Difference between revisions of "Phyllodes tumour"
Jump to navigation
Jump to search
(→Sign out: update) |
|||
| (8 intermediate revisions by 2 users not shown) | |||
| Line 5: | Line 5: | ||
| Caption = Phyllodes tumour. [[H&E stain]]. | | Caption = Phyllodes tumour. [[H&E stain]]. | ||
| Synonyms = | | Synonyms = | ||
| Micro = either (1) or (2): (1) large slit-like spaces, (2) cellular stroma - may be myxoid; +/-infiltrative border, +/-mitoses, +/-nuclear atypia, +/-"stromal overgrowth" ~ stroma fills microscopic field | | Micro = either (1) or (2): (1) large slit-like spaces, (2) cellular stroma - may be myxoid; +/-infiltrative border, +/-mitoses, +/-nuclear atypia, +/-"stromal overgrowth" ~ stroma fills microscopic field (see ''microscopic'' section) | ||
| Subtypes = benign, borderline, malignant | | Subtypes = benign, borderline, malignant | ||
| LMDDx = [[fibroadenoma]], [[metaplastic breast carcinoma]], primary breast sarcoma, other [[sarcoma]]s | | LMDDx = [[fibroadenoma]], [[metaplastic breast carcinoma]], primary breast sarcoma, other [[sarcoma]]s | ||
| Line 32: | Line 32: | ||
'''Phyllodes tumour''' is a tumour of the intralobular breast stroma. It may be benign or [[malignant]]. | '''Phyllodes tumour''' is a tumour of the intralobular breast stroma. It may be benign or [[malignant]]. | ||
It was previously called '''cystosarcoma phyllodes'''. | It was previously called '''cystosarcoma phyllodes'''. It is a type of [[fibroepithelial tumours of the breast|fibroepithelial tumour]]. | ||
==General== | ==General== | ||
| Line 59: | Line 59: | ||
*+/-Mitoses. | *+/-Mitoses. | ||
*+/-Nuclear atypia. | *+/-Nuclear atypia. | ||
*+/-"Stromal overgrowth" ~ stroma fills microscopic field. | *+/-"Stromal overgrowth" ~ stroma fills microscopic field (see below). | ||
Notes: | Notes: | ||
| Line 77: | Line 77: | ||
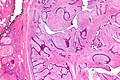
Image:Phyllodes_tumour_-_very_low_mag.jpg | Phyllodes tumour - very low mag. (WC/Nephron) | Image:Phyllodes_tumour_-_very_low_mag.jpg | Phyllodes tumour - very low mag. (WC/Nephron) | ||
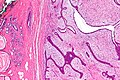
Image:Phyllodes_tumour_-_low_mag.jpg | Phyllodes tumour - low mag. (WC/Nephron) | Image:Phyllodes_tumour_-_low_mag.jpg | Phyllodes tumour - low mag. (WC/Nephron) | ||
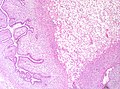
Image:Malignant phyllodes tumour.jpg |Malignant phyllodes tumour - low mag (WC) | |||
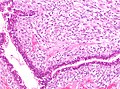
Image:Malignant phyllodes tumour high magnification.jpg |Malignant phyllodes tumour - high mag (WC) | |||
</gallery> | </gallery> | ||
| Line 127: | Line 129: | ||
* † Stromal overgrowth = epithelial elements absent in one low power field (LPF), defined as x40;<ref name=pmid17932112>{{cite journal |author=Taira N, Takabatake D, Aogi K, ''et al'' |title=Phyllodes tumor of the breast: stromal overgrowth and histological classification are useful prognosis-predictive factors for local recurrence in patients with a positive surgical margin |journal=Jpn. J. Clin. Oncol. |volume=37 |issue=10 |pages=730-6 |year=2007 |month=October |pmid=17932112 |doi=10.1093/jjco/hym099 |url=http://jjco.oxfordjournals.org/cgi/reprint/37/10/730}}</ref> ''LPF'' is not adequately defined - see [[LPFitis]]. | * † Stromal overgrowth = epithelial elements absent in one low power field (LPF), defined as x40;<ref name=pmid17932112>{{cite journal |author=Taira N, Takabatake D, Aogi K, ''et al'' |title=Phyllodes tumor of the breast: stromal overgrowth and histological classification are useful prognosis-predictive factors for local recurrence in patients with a positive surgical margin |journal=Jpn. J. Clin. Oncol. |volume=37 |issue=10 |pages=730-6 |year=2007 |month=October |pmid=17932112 |doi=10.1093/jjco/hym099 |url=http://jjco.oxfordjournals.org/cgi/reprint/37/10/730}}</ref> ''LPF'' is not adequately defined - see [[LPFitis]]. | ||
* ‡ ''HPF'' is not adequately defined - see [[HPFitis]]. | * ‡ ''HPF'' is not adequately defined - see [[HPFitis]]. | ||
==Sign out== | |||
===Benign=== | |||
<pre> | |||
Right Breast Mass, Excision: | |||
- Benign phyllodes tumour. | |||
- NEGATIVE for malignancy. | |||
</pre> | |||
====Micro==== | |||
The sections show a well-circumscribed mass with a leaf-like architecture. There is no stromal overgrowth or atypia. Proliferative activity is not readily apparent. | |||
==See also== | ==See also== | ||
Latest revision as of 19:59, 21 October 2021
| Phyllodes tumour | |
|---|---|
| Diagnosis in short | |
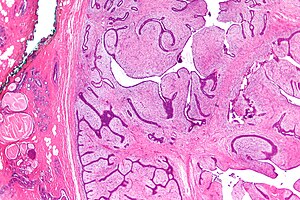 Phyllodes tumour. H&E stain. | |
|
| |
| LM | either (1) or (2): (1) large slit-like spaces, (2) cellular stroma - may be myxoid; +/-infiltrative border, +/-mitoses, +/-nuclear atypia, +/-"stromal overgrowth" ~ stroma fills microscopic field (see microscopic section) |
| Subtypes | benign, borderline, malignant |
| LM DDx | fibroadenoma, metaplastic breast carcinoma, primary breast sarcoma, other sarcomas |
| Gross | mass with clefts - leaf-like structures |
| Site | breast |
|
| |
| Signs | mass lesion |
| Prevalence | uncommon |
| Prognosis | usually benign, may be malignant |
| Clin. DDx | other breast tumours - often fibroadenoma |
| Treatment | wide excision |
Phyllodes tumour is a tumour of the intralobular breast stroma. It may be benign or malignant.
