Difference between revisions of "Necrosis"
(fix typo found by AC) |
|||
| (One intermediate revision by the same user not shown) | |||
| Line 1: | Line 1: | ||
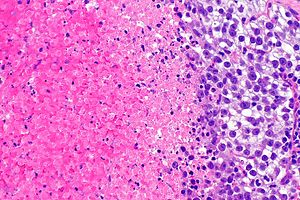
[[Image:Seminoma with necrosis -- high mag.jpg|thumb|right|Necrosis in a [[seminoma]]. [[H&E stain]].]] | [[Image:Seminoma with necrosis -- high mag.jpg|thumb|right|Necrosis (left of image) in a [[seminoma]] (right of image). [[H&E stain]].]] | ||
'''Necrosis''' is a type of cell death that is characterized by inflammation. | '''Necrosis''' is a type of cell death that is characterized by inflammation. | ||
| Line 27: | Line 27: | ||
===Other classic types=== | ===Other classic types=== | ||
*Gangrenous: coagulative necrosis in ischemic limb. | *Gangrenous: coagulative necrosis in ischemic limb. | ||
*Caseous: | *Caseous: cheesy material; [[tuberculosis]]. | ||
*Fat: adipose tissue, e.g. pancreatitis. | *Fat: adipose tissue, e.g. pancreatitis. | ||
*Fibrinoid: immune complex mediated; bright-pink in vessel walls. | *Fibrinoid: immune complex mediated; bright-pink in vessel walls. | ||
Latest revision as of 03:35, 14 July 2016
Necrosis is a type of cell death that is characterized by inflammation.
It is always pathologic. The differential diagnosis of necrosis is very broad; it is important to not be focused only on cancer and infections.
Classic types
As per Robbins:[1]
- Coagulative.
- Liquefactive.
- Gangreneous.
- Caseous.
- Fatty necrosis.
- Fibrinoid.
Coagulative
Features:[2]
- General: most common; proteinlysis > autolysis/heterolysis.
- Where/when: all tissue except the brain.
- Microscopic: cell outlines present.
Liquefactive
Features:[2]
- General: proteinlysis < autolysis/heterolysis.
- Where/when: infections, brain, abscess.
- Microscopic: nothing left; pink on H&E.
Other classic types
- Gangrenous: coagulative necrosis in ischemic limb.
- Caseous: cheesy material; tuberculosis.
- Fat: adipose tissue, e.g. pancreatitis.
- Fibrinoid: immune complex mediated; bright-pink in vessel walls.
Other types
- Cystic medial necrosis.
- Acute tubular necrosis.
- Contraction band necrosis.
- Dirty necrosis.
- Radiation necrosis.
Gross
Coagulative necrosis:
- Soft.
- Grey or white.
Liquefactive necrosis:
- Mushy, grey.
- Porridge-like consistency.
Image:
Microscopic
Features:[3]
- Dead cells - (too much pink on H&E) - one of the following:
- Anucleate cells ("Ghost cells") - outlines of cells only.
- Usually subtle.
- Fluffy appearance.
- Karyolysis - nucleus disintegrating.
- Karyorrhexis - nucleus fragmenting.
- Pyknosis - nuclear strinkage.
- Weak sign.
- Anucleate cells ("Ghost cells") - outlines of cells only.
- Inflammation - typically neutrophils (very common).
DDx of necrosis:
- Fibrin.
Notes:
- Inflammation is a reactive phenomenon; it requires blood flow.
- Post-mortem it is not found.
Images
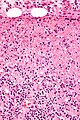
Necrosis in cat scratch disease. (WC/Nephron)
Necrosis in histiocytic necrotizing lymphadenitis. (WC/Nephron)
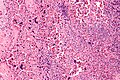
Necrosis in SLE lymphadenopathy. (WC/Nephron)
Necrotic bone. (WC/Nephron)
www:
- Necrosis at the centre of a granuloma (sun.ac.za).
- Necrosis (biomedical-engineering-online.com).
- Necrosis (nature.com).
- Necrosis (ouhsc.edu).[4]
Stains
- Martius scarlet blue stain - fibroid necrosis = red.
Sign out
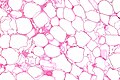
LESION, ANTERIOR RECTUS WALL, SURGICAL BIOPSY: - EXTENSIVE FAT NECROSIS. - NO EVIDENCE OF MALIGNANCY.
Micro
The sections show fibroadipose tissue with abundant foamy histiocytes and necrotic adipocytes. Scattered chronic inflammatory cells, including plasma cells eosinophils and lymphocytes, are present. Focally hemosiderin-laden macrophages are identified. Multi-nucleated giant cells are seen. No definite epithelium is identified. Some reactive fibroblasts are present. No significant nuclear atypia is identified.
See also
References
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 21-22. ISBN 0-7216-0187-1.
- ↑ 2.0 2.1 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 6. ISBN 978-1416054542.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 4. ISBN 978-1416054542.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/Com08/Com801-1-Diss.htm. Accessed on: 3 November 2010.