKA]] ''solitary circumscribed neuroma''. | |||
===General=== | ===General=== | ||
*Flesh-colour [[papule]] - classically on the face.<ref name=Ref_Derm536>{{Ref Derm|536}}</ref> | *Flesh-colour [[papule]] - classically on the face.<ref name=Ref_Derm536>{{Ref Derm|536}}</ref> | ||
*Isolated finding - not associated with a systemic disease or malignancy.<ref name=pmid18718196>{{Cite journal | last1 = Newman | first1 = MD. | last2 = Milgraum | first2 = S. | title = Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor. | journal = Dermatol Online J | volume = 14 | issue = 7 | pages = 12 | month = | year = 2008 | doi = | PMID = 18718196 }}</ref> | *Isolated finding - not associated with a systemic disease or malignancy.<ref name=pmid18718196>{{Cite journal | last1 = Newman | first1 = MD. | last2 = Milgraum | first2 = S. | title = Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor. | journal = Dermatol Online J | volume = 14 | issue = 7 | pages = 12 | month = | year = 2008 | doi = | PMID = 18718196 }}</ref> | ||
*Superficial skin.<ref>S. Sade. 8 September 2011.</ref> | *Superficial skin papule.<ref>S. Sade. 8 September 2011.</ref> | ||
*It is considered hyperplastic rather than neoplastic. <ref>Rosai & Ackermann, Surgical Pathology, 10th ed. p183</ref> | |||
===Microscopic=== | ===Microscopic=== | ||
| Line 107: | Line 110: | ||
**#Not vacuolated. | **#Not vacuolated. | ||
**#Nuclei have pointy ends. | **#Nuclei have pointy ends. | ||
**#Sometimes epitheloid appearance. | |||
*Intralesional clefts. | *Intralesional clefts. | ||
**Useful to differentiate from schwannoma. | **Useful to differentiate from schwannoma. | ||
| Line 121: | Line 125: | ||
Images: | Images: | ||
*[http://dermatology.cdlib.org/147/case_presentation/pen/2.jpg PEN (cdlib.org)].<ref name=pmid18718196>{{Cite journal | last1 = Newman | first1 = MD. | last2 = Milgraum | first2 = S. | title = Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor. | journal = Dermatol Online J | volume = 14 | issue = 7 | pages = 12 | month = | year = 2008 | doi = | PMID = 18718196 }}</ref> | *[http://dermatology.cdlib.org/147/case_presentation/pen/2.jpg PEN (cdlib.org)].<ref name=pmid18718196>{{Cite journal | last1 = Newman | first1 = MD. | last2 = Milgraum | first2 = S. | title = Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor. | journal = Dermatol Online J | volume = 14 | issue = 7 | pages = 12 | month = | year = 2008 | doi = | PMID = 18718196 }}</ref> | ||
<gallery> | |||
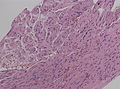
File:Palisaded_and_Encapsulated_Neuroma_(3952635881).jpg | Palisaded and encapsulated neuroma (Ed Uthman) | |||
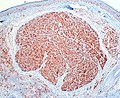
File:Palisaded_and_Encapsulated_Neuroma,_S-100_Immunostain_(3953412396).jpg| PEN, S-100 staining (Ed Uthman) | |||
</gallery> | |||
===IHC=== | ===IHC=== | ||
Revision as of 08:01, 14 December 2015
Peripheral nerve sheath tumours, abbreviated PNSTs, are common in neuropathology and occasionally show-up elsewhere. A very common PNST is the schwannoma.
Classification
A classification:[1]
- Benign:
- Malignant:
Specific diagnoses
Schwannoma
Main article: Schwannoma
Perineurioma
General
- Benign tumour derived from perineurial cells (intraneural or soft tissue).
- ICD-O 9571/0
- WHO grade I
- Rarely malignant soft tissue perineurioma.
Variant:
- Reticular perineurioma.[2]
Macroscopy
- Intraneural perineurioma: segmental tubular enlargement of the nerve.
- Soft tissue perineurioma: Well circumscribed, but not encapsulated.
Microscopic
Features:[3]
- Perineural epithelioid cells.
- Abundant pale, fluffy appearing cytoplasm.
Note:
- May be intraneural.[3]
- Typical pseudo-onion bulbs.
- Long considered hypertrophic neuropathy.
- Rare (less than 1% of all nerve sheath tumours).
DDx:
- Neuroma.
- Neurofibroma.
- Schwannoma.
- S100 +ve, EMA -ve.[3]
- Liposarcoma - reticular perineurioma.
Images:
IHC
- S100 -ve.
- EMA +ve.
- CD34 ~65% +ve.[4]
Traumatic neuroma
General
- Consequence of trauma - diagnosis requires history of trauma.
- May mimic a cancer recurrence at the site of a surgery.[6]
Microscopic
- +/-Nerve - that was injured.
- Grouping of disordered nerve fibre bundles in fibrous tissue (collagen) - key feature.
