Difference between revisions of "Giant cell arteritis"
Jump to navigation
Jump to search
(→Sign out: +w/ gcs) |
|||
| (5 intermediate revisions by the same user not shown) | |||
| Line 55: | Line 55: | ||
==Microscopic== | ==Microscopic== | ||
Features | Features:<ref name=pmid25457237/><ref name=pmid23543964/> | ||
*Artery with intimal thickening. | *Artery with intimal thickening and luminal narrowing. | ||
*Transmural inflammatory cells. | *Transmural inflammatory cells. | ||
*Giant cells. | *Giant cells. | ||
Notes: | Notes: | ||
*Inflammation classically [[granuloma|granulomatous]] | *Inflammation classically [[granuloma|granulomatous]]; however, granulomas not required for the diagnosis! | ||
**In one series, 11 of 15 patients (73%) had giant cells.<ref name=pmid23543964>{{cite journal |authors=Roberts WC, Zafar S, Ko JM |title=Morphological features of temporal arteritis |journal=Proc (Bayl Univ Med Cent) |volume=26 |issue=2 |pages=109–15 |date=April 2013 |pmid=23543964 |pmc=3603723 |doi=10.1080/08998280.2013.11928932 |url=}}</ref> | |||
**In another series, 33 of 40 patients (83%) had giant cells on the initial biopsy.<ref name=pmid28256573>{{cite journal |authors=Maleszewski JJ, Younge BR, Fritzlen JT, Hunder GG, Goronzy JJ, Warrington KJ, Weyand CM |title=Clinical and pathological evolution of giant cell arteritis: a prospective study of follow-up temporal artery biopsies in 40 treated patients |journal=Mod Pathol |volume=30 |issue=6 |pages=788–796 |date=June 2017 |pmid=28256573 |pmc=5650068 |doi=10.1038/modpathol.2017.10 |url=}}</ref> | |||
*Often accompanied by frank destruction of the arterial wall, e.g. fibrinoid necrosis (pink anucleate arterial wall). | *Often accompanied by frank destruction of the arterial wall, e.g. fibrinoid necrosis (pink anucleate arterial wall). | ||
*Luminal narrowing is common (>85% of cases) and typical marked.<ref name=pmid23543964/> | |||
DDx: | DDx: | ||
| Line 96: | Line 98: | ||
- Consistent with temporal arteritis (medium size artery with | - Consistent with temporal arteritis (medium size artery with | ||
lymphohistocytic inflammation, giant cells, arterial wall thickening, | lymphohistocytic inflammation, giant cells, arterial wall thickening, | ||
and elastic fibre fragmentation). | |||
</pre> | </pre> | ||
| Line 158: | Line 160: | ||
The sections show a focal histocytic response with intimal thickening. Giant cells are absent. Fibrinoid necrosis is absent. Significant transmural inflammation is absent. | The sections show a focal histocytic response with intimal thickening. Giant cells are absent. Fibrinoid necrosis is absent. Significant transmural inflammation is absent. | ||
</pre> | |||
====Alternate==== | |||
<pre> | |||
Temporal Artery, Right, Biopsy: | |||
- Medium size artery with mild-to-moderate atherosclerosis, small calcifications and focal internal | |||
elastic lamina disruption, otherwise within normal limits, see comment. | |||
Comment: | |||
A negative biopsy does not rule out the possibility of giant cell (temporal) arteritis, as this may be a focal disorder. The clinical management should be dependent upon the clinical impression. | |||
</pre> | </pre> | ||
Latest revision as of 16:49, 7 June 2024
| Giant cell arteritis | |
|---|---|
| Diagnosis in short | |
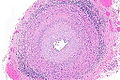
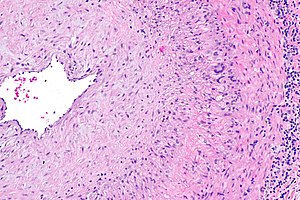 Giant cell arteritis. H&E stain. | |
|
| |
| Synonyms | temporal arteritis |
|
| |
| LM | large artery with intramural inflammatory cells (often granulomatous); intimal thickening; frank destruction of arterial wall common - fibrinoid necrosis |
| Grossing notes | temporal artery grossing |
| Site | large blood vessels - see vasculitides |
|
| |
| Clinical history | typically older than 50 years |
| Signs | loss of vision, weight loss, chills, fever |
| Symptoms | jaw claudication (classic), headache (classic), double vision, scalp tenderness |
| Prevalence | uncommon |
| Blood work | ESR elevated |
| Radiology | halo sign |
| Prognosis | good if treated |
| Clin. DDx | other causes of headache |
| Treatment | steroids |
Giant cell arteritis (abbreviated GCA), also known as temporal arteritis, is a type of large vessel vasculitis.
General
- Classically afflicts the temporal artery.
Clinical features:
- Classic finding: jaw claudication, typically in a patient older than 50 years.
- Other findings: headache (very common),[1] vision loss or diplopia, scalp tenderness, polymyalgia, weight loss, chills, fever.
Work-up:
- CRP, ESR, temporal artery biopsy.
- ESR normal (>50 years old): <20 mm/hr males, <30 mm/hr females.[2]
Treatment:
- Treat right away with high dose steroids.
- Biopsy is confirmatory and is still diagnostic if done <7-10 days after treatment starts.[3]
Gross
- Recommended length of artery >20 mm.[4]
Notes:
- Radiology: halo sign (on ultrasound); sensitivity 86% and specificity 78%.[5]
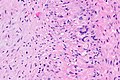
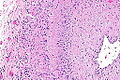
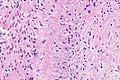
Microscopic
- Artery with intimal thickening and luminal narrowing.
- Transmural inflammatory cells.
- Giant cells.
Notes:
- Inflammation classically granulomatous; however, granulomas not required for the diagnosis!
- Often accompanied by frank destruction of the arterial wall, e.g. fibrinoid necrosis (pink anucleate arterial wall).
- Luminal narrowing is common (>85% of cases) and typical marked.[6]
DDx:
- Atherosclerosis.
- Takayasu arteritis - can be overlapping with GCA.
- Aneurysm.
- Amyloidosis.
- Granulomatosis with polyangiitis - Wegener Granulomatosis.
- Polyarteritis nodosa.
Images
www:
Sign out
Note:
- The evidence is weak that the biopsy result influences management; a negative biopsy doesn't preclude treatment for clinically presumed giant cell arteritis.[8]
Positive with giant cells
Left Temporal Artery, Biopsy:
- Consistent with temporal arteritis (medium size artery with
lymphohistocytic inflammation, giant cells, arterial wall thickening,
and elastic fibre fragmentation).
Positive
Left Temporal Artery, Biopsy:
- Consistent with temporal arteritis (medium size artery with
lymphohistocytic inflammation, arterial wall thickening, and
elastic fibre fragmentation).
Comment:
Giant cells are not seen. The findings should be correlated with the clinical impression.
Neutrophilic
Left Temporal Artery, Biopsy:
- Consistent with temporal arteritis (medium size artery with
neutrophilic inflammation, fibrioid necrosis, and
elastic fibre fragmentation).
Comment:
Giant cells are not seen.
Minimal findings - positive
Left Temporal Artery, Biopsy:
- Medium size artery with minimal lymphohistocytic inflammation
without definite giant cells or arterial wall thickening, see comment.
Comment:
The biopsy is suggestive of temporal arteritis that is either (1) early/poorly developed from a histomorphological perspective or (2) under-appreciated due to sampling.
The findings should be correlated with the clinical impression. The
management should be dependent upon the clinical impression.
Negative with atherosclerosis
Temporal Artery, Left, Biopsy: - Medium size artery with mild-to-moderate atherosclerosis, otherwise within normal limits, see comment. Comment: A negative biopsy does not rule out the possibility of giant cell (temporal) arteritis, as this may be a focal disorder. The clinical management should be dependent upon the clinical impression.
