Difference between revisions of "Leiomyosarcoma"
Jump to navigation
Jump to search
| (12 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Cutaneous_leiomyosarcoma_-_high_mag.jpg | |||
| Width = | |||
| Caption = Leiomyosarcoma. [[H&E stain]]. | |||
| Micro = fasciclar arrangement (characteristic of smooth muscle), features of malignancy (usually need 2 of 3): † (1) nuclear atypia, (2) tumour cell necrosis, (3) mitoses - variable & definitions suffer from [[HPFitis]] | |||
| Subtypes = major: spindled leiomyosarcoma (leiomyosarcoma NOS), epithelioid leiomyosarcoma, myxoid leiomyosarcoma; minor: leiomyosarcoma with prominent intravascular growth, leiomyosarcoma with osteoclast-type cells, leiomyosarcoma with clear cells, leiomyosarcoma with xanthoma-type cells | |||
| LMDDx = [[pleomorphic undifferentiated sarcoma]], [[atypical fibroxanthoma]] (skin only), [[EBV-associated smooth muscle tumour]], [[carcinosarcoma]], [[smooth muscle tumour of uncertain malignant potential]] (STUMP), [[endometrial stromal sarcoma]], [[atypical leiomyoma]] (symplastic leiomyoma) | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = "fleshy" appearance, necrosis, large size | |||
| Grossing = | |||
| Site = [[uterus]], [[skin]], others | |||
| Assdx = | |||
| Syndromes = [[hereditary leiomyomatosis and renal cell cancer]] | |||
| Clinicalhx = | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = uncommon | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = poor | |||
| Other = | |||
| ClinDDx = | |||
}} | |||
'''Leiomyosarcoma''' is a malignant tumour of smooth muscle. It is seen in various places including the [[uterus]] and [[skin]]. | '''Leiomyosarcoma''' is a malignant tumour of smooth muscle. It is seen in various places including the [[uterus]] and [[skin]]. | ||
==General== | ==General== | ||
*Poor prognosis. | *Poor prognosis - usually. | ||
**In locally advanced/metastatic disease (arising from the uterus) the median survival is 12-14 months.<ref>{{Cite journal | last1 = Hadoux | first1 = J. | last2 = Morice | first2 = P. | last3 = Lhommé | first3 = C. | last4 = Duvillard | first4 = P. | last5 = Balleyguier | first5 = C. | last6 = Haie-Meder | first6 = C. | last7 = Gouy | first7 = S. | last8 = Uzan | first8 = C. | last9 = Mazeron | first9 = R. | title = [Uterine leiomyosarcoma: epidemiology, pathology, biology, diagnosis, prognosis and treatment]. | journal = Bull Cancer | volume = 100 | issue = 9 | pages = 903-15 | month = Sep | year = 2013 | doi = 10.1684/bdc.2013.1801 | PMID = 24004576 }}</ref> | |||
*Do not (generally) arise from leiomyomas. | *Do not (generally) arise from leiomyomas. | ||
*Often singular, i.e. one tumour; unlike [[leiomyoma]]s (which are often multiple). | *Often singular, i.e. one tumour; unlike [[leiomyoma]]s (which are often multiple). | ||
*May be a part of [[hereditary leiomyomatosis and renal cell cancer]]. | |||
Note: | |||
*''Skin leiomyosarcoma'' do so well it has been proposed to no longer refer to them as ''sarcomas''.<ref name=pmid21358302/> | |||
==Gross== | ==Gross== | ||
| Line 19: | Line 53: | ||
**Whorled look at low power. | **Whorled look at low power. | ||
**Groups of spindle cells cut peripendicular to their long axis adjacent to groups of spindle cells cut in the plane of their long axis. | **Groups of spindle cells cut peripendicular to their long axis adjacent to groups of spindle cells cut in the plane of their long axis. | ||
*Features of malignancy (need | *Features of malignancy (usually need 2 of 3): † | ||