It was previously called cystosarcoma phyllodes. It is a type of fibroepithelial tumour.
General
- The name comes from the word "leaf".
- With imagination or psychotropic drugs, it may look like one: the epithelial component = the veins of the leaf.
- Wide excision -- this differs from fibroadenoma (just local excision).
- Approximately 6% are malignant.[1]
Notes:
- There are case reports of phyllodes tumours in the prostate gland.[2]
- Outside of the breast a phyllodes-like histomorphology may represent an adenosarcoma.[3]
Gross
- Clefts/leaf-like structures.
- Friable - especially vis-à-vis a fibroadenoma.
Image:
Microscopic
Features - either 1, 2 or both of the following:
- Large slit-like spaces - key feature. †
- Cellular stroma - key feature. †
- May be myxoid.
- +/-Infiltrative border.
- +/-Mitoses.
- +/-Nuclear atypia.
- +/-"Stromal overgrowth" ~ stroma fills microscopic field (see below).
Notes:
- † Large slit-like spaces are required for a benign phyllodes tumour.
- Slit-like spaces may absent in a borderline phyllodes or a malignant phyllodes.
- A cellular tumour without features suggestive of malignancy and without slit-like spaces is a cellular fibroadenoma.
- Some pathologists don't believe in cellular fibroadenoma - they call everything with stromal cellularity a phyllodes tumour.[4]
DDx:
- Fibroadenoma.
- Metaplastic breast carcinoma.
- Primary breast sarcoma.
- Other sarcomas.
Images
Grading
Phyllodes tumours are graded:
- Benign.
- Borderline.
- Malignant.
Grading phyllodes tumours - based on WMSP:[5]
| Feature | Benign phyllodes | Borderline phyllodes | Malignant phyllodes |
|---|---|---|---|
| Circumscription | Well | Well | Poor |
| Stromal overgrowth † | none | none | may be present |
| Nuclear atypia | mild | mild-to-moderate | moderate-to-marked |
| Mitoses per 10 HPFs ‡ | < 5 | 5-10 | >10 |
| Heterologous elements | +/- benign | +/- benign | +/- malignant |
| DDx | fibroadenoma | benign phyllodes, malignant phyllodes | metaplastic breast carcinoma, sarcoma |
Notes:
- † Stromal overgrowth = epithelial elements absent in one low power field (LPF), defined as x40;[6] LPF is not adequately defined - see LPFitis.
- ‡ HPF is not adequately defined - see HPFitis.
Sign out
Benign
Right Breast Mass, Excision: - Benign phyllodes tumour. - NEGATIVE for malignancy.
Micro
The sections show a well-circumscribed mass with a leaf-like architecture. There is no stromal overgrowth or atypia. Proliferative activity is not readily apparent.
See also
References
- ↑ Guerrero MA, Ballard BR, Grau AM (July 2003). "Malignant phyllodes tumor of the breast: review of the literature and case report of stromal overgrowth". Surg Oncol 12 (1): 27–37. PMID 12689668. http://linkinghub.elsevier.com/retrieve/pii/S0960740403000057.
- ↑ Bannowsky, A.; Probst, A.; Dunker, H.; Loch, T. (2009). "Rare and challenging tumor entity: phyllodes tumor of the prostate.". J Oncol 2009: 241270. doi:10.1155/2009/241270. PMID 20069045.
- ↑ McCluggage, WG. (Mar 2010). "Mullerian adenosarcoma of the female genital tract.". Adv Anat Pathol 17 (2): 122-9. doi:10.1097/PAP.0b013e3181cfe732. PMID 20179434.
- ↑ URL: http://www.breastpathologyconsults.com/blog/wp-content/uploads/2011/03/FEL_poster.pdf. Accessed on: 23 February 2012.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 263. ISBN 978-0781765275.
- ↑ Taira N, Takabatake D, Aogi K, et al (October 2007). "Phyllodes tumor of the breast: stromal overgrowth and histological classification are useful prognosis-predictive factors for local recurrence in patients with a positive surgical margin". Jpn. J. Clin. Oncol. 37 (10): 730-6. doi:10.1093/jjco/hym099. PMID 17932112. http://jjco.oxfordjournals.org/cgi/reprint/37/10/730.