Alternate
Temporal Artery, Left, Biopsy:
- Medium size artery with moderate-to-severe atherosclerosis, otherwise
within normal limits, see comment.
Comment:
A negative biopsy does not rule out the possibility of giant cell (temporal)
arteritis, as this may be a focal disorder. The clinical management should be
dependent upon the clinical impression.
The sections show a focal histocytic response with intimal thickening. Giant cells are absent. Fibrinoid necrosis is absent. Significant transmural inflammation is absent.
Alternate
Temporal Artery, Right, Biopsy: - Medium size artery with mild-to-moderate atherosclerosis, small calcifications and focal internal elastic lamina disruption, otherwise within normal limits, see comment. Comment: A negative biopsy does not rule out the possibility of giant cell (temporal) arteritis, as this may be a focal disorder. The clinical management should be dependent upon the clinical impression.
Negative
Temporal Artery, Left, Biopsy: - Medium size artery without pathologic diagnosis, see comment. Comment: A negative biopsy does not rule out the possibility of giant cell (temporal) arteritis, as this may be a focal disorder. The clinical management should be dependent upon the clinical impression.
Block letters
TEMPORAL ARTERY, LEFT, BIOPSY: - MEDIUM SIZE ARTERY WITHOUT PATHOLOGIC DIAGNOSIS, SEE COMMENT. COMMENT: A negative biopsy does not rule out the possibility of giant cell (temporal) arteritis, as this may be a focal disorder. The clinical management should be dependent upon the clinical impression.
See also
References
- ↑ 1.0 1.1 Le, K.; Bools, LM.; Lynn, AB.; Clancy, TV.; Hooks, WB.; Hope, WW. (Oct 2014). "The effect of temporal artery biopsy on the treatment of temporal arteritis.". Am J Surg. doi:10.1016/j.amjsurg.2014.07.007. PMID 25457237.
- ↑ URL: http://www.nlm.nih.gov/medlineplus/ency/article/003638.htm. Accessed on: 17 August 2012.
- ↑ Weinberg, DA.; Savino, PJ.; Sergott, RC.; Bosley, TM. (Jul 1994). "Giant cell arteritis. Corticosteroids, temporal artery biopsy, and blindness.". Arch Fam Med 3 (7): 623-7. PMID 7921300.
- ↑ Sharma, NS.; Ooi, JL.; McGarity, BH.; Vollmer-Conna, U.; McCluskey, P. (Jun 2007). "The length of superficial temporal artery biopsies.". ANZ J Surg 77 (6): 437-9. doi:10.1111/j.1445-2197.2007.04090.x. PMID 17501882.
- ↑ Nesher G, Shemesh D, Mates M, Sonnenblick M, Abramowitz HB (June 2002). "The predictive value of the halo sign in color Doppler ultrasonography of the temporal arteries for diagnosing giant cell arteritis". J Rheumatol 29 (6): 1224–6. PMID 12064840.
- ↑ 6.0 6.1 6.2 Roberts WC, Zafar S, Ko JM (April 2013). "Morphological features of temporal arteritis". Proc (Bayl Univ Med Cent) 26 (2): 109–15. doi:10.1080/08998280.2013.11928932. PMC 3603723. PMID 23543964. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3603723/.
- ↑ Maleszewski JJ, Younge BR, Fritzlen JT, Hunder GG, Goronzy JJ, Warrington KJ, Weyand CM (June 2017). "Clinical and pathological evolution of giant cell arteritis: a prospective study of follow-up temporal artery biopsies in 40 treated patients". Mod Pathol 30 (6): 788–796. doi:10.1038/modpathol.2017.10. PMC 5650068. PMID 28256573. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5650068/.
- ↑ Lenton, J.; Donnelly, R.; Nash, JR. (Jan 2006). "Does temporal artery biopsy influence the management of temporal arteritis?". QJM 99 (1): 33-6. doi:10.1093/qjmed/hci141. PMID 16287908.