*#Nuclear atypia. | *#Nuclear atypia. | ||
*#Tumour cell necrosis. | *#Tumour cell necrosis. | ||
| Line 25: | Line 59: | ||
*#**Zonal necrosis is suggestive of vascular cause. | *#**Zonal necrosis is suggestive of vascular cause. | ||
*#Mitoses - '''key feature''' - definitions suffer from [[HPFitis]]: | *#Mitoses - '''key feature''' - definitions suffer from [[HPFitis]]: | ||
*#*>=10 mitoses/HPF - if spindled.<ref name=Ref_GP281>{{Ref GP|281}}</ref> | *#*>=10 mitoses/10 HPF - if spindled.<ref name=Ref_GP281>{{Ref GP|281}}</ref> | ||
*#*>=5 mitoses/HPF - if epithelioid.<ref name=Ref_GP281>{{Ref GP|281}}</ref> | *#*>=5 mitoses/10 HPF - if epithelioid.<ref name=Ref_GP281>{{Ref GP|281}}</ref> | ||
*#*>=2 mitoses/HPF - if [[myxoid]].<ref name=Ref_GP281>{{Ref GP|281}}</ref> | *#*>=2 mitoses/10 HPF - if [[myxoid]].<ref name=Ref_GP281>{{Ref GP|281}}</ref> | ||
*#*>=1 mitosis/HPF - if cutaneous.<ref name=pmid21358302>{{cite journal |author=Kraft S, Fletcher CD |title=Atypical intradermal smooth muscle neoplasms: clinicopathologic analysis of 84 cases and a reappraisal of cutaneous "leiomyosarcoma" |journal=Am. J. Surg. Pathol. |volume=35 |issue=4 |pages=599–607 |year=2011 |month=April |pmid=21358302 |doi=10.1097/PAS.0b013e31820e6093 |url=}}</ref> | *#*>=1 mitosis/10 HPF - if cutaneous.<ref name=pmid21358302>{{cite journal |author=Kraft S, Fletcher CD |title=Atypical intradermal smooth muscle neoplasms: clinicopathologic analysis of 84 cases and a reappraisal of cutaneous "leiomyosarcoma" |journal=Am. J. Surg. Pathol. |volume=35 |issue=4 |pages=599–607 |year=2011 |month=April |pmid=21358302 |doi=10.1097/PAS.0b013e31820e6093 |url=}}</ref> | ||
*+/-Heterologous elements, e.g. malignant cartilage or bone.<ref name=pmid22833086>{{Cite journal | last1 = Anh Tran | first1 = T. | last2 = Holloway | first2 = RW. | title = Metastatic leiomyosarcoma of the uterus with heterologous differentiation to malignant mesenchymoma. | journal = Int J Gynecol Pathol | volume = 31 | issue = 5 | pages = 453-7 | month = Sep | year = 2012 | doi = 10.1097/PGP.0b013e318246977d | PMID = 22833086 }}</ref> | *+/-Heterologous elements, e.g. malignant cartilage or bone.<ref name=pmid22833086>{{Cite journal | last1 = Anh Tran | first1 = T. | last2 = Holloway | first2 = RW. | title = Metastatic leiomyosarcoma of the uterus with heterologous differentiation to malignant mesenchymoma. | journal = Int J Gynecol Pathol | volume = 31 | issue = 5 | pages = 453-7 | month = Sep | year = 2012 | doi = 10.1097/PGP.0b013e318246977d | PMID = 22833086 }}</ref> | ||
Notes: | Notes: | ||
*† In deep soft tissue. 1 of 3 criteria is considered enough.<ref>URL: [http://surgpathcriteria.stanford.edu/softsmoothmuscle/soft_tissue_leiomyosarcoma/differentialdiagnosis.html http://surgpathcriteria.stanford.edu/softsmoothmuscle/soft_tissue_leiomyosarcoma/differentialdiagnosis.html]. Accessed on: 10 May 2013.</ref> | |||
*Leiomyosarcoma ''de facto'' trumps other sarcomas.<ref name=pmid22833086/> | *Leiomyosarcoma ''de facto'' trumps other sarcomas.<ref name=pmid22833086/> | ||
*Mitotic rate seems to be a relatively weak predictor; modest rate may be malignant and a high rate benign.<ref name=pmid9388868>{{Cite journal | last1 = Guo | first1 = L. | last2 = Liu | first2 = T. | last3 = Huang | first3 = H. | title = [Reappraisal of the pathological criteria for uterine leiomyosarcoma]. | journal = Zhonghua Bing Li Xue Za Zhi | volume = 25 | issue = 5 | pages = 266-9 | month = Oct | year = 1996 | doi = | PMID = 9388868 }}</ref> | |||
DDx: | DDx: | ||
| Line 39: | Line 75: | ||
*[[Carcinosarcoma]]. | *[[Carcinosarcoma]]. | ||
*[[Smooth muscle tumour of uncertain malignant potential]] (STUMP). | *[[Smooth muscle tumour of uncertain malignant potential]] (STUMP). | ||
*[[Endometrial stromal sarcoma]]. | |||
*[[Atypical leiomyoma]]. | |||
===Images=== | |||
Uterine: | |||
<gallery> | |||
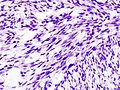
Image:Uterine_leiomyosarcoma_%281%29.jpg | Uterine leiomyosarcoma 1 (WC) | |||
Image:Uterine_leiomyosarcoma_%282%29.jpg | Uterine leiomyosarcoma 2 (WC) | |||
</gallery> | |||
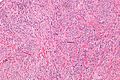
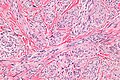
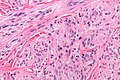
Cutaneous: | |||
<gallery> | |||
Image:Cutaneous_leiomyosarcoma_-_intermed_mag.jpg | Cutaneous leiomyosarcoma - intermed. mag. - shows fascicular pattern (WC) | |||
Image:Cutaneous_leiomyosarcoma_-_a_-_intermed_mag.jpg | Cutaneous leiomyosarcoma - intermed. mag. (WC) | |||
Image:Cutaneous_leiomyosarcoma_-_high_mag.jpg | Cutaneous leiomyosarcoma - high mag. (WC) | |||
Image:Cutaneous_leiomyosarcoma_-_very_high_mag.jpg | Cutaneous leiomyosarcoma - very high mag. (WC) | |||
</gallery> | |||
www: | |||
*[http://path.upmc.edu/cases/case107/micro.html Cutaneous leiomyosarcoma (upmc.edu)]. | |||
===Subtypes=== | ===Subtypes=== | ||
Major variants:<ref name=Ref_GP284>{{Ref GP|284}}</ref> | Major variants:<ref name=Ref_GP284>{{Ref GP|284}}</ref> | ||
| Line 92: | Line 135: | ||
*MIB1 high. | *MIB1 high. | ||
*Kertins usu. -ve -- more often +ve in epithelioid variant. | *Kertins usu. -ve -- more often +ve in epithelioid variant. | ||
==Sign out== | |||
<pre> | |||
SKIN LESION, LEFT SHOULDER (SUTURE AT 12 O'CLOCK), WIDE EXCISION: | |||
- LEIOMYOSARCOMA, MARGINALLY EXCISED. | |||
-- PLEASE SEE TUMOUR SUMMARY. | |||
- DERMAL SCAR. | |||
</pre> | |||
==See also== | ==See also== | ||
Latest revision as of 06:15, 16 October 2014
| Leiomyosarcoma | |
|---|---|
| Diagnosis in short | |
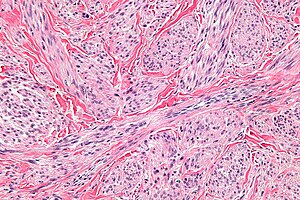 Leiomyosarcoma. H&E stain. | |
|
| |
| LM | fasciclar arrangement (characteristic of smooth muscle), features of malignancy (usually need 2 of 3): † (1) nuclear atypia, (2) tumour cell necrosis, (3) mitoses - variable & definitions suffer from HPFitis |
| Subtypes | major: spindled leiomyosarcoma (leiomyosarcoma NOS), epithelioid leiomyosarcoma, myxoid leiomyosarcoma; minor: leiomyosarcoma with prominent intravascular growth, leiomyosarcoma with osteoclast-type cells, leiomyosarcoma with clear cells, leiomyosarcoma with xanthoma-type cells |
| LM DDx | pleomorphic undifferentiated sarcoma, atypical fibroxanthoma (skin only), EBV-associated smooth muscle tumour, carcinosarcoma, smooth muscle tumour of uncertain malignant potential (STUMP), endometrial stromal sarcoma, atypical leiomyoma (symplastic leiomyoma) |
| Gross | "fleshy" appearance, necrosis, large size |
| Site | uterus, skin, others |
|
| |
| Syndromes | hereditary leiomyomatosis and renal cell cancer |
|
| |
| Prevalence | uncommon |
| Prognosis | poor |
Leiomyosarcoma is a malignant tumour of smooth muscle. It is seen in various places including the uterus and skin.
General
- Poor prognosis - usually.
- In locally advanced/metastatic disease (arising from the uterus) the median survival is 12-14 months.[1]
- Do not (generally) arise from leiomyomas.
- Often singular, i.e. one tumour; unlike leiomyomas (which are often multiple).
- May be a part of hereditary leiomyomatosis and renal cell cancer.
Note:
- Skin leiomyosarcoma do so well it has been proposed to no longer refer to them as sarcomas.[2]
Gross
Features:
- "Fleshy" appearance.
- Necrosis.
- Large size.
- Often singular, i.e. one lesion; leiomyomata are often multiple.
Microscopic
Features:
- Usually a cellular lesion.
- Fasciclar arrangement:
- Whorled look at low power.
- Groups of spindle cells cut peripendicular to their long axis adjacent to groups of spindle cells cut in the plane of their long axis.
- Features of malignancy (usually need 2 of 3): †
- Nuclear atypia.
- Tumour cell necrosis.
- Should be patchy/multifocal.
- Zonal necrosis is suggestive of vascular cause.
- Should be patchy/multifocal.
- Mitoses - key feature - definitions suffer from HPFitis:
- +/-Heterologous elements, e.g. malignant cartilage or bone.[4]
Notes:
- † In deep soft tissue. 1 of 3 criteria is considered enough.[5]
- Leiomyosarcoma de facto trumps other sarcomas.[4]
- Mitotic rate seems to be a relatively weak predictor; modest rate may be malignant and a high rate benign.[6]
DDx:
- Pleomorphic undifferentiated sarcoma.
- EBV-associated smooth muscle tumour - rare, immunoincompetent individuals.
- Carcinosarcoma.
- Smooth muscle tumour of uncertain malignant potential (STUMP).
- Endometrial stromal sarcoma.
- Atypical leiomyoma.
Images
Uterine:
Cutaneous:
www:
Subtypes
Major variants:[7]
- Spindled leiomyosarcoma (leiomyosarcoma NOS) - see above.
- Epithelioid leiomyosarcoma.
- Myxoid leiomyosarcoma.
Minor variants:[7]
- Leiomyosarcoma with prominent intravascular growth.
- Leiomyosarcoma with osteoclast-type cells.
- Leiomyosarcoma with clear cells.
- Leiomyosarcoma with xanthoma-type cells.
Epithelioid leiomyosarcoma
Features:[3]
- >50% epithelial appearance.
- >=5 mitoses/HPF - definition suffers from HPFitis.
Image:
Myxoid leiomyosarcoma
Features:[3]
- >=2 mitoses/HPF - definition suffers from HPFitis.
- May have minimal nuclear atypia.
IHC
Features:
- Positive for SMC markers.
- Desmin - present in all three types of muscle.
- H-caldesmon.
- Smooth muscle myosin.
- CD10 -ve.
- May be +ve.[7]
- Some use in the context of uterine lesions -- CD10 +ve in endometrial stromal sarcoma.
Others:[7]
- ER, PR, AR +ve -- 30-40% of the time.
- CD117 +ve/-ve.
- p53 +ve.
- MIB1 high.
- Kertins usu. -ve -- more often +ve in epithelioid variant.
Sign out
SKIN LESION, LEFT SHOULDER (SUTURE AT 12 O'CLOCK), WIDE EXCISION: - LEIOMYOSARCOMA, MARGINALLY EXCISED. -- PLEASE SEE TUMOUR SUMMARY. - DERMAL SCAR.
See also
References
- ↑ Hadoux, J.; Morice, P.; Lhommé, C.; Duvillard, P.; Balleyguier, C.; Haie-Meder, C.; Gouy, S.; Uzan, C. et al. (Sep 2013). "[Uterine leiomyosarcoma: epidemiology, pathology, biology, diagnosis, prognosis and treatment].". Bull Cancer 100 (9): 903-15. doi:10.1684/bdc.2013.1801. PMID 24004576.
- ↑ 2.0 2.1 Kraft S, Fletcher CD (April 2011). "Atypical intradermal smooth muscle neoplasms: clinicopathologic analysis of 84 cases and a reappraisal of cutaneous "leiomyosarcoma"". Am. J. Surg. Pathol. 35 (4): 599–607. doi:10.1097/PAS.0b013e31820e6093. PMID 21358302.
- ↑ 3.0 3.1 3.2 3.3 3.4 Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 281. ISBN 978-0443069208.
- ↑ 4.0 4.1 Anh Tran, T.; Holloway, RW. (Sep 2012). "Metastatic leiomyosarcoma of the uterus with heterologous differentiation to malