Difference between revisions of "Nephrotic syndrome"
Jump to navigation
Jump to search
(→Etiology: more) |
|||
| (27 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
'''Nephrotic syndrome''' is a constellation of clinical findings seen in a number of [[medical kidney diseases]]. This article deals with them. | '''Nephrotic syndrome''' is a constellation of clinical findings seen in a number of [[medical kidney diseases]]. This article deals with them. It should '''not''' be confused with ''[[nephritic syndrome]]'' which has an almost identical spelling. | ||
In children nephrotic syndrome is assumed to be ''minimal change disease''. Biopsies are done only there is no response to | An introduction to the medical kidney is in the ''[[medical kidney diseases]]'' article. In children nephrotic syndrome is assumed to be ''minimal change disease''. Biopsies are done only there is no response to steroids. | ||
=Clinical definition= | =Clinical definition= | ||
| Line 16: | Line 16: | ||
Immune complex positive: | Immune complex positive: | ||
#[[MN]]. | #[[MN]]. | ||
#[[IgA nephropathy]]. | #[[IgA nephropathy]].<ref name=pmid7849391>{{Cite journal | last1 = Komatsuda | first1 = A. | last2 = Wakui | first2 = H. | last3 = Yasuda | first3 = T. | last4 = Imai | first4 = H. | last5 = Miura | first5 = AB. | last6 = Tsuda | first6 = A. | last7 = Nakamoto | first7 = Y. | title = Successful delivery in a pregnant women with crescentic IgA nephropathy. | journal = Intern Med | volume = 33 | issue = 11 | pages = 723-6 | month = Nov | year = 1994 | doi = | PMID = 7849391 }}</ref><ref name=pmid22322610>{{Cite journal | last1 = Kim | first1 = JK. | last2 = Kim | first2 = JH. | last3 = Lee | first3 = SC. | last4 = Kang | first4 = EW. | last5 = Chang | first5 = TI. | last6 = Moon | first6 = SJ. | last7 = Yoon | first7 = SY. | last8 = Yoo | first8 = TH. | last9 = Kang | first9 = SW. | title = Clinical features and outcomes of IgA nephropathy with nephrotic syndrome. | journal = Clin J Am Soc Nephrol | volume = 7 | issue = 3 | pages = 427-36 | month = Mar | year = 2012 | doi = 10.2215/CJN.04820511 | PMID = 22322610 }}</ref> | ||
Other: | |||
*Pre-eclampsia.<ref name=pmid20033418>{{Cite journal | last1 = Wei | first1 = Q. | last2 = Zhang | first2 = L. | last3 = Liu | first3 = X. | title = Outcome of severe preeclampsia manifested as nephrotic syndrome. | journal = Arch Gynecol Obstet | volume = 283 | issue = 2 | pages = 201-4 | month = Feb | year = 2011 | doi = 10.1007/s00404-009-1338-z | PMID = 20033418 }}</ref> | |||
=Specific entities= | =Specific entities= | ||
| Line 30: | Line 32: | ||
Features: | Features: | ||
*No changes on light microscopy. | *No changes on light microscopy. | ||
DDx: | |||
*[[Focal segmental glomerulosclerosis]] - that is undersampled. | |||
===EM=== | ===EM=== | ||
| Line 45: | Line 50: | ||
===General=== | ===General=== | ||
*Presents as nephrotic syndrome. | *Presents as nephrotic syndrome. | ||
*Does not respond to steroids (unlike MCD). | *Does not respond to steroids (unlike [[MCD]]). | ||
*Usually less rapid onset than MCD. | |||
**Fibrosis usually takes some time. | |||
====Etiology==== | ====Etiology==== | ||
| Line 51: | Line 58: | ||
**May be familial.<ref name=pmid12778884>{{cite journal |author=Sánchez de la Nieta MD, Arias LF, Alcázar R, ''et al.'' |title=[Familial focal and segmentary hyalinosis] |language=Spanish; Castilian |journal=Nefrologia |volume=23 |issue=2 |pages=172–6 |year=2003 |pmid=12778884 |doi= |url=}}</ref> | **May be familial.<ref name=pmid12778884>{{cite journal |author=Sánchez de la Nieta MD, Arias LF, Alcázar R, ''et al.'' |title=[Familial focal and segmentary hyalinosis] |language=Spanish; Castilian |journal=Nefrologia |volume=23 |issue=2 |pages=172–6 |year=2003 |pmid=12778884 |doi= |url=}}</ref> | ||
*Secondary.<ref>URL: [http://www.kidneypathology.com/English_version/Focal_segmental_GS.html http://www.kidneypathology.com/English_version/Focal_segmental_GS.html]. Accessed on: 11 February 2011.</ref> | *Secondary.<ref>URL: [http://www.kidneypathology.com/English_version/Focal_segmental_GS.html http://www.kidneypathology.com/English_version/Focal_segmental_GS.html]. Accessed on: 11 February 2011.</ref> | ||
**HIV. | **HIV, [[parvovirus B19]].<ref name=pmid12704581/> | ||
**Drug use. | **Drug use. | ||
**Reduced renal mass. | **Reduced renal mass. | ||
| Line 87: | Line 94: | ||
*Partial sclerosis of less than 50% of glomeruli. | *Partial sclerosis of less than 50% of glomeruli. | ||
*+/-Adhesions between the glomerular tuft and Bowman's capsule. | *+/-Adhesions between the glomerular tuft and Bowman's capsule. | ||
*+/-Glomerular enlargement. | |||
DDx: | |||
*[http://library.med.utah.edu/WebPath/jpeg1/RENAL083.jpg FSGS (utah.edu)]. | *[[Minimal change disease]]. | ||
*[[C1q nephropathy]]. | |||
Images: | |||
*www: | |||
**[http://library.med.utah.edu/WebPath/jpeg1/RENAL083.jpg FSGS (utah.edu)]. | |||
*[[WC]]: | |||
**[http://commons.wikimedia.org/wiki/File:Focal_segmental_glomerulosclerosis_-_high_mag.jpg FSGS - high mag. (WC)]. | |||
**[http://commons.wikimedia.org/wiki/File:Collapsing_glomerulopathy_-_high_mag.jpg Collapsing glomerulopathy - high mag. (WC)]. | |||
**[http://commons.wikimedia.org/wiki/File:Collapsing_glomerulopathy_-_very_high_mag.jpg Collapsing glomerulopathy - very high mag. (WC)]. | |||
====Histologic classification==== | ====Histologic classification==== | ||
| Line 100: | Line 117: | ||
|abrupt severe onset | |abrupt severe onset | ||
|- | |- | ||
|Collapsing | |Collapsing ([[AKA]] collapsing glomerulopathy<ref name=pmid12704581>{{Cite journal | last1 = Schwimmer | first1 = JA. | last2 = Markowitz | first2 = GS. | last3 = Valeri | first3 = A. | last4 = Appel | first4 = GB. | title = Collapsing glomerulopathy. | journal = Semin Nephrol | volume = 23 | issue = 2 | pages = 209-18 | month = Mar | year = 2003 | doi = 10.1053/snep.2003.50019 | PMID = 12704581 }}</ref>) | ||
|poor prognosis, viral/toxic etiology | |poor prognosis, viral/toxic etiology | ||
|- | |- | ||
| Line 134: | Line 151: | ||
===General=== | ===General=== | ||
*Presents as nephrotic syndrome. | *Presents as [[nephrotic syndrome]]. | ||
*Variable course. | *Variable course. | ||
*Pathogenesis: autoantibodies directed against ''phospholipase A2 receptor 1'', abbreviated PLA2R.<ref name=pmid22388552>{{Cite journal | last1 = Glassock | first1 = RJ. | title = The pathogenesis of membranous nephropathy: evolution and revolution. | journal = Curr Opin Nephrol Hypertens | volume = | issue = | pages = | month = Mar | year = 2012 | doi = 10.1097/MNH.0b013e3283522ea8 | PMID = 22388552 }}</ref><ref name=omim604939>{{OMIM|604939}}</ref> | |||
Clinical DDx:<ref>{{Ref Klatt|241}}</ref> | Clinical DDx:<ref>{{Ref Klatt|241}}</ref> | ||
*Hepatitis B. | *[[Hepatitis B]]. | ||
*Hepatitis C. | *[[Hepatitis C]]. | ||
*Carcinoma. | *Carcinoma. | ||
*NSAID toxicity. | *[[NSAID]] toxicity. | ||
*SLE. | *[[SLE]]. | ||
*Idiopathic. | *Idiopathic. | ||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features: | ||
* | *Rigid (thickened) loop-like (glomerular) capillaries due to subepithelial immune complex deposition: | ||
**Spikes or pinholes - seen on silver stain. | **Spikes or pinholes - seen on silver stain - '''key light microscopy feature'''. | ||
**+/-Tram-tracking | **+/-Tram-tracking - seen in advanced lesions. | ||
Note: | |||
* | *Normal glomerular capillaries have a wavy wall with some undulation. | ||
*Early lesions may have an essential normal appearance on light microscopy. | |||
Lame memory device ''Oh ABCDEs'': | |||
*Nephr'''o'''tic syndrome (caused by) '''a'''utoimmune disorders, hepatitis '''B''', '''c'''ancer, '''d'''rugs (with), sub'''e'''pithelial deposits & '''s'''pikes. | |||
====Images==== | |||
www: | |||
*[http://www.flickr.com/photos/jian-hua_qiao_md/3989875091/in/set-72157622411941607 MN - silver stain (flickr.com)]. | *[http://www.flickr.com/photos/jian-hua_qiao_md/3989875091/in/set-72157622411941607 MN - silver stain (flickr.com)]. | ||
<gallery> | |||
Image:Membranous_nephropathy_-_he_-_very_high_mag.jpg | MN - very high mag. (WC) | |||
Image:Membranous_nephropathy_-_pas_-_very_high_mag.jpg | MN - PAS - very high mag. (WC) | |||
Image:Membranous_nephropathy_-_mpas_-_very_high_mag.jpg | MN - MPAS - very high mag. (WC) | |||
Image:Membranous_nephropathy_-_cropped_-_mpas_-_very_high_mag.jpg | MN - MPAS - very high mag. (WC) | |||
</gallery> | |||
===IF=== | ===IF=== | ||
| Line 161: | Line 191: | ||
===EM=== | ===EM=== | ||
*Diffuse subepithelial deposits - spike forming. | *Diffuse subepithelial deposits - spike forming. | ||
**The size of the deposits measured perpendicular to the basement membrane is smaller than seen in [[post-infectious glomerulonephritis]] (PIGN), and more diffuse. In other words, MN has a thin band-like deposits. PIGN has scattered tombstone-like ones. | |||
Image: | |||
*[http://missinglink.ucsf.edu/lm/IDS_102_cases_glomerular/images/membranous_EM.jpg MN (ucsf.edu)].<ref>URL: [http://missinglink.ucsf.edu/lm/IDS_102_cases_glomerular/Nephrotic_syndrome.htm http://missinglink.ucsf.edu/lm/IDS_102_cases_glomerular/Nephrotic_syndrome.htm]. Accessed on: 2 April 2012.</ref> | |||
==C1q nephropathy== | |||
===General=== | |||
*Distinct entity<ref name=pmid3875286>{{Cite journal | last1 = Jennette | first1 = JC. | last2 = Hipp | first2 = CG. | title = C1q nephropathy: a distinct pathologic entity usually causing nephrotic syndrome. | journal = Am J Kidney Dis | volume = 6 | issue = 2 | pages = 103-10 | month = Aug | year = 1985 | doi = | PMID = 3875286 }}</ref> ''or'' a variant of [[focal segmental glomerulosclerosis]] (FSGS)<ref name=pmid12969141>{{Cite journal | last1 = Markowitz | first1 = GS. | last2 = Schwimmer | first2 = JA. | last3 = Stokes | first3 = MB. | last4 = Nasr | first4 = S. | last5 = Seigle | first5 = RL. | last6 = Valeri | first6 = AM. | last7 = D'Agati | first7 = VD. | title = C1q nephropathy: a variant of focal segmental glomerulosclerosis. | journal = Kidney Int | volume = 64 | issue = 4 | pages = 1232-40 | month = Oct | year = 2003 | doi = 10.1046/j.1523-1755.2003.00218.x | PMID = 12969141 }}</ref> -- entity is controversial.<ref>{{Cite journal | last1 = Reeves-Daniel | first1 = AM. | last2 = Iskandar | first2 = SS. | last3 = Bowden | first3 = DW. | last4 = Bostrom | first4 = MA. | last5 = Hicks | first5 = PJ. | last6 = Comeau | first6 = ME. | last7 = Langefeld | first7 = CD. | last8 = Freedman | first8 = BI. | title = Is collapsing C1q nephropathy another MYH9-associated kidney disease? A case report. | journal = Am J Kidney Dis | volume = 55 | issue = 5 | pages = e21-4 | month = May | year = 2010 | doi = 10.1053/j.ajkd.2009.10.060 | PMID = 20116156 }}</ref> | |||
*Nephrotic syndrome. | |||
*Steroid resistant - like FSGS.<ref name=pmid3875286>{{Cite journal | last1 = Jennette | first1 = JC. | last2 = Hipp | first2 = CG. | title = C1q nephropathy: a distinct pathologic entity usually causing nephrotic syndrome. | journal = Am J Kidney Dis | volume = 6 | issue = 2 | pages = 103-10 | month = Aug | year = 1985 | doi = | PMID = 3875286 }}</ref> | |||
*[[ANA]] -ve. | |||
===Microscopic=== | |||
Features: | |||
*+/-[[Focal segmental glomerulosclerosis]]. | |||
*+/-Glomeular enlargement. | |||
===IF=== | |||
*C1q +ve - '''key feature'''. | |||
=See also= | =See also= | ||
Latest revision as of 21:35, 20 August 2014
Nephrotic syndrome is a constellation of clinical findings seen in a number of medical kidney diseases. This article deals with them. It should not be confused with nephritic syndrome which has an almost identical spelling.
An introduction to the medical kidney is in the medical kidney diseases article. In children nephrotic syndrome is assumed to be minimal change disease. Biopsies are done only there is no response to steroids.
Clinical definition
Features:
- Anasarca (whole body - edema).
- Proteinuria (>3.5 g/24h).
- Hypercholesterolemia.
- Hypoalbuminemia.
Overview
Immune complex negative:
Immune complex positive:
Other:
- Pre-eclampsia.[3]
Specific entities
Minimal change disease
- Abbreviated MCD.
General
- Responds to steroids.
- Most common cause of nephrotic syndrome in children.
- Onset rapid when compared to FSGS.
- Proteinuria usually higher in FSGS.
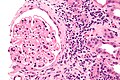
Microscopic
Features:
- No changes on light microscopy.
DDx:
- Focal segmental glomerulosclerosis - that is undersampled.
EM
Features:
- Diffuse loss of foot processes.
Note:
- Foot processes on urinary space side.
Image:
Focal segmental glomerulosclerosis
- Abbreviated FSGS.
General
- Presents as nephrotic syndrome.
- Does not respond to steroids (unlike MCD).
- Usually less rapid onset than MCD.
- Fibrosis usually takes some time.
Etiology
- Primary.
- May be familial.[4]
- Secondary.[5]
- HIV, parvovirus B19.[6]
- Drug use.
- Reduced renal mass.
| Feature | Primary | Secondary |
| Proteinuria (onset) | sudden | progressive |
| Albumnin | low | normal |
| Glomerulus size | normal | increased |
| Foot process effacement | diffuse | mild |
Notes:
- Primary FSGS needs ~70-80% foot process effacement.[7]
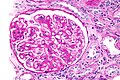
Microscopic
Features:
- Partial sclerosis of less than 50% of glomeruli.
- +/-Adhesions between the glomerular tuft and Bowman's capsule.
- +/-Glomerular enlargement.
DDx:
Images:
- www:
- WC:
Histologic classification
FSGS can be subdivided into the following subgroups:[9]
| Subtype | Comment |
|---|---|
| Cellular | abrupt severe onset |
| Collapsing (AKA collapsing glomerulopathy[6]) | poor prognosis, viral/toxic etiology |
| Tip lesion | good prognosis |
| Perihilar | reduced renal mass |
| Not otherwise specified (NOS) | most common |
Stains
Features:[10]
- PAS +ve crescents.
IF
- No immune deposits.
- No IgG.
- No IgA.
Note:
- IgM, C3 - may be focally positive due to trapping.
EM
- Foot process loss.
- Secondary causes tend to have a thinner foot process width.
Membranous nephropathy
- AKA membranous glomerulonephritis.
- Abbreviated MN.
General
- Presents as nephrotic syndrome.
- Variable course.
- Pathogenesis: autoantibodies directed against phospholipase A2 receptor 1, abbreviated PLA2R.[11][12]
Clinical DDx:[13]
- Hepatitis B.
- Hepatitis C.
- Carcinoma.
- NSAID toxicity.
- SLE.
- Idiopathic.
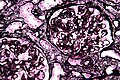
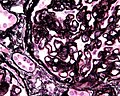
Microscopic
Features:
- Rigid (thickened) loop-like (glomerular) capillaries due to subepithelial immune complex deposition:
- Spikes or pinholes - seen on silver stain - key light microscopy feature.
- +/-Tram-tracking - seen in advanced lesions.
Note:
- Normal glomerular capillaries have a wavy wall with some undulation.
- Early lesions may have an essential normal appearance on light microscopy.
Lame memory device Oh ABCDEs:
- Nephrotic syndrome (caused by) autoimmune disorders, hepatitis B, cancer, drugs (with), subepithelial deposits & spikes.
Images
www:
IF
- Diffuse granular capillary loop - IgG, C3, kappa, lambda.
EM
- Diffuse subepithelial deposits - spike forming.
- The size of the deposits measured perpendicular to the basement membrane is smaller than seen in post-infectious glomerulonephritis (PIGN), and more diffuse. In other words, MN has a thin band-like deposits. PIGN has scattered tombstone-like ones.
Image:
C1q nephropathy
General
- Distinct entity[15] or a variant of focal segmental glomerulosclerosis (FSGS)[16] -- entity is controversial.[17]
- Nephrotic syndrome.
- Steroid resistant - like FSGS.[15]
- ANA -ve.
Microscopic
Features:
- +/-Focal segmental glomerulosclerosis.
- +/-Glomeular enlargement.
IF
- C1q +ve - key feature.
See also
References
- ↑ Komatsuda, A.; Wakui, H.; Yasuda, T.; Imai, H.; Miura, AB.; Tsuda, A.; Nakamoto, Y. (Nov 1994). "Successful delivery in a pregnant women with crescentic IgA nephropathy.". Intern Med 33 (11): 723-6. PMID 7849391.
- ↑ Kim, JK.; Kim, JH.; Lee, SC.; Kang, EW.; Chang, TI.; Moon, SJ.; Yoon, SY.; Yoo, TH. et al. (Mar 2012). "Clinical features and outcomes of IgA nephropathy with nephrotic syndrome.". Clin J Am Soc Nephrol 7 (3): 427-36. doi:10.2215/CJN.04820511. PMID 22322610.
- ↑ Wei, Q.; Zhang, L.; Liu, X. (Feb 2011). "Outcome of severe preeclampsia manifested as nephrotic syndrome.". Arch Gynecol Obstet 283 (2): 201-4. doi:10.1007/s00404-009-1338-z. PMID 20033418.
- ↑ Sánchez de la Nieta MD, Arias LF, Alcázar R, et al. (2003). "[Familial focal and segmentary hyalinosis]" (in Spanish; Castilian). Nefrologia 23 (2): 172–6. PMID 12778884.
- ↑ URL: http://www.kidneypathology.com/English_version/Focal_segmental_GS.html. Accessed on: 11 February 2011.
- ↑ 6.0 6.1 Schwimmer, JA.; Markowitz, GS.; Valeri, A.; Appel, GB. (Mar 2003). "Collapsing glomerulopathy.". Semin Nephrol 23 (2): 209-18. doi:10.1053/snep.2003.50019. PMID 12704581.
- ↑ 7.0 7.1 D'Agati, V. (Mar 2003). "Pathologic classification of focal segmental glomerulosclerosis.". Semin Nephrol 23 (2): 117-34. doi:10.1053/snep.2003.50012. PMID 12704572.
Cite error: Invalid
<ref>tag; name "pmid12704572" defined multiple times with different content - ↑ Noël, LH. (1999). "Morphological features of primary focal and segmental glomerulosclerosis.". Nephrol Dial Transplant 14 Suppl 3: 53-7. PMID 10382983.
- ↑ Thomas, DB.; Franceschini, N.; Hogan, SL.; Ten Holder, S.; Jennette, CE.; Falk, RJ.; Jennette, JC. (Mar 2006). "Clinical and pathologic characteristics of focal segmental glomerulosclerosis pathologic variants.". Kidney Int 69 (5): 920-6. doi:10.1038/sj.ki.5000160. PMID 16518352.
- ↑ URL: http://www.kidneypathology.com/English_version/Focal_segmental_GS.html. Accessed on: 11 February 2011.
- ↑ Glassock, RJ. (Mar 2012). "The pathogenesis of membranous nephropathy: evolution and revolution.". Curr Opin Nephrol Hypertens. doi:10.1097/MNH.0b013e3283522ea8. PMID 22388552.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 604939
- ↑ Klatt, Edward C. (2006). Robbins and Cotran Atlas of Pathology (1st ed.). Saunders. pp. 241. ISBN 978-1416002741.
- ↑ URL: http://missinglink.ucsf.edu/lm/IDS_102_cases_glomerular/Nephrotic_syndrome.htm. Accessed on: 2 April 2012.
- ↑ 15.0 15.1 Jennette, JC.; Hipp, CG. (Aug 1985). "C1q nephropathy: a distinct pathologic entity usually causing nephrotic syndrome.". Am J Kidney Dis 6 (2): 103-10. PMID 3875286.
- ↑ Markowitz, GS.; Schwimmer, JA.; Stokes, MB.; Nasr, S.; Seigle, RL.; Valeri, AM.; D'Agati, VD. (Oct 2003). "C1q nephropathy: a variant of focal segmental glomerulosclerosis.". Kidney Int 64 (4): 1232-40. doi:10.1046/j.1523-1755.2003.00218.x. PMID 12969141.
- ↑ Reeves-Daniel, AM.; Iskandar, SS.; Bowden, DW.; Bostrom, MA.; Hicks, PJ.; Comeau, ME.; Langefeld, CD.; Freedman, BI. (May 2010). "Is collapsing C1q nephropathy another MYH9-associated kidney disease? A case report.". Am J Kidney Dis 55 (5): e21-4. doi:10.1053/j.ajkd.2009.10.060. PMID 20116156.