- +/-Myxoid change.
- +/-Axonal swellings (ovoid pink/purple blobs).
DDx:
- Morton neuroma (foot).
Images:
- Traumatic neuroma (nih.gov).[6]
- Traumatic neuroma - several images (upmc.edu).
- Traumatic neuroma (sarcomaimages.com).
- Traumatic neuroma (nih.gov).[8]
- Neuroma (nih.gov).[9]
Sign out
SOFT TISSUE LESION, RIGHT WRIST, EXCISION: - TRAUMATIC NEUROMA. - BENIGN FIBROADIPOSE TISSUE.
Micro
The sections show disordered nerve fibre bundles in fibrous tissue.
Palisaded encapsulated neuroma
General
- Flesh-colour papule - classically on the face.[10]
- Isolated finding - not associated with a systemic disease or malignancy.[11]
- Superficial skin papule.[12]
- It is considered hyperplastic rather than neoplastic. [13]
Microscopic
Features:[10]
- Encapsulated dermal spindle cell lesion.
- Fasciular arrangement.
- Neural-type spindle cells:
- Not vacuolated.
- Nuclei have pointy ends.
- Sometimes epitheloid appearance.
- Intralesional clefts.
- Useful to differentiate from schwannoma.
DDx:
- Schwannoma:[10]
- No intralesional clefts.
- More variability in the cellularity.
- May be deep.
Other considerations:
- Leiomyoma - cytoplasm not vacuolated, nuclei more elliptical.
Images:
IHC
Features:[11]
- S100 +ve.
- EMA +ve (capsule of lesion).
Neurofibroma
Main article: Neurofibroma
Includes discussion of plexiform neurofibroma.
Neurothekeoma
General
- Rare.
- Female > male.
Microscopic
Features:[14]
- Superficial dermal lesion:
- Usu. lobulated or micronodular architecture - key feature.
- +/-Focal sheeting.
- Spindle/epithelioid morphology with pale eosinophilic cytoplasm - key feature.
- +/-Inflammation around lesion.
- +/-Surrounded by collagen.
- Usu. lobulated or micronodular architecture - key feature.
Notes:
- No atypia.
- Mitoses rare/none.
- Often poorly circumscribed.
Subtypes:[15]
- Cellular.
- Myxoid.
- Intermediate.
DDx:
- Dermatofibroma.
- Angiomatoid fibrous histiocytoma -- have cystic blood filled spaces, inflammation.[16]
Images:
IHC
Features:[14]
- NKI/C3 (AKA NKI-C3) +ve.
- NSE +/-ve.
Others:[17]
- Vimentin +ve.
- CD10 +ve.
- Microphthalmia transcription factor +ve.
- PGP9.5 +ve.
Exclusionary:
- S100 -ve.
- Exclude other peripheral nerve sheath tumours. (???)
- Myxoid variant +ve. [citation needed]
Malignant peripheral nerve sheath tumour
Main article: Malignant peripheral nerve sheath tumour
Malignant triton tumour
- Abbreviated MTT.
- AKA malignant peripheral nerve sheath tumor with rhabdomyosarcomatous differentiation.[18]
General
- Rare.
- Considered to be a variant of MPNST.
- Prognosis worse that conventional MPNST.[18]
- Five year survival ~14%.[19]
- Diagnosis may require clinical information, i.e. individual has a history of neurofibromatosis type 1 (NF1).
Note:
- A handful of benign triton tumours are reported; these are considered neuromuscular hamartomas.[20]
Microscopic
Features - Woodruff criteria - all three required:[18]
- (a) Tumour arise from a peripheral nerve or (b) individual has NF1 or (c) lesion a metastasis arising in the context of (a) or (b).
- Schwann cell tumour characteristics.
- Rhabdomyoblasts.
- Eccentric nucleus.
- Moderate amount of eosinophilic cytoplasm.
- +/-Cross-striations.
DDx:
- Malignant peripheral nerve sheath tumour.
- Adult fibrosarcoma.
- Synovial sarcoma.
- Rhabdomyosarcoma.
- Carcinosarcoma.
IHC
Features:
- S100 +ve/-ve -- usu. focal if positive.[18]
- Leu-7 +ve/-ve.
- Myelin basic protein +ve/-ve.
Rhabdomyoblastic differentiation:[18]
- Desmin.
- Actin.
- Myogenin.
EM
- +/-Sarcomeres.[18]
Morton neuroma
Main article: Morton neuroma
See also
References
- ↑ Wippold FJ, Lubner M, Perrin RJ, Lämmle M, Perry A (October 2007). "Neuropathology for the neuroradiologist: Antoni A and Antoni B tissue patterns". AJNR Am J Neuroradiol 28 (9): 1633–8. doi:10.3174/ajnr.A0682. PMID 17893219. http://www.ajnr.org/cgi/reprint/28/9/1633.
- ↑ Graadt van Roggen, JF.; McMenamin, ME.; Belchis, DA.; Nielsen, GP.; Rosenberg, AE.; Fletcher, CD. (Apr 2001). "Reticular perineurioma: a distinctive variant of soft tissue perineurioma.". Am J Surg Pathol 25 (4): 485-93. PMID 11257623.
- ↑ Jump up to: 3.0 3.1 3.2 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Reuter, Victor E; Stoler, Mark H (2009). Sternberg's Diagnostic Surgical Pathology (5th ed.). Lippincott Williams & Wilkins. pp. 424. ISBN 978-0781779425.
- ↑ Jump up to: 4.0 4.1 Hornick, JL.; Fletcher, CD. (Jul 2005). "Soft tissue perineurioma: clinicopathologic analysis of 81 cases including those with atypical histologic features.". Am J Surg Pathol 29 (7): 845-58. PMID 15958848.
- ↑ Tsang, WY.; Chan, JK.; Chow, LT.; Tse, CC. (Aug 1992). "Perineurioma: an uncommon soft tissue neoplasm distinct from localized hypertrophic neuropathy and neurofibroma.". Am J Surg Pathol 16 (8): 756-63. PMID 1497116.
- ↑ Jump up to: 6.0 6.1 6.2 Li, Q.; Gao, EL.; Yang, YL.; Hu, HY.; Hu, XQ. (2012). "Traumatic neuroma in a patient with breast cancer after mastectomy: a case report and review of the literature.". World J Surg Oncol 10: 35. doi:10.1186/1477-7819-10-35. PMID 22330690.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 317. ISBN 978-0470519035.
- ↑ Kwon, JH.; Ryu, SW.; Kang, YN.. "Traumatic neuroma around the celiac trunk after gastrectomy mimicking a nodal metastasis: a case report.". Korean J Radiol 8 (3): 242-5. PMC 2627419. PMID 17554193. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2627419/.
- ↑ Kitcat, M.; Hunter, JE.; Malata, CM. (2009). "Sciatic neuroma presenting forty years after above-knee amputation.". Open Orthop J 3: 125-7. doi:10.2174/1874325000903010125. PMID 20224738.
- ↑ Jump up to: 10.0 10.1 10.2 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 536. ISBN 978-0443066542.
- ↑ Jump up to: 11.0 11.1 11.2 Newman, MD.; Milgraum, S. (2008). "Palisaded encapsulated neuroma (PEN): an often misdiagnosed neural tumor.". Dermatol Online J 14 (7): 12. PMID 18718196.
- ↑ S. Sade. 8 September 2011.
- ↑ Rosai & Ackermann, Surgical Pathology, 10th ed. p183
- ↑ Jump up to: 14.0 14.1 Hornick JL, Fletcher CD (March 2007). "Cellular neurothekeoma: detailed characterization in a series of 133 cases". Am. J. Surg. Pathol. 31 (3): 329–40. doi:10.1097/01.pas.0000213360.03133.89. PMID 17325474.
- ↑ Wang AR, May D, Bourne P, Scott G (November 1999). "PGP9.5: a marker for cellular neurothekeoma". Am. J. Surg. Pathol. 23 (11): 1401–7. PMID 10555009.
- ↑ URL: http://surgpathcriteria.stanford.edu/softfib/angiomatoid_fibrous_histiocytoma/. Accessed on: 11 May 2011.
- ↑ Fetsch JF, Laskin WB, Hallman JR, Lupton GP, Miettinen M (July 2007). "Neurothekeoma: an analysis of 178 tumors with detailed immunohistochemical data and long-term patient follow-up information". Am. J. Surg. Pathol. 31 (7): 1103–14. doi:10.1097/PAS.0b013e31802d96af. PMID 17592278.
- ↑ Jump up to: 18.0 18.1 18.2 18.3 18.4 18.5 Stasik, CJ.; Tawfik, O. (Dec 2006). "Malignant peripheral nerve sheath tumor with rhabdomyosarcomatous differentiation (malignant triton tumor).". Arch Pathol Lab Med 130 (12): 1878-81. doi:10.1043/1543-2165(2006)130[1878:MPNSTW]2.0.CO;2. PMID 17149968.
- ↑ McConnell, YJ.; Giacomantonio, CA. (Jan 2012). "Malignant triton tumors-complete surgical resection and adjuvant radiotherapy associated with improved survival.". J Surg Oncol. doi:10.1002/jso.23042. PMID 22253011.
- ↑ Castro, DE.; Raghuram, K.; Phillips, CD. (Apr 2005). "Benign triton tumor of the trigeminal nerve.". AJNR Am J Neuroradiol 26 (4): 967-9. PMID 15814954.
- ↑ Makki, D.; Haddad, BZ.; Mahmood, Z.; Shahid, MS.; Pathak, S.; Garnham, I. (Sep 2012). "Efficacy of corticosteroid injection versus size of plantar interdigital neuroma.". Foot Ankle Int 33 (9): 722-6. doi:DOI: 10.3113/FAI.2012.0722. PMID 22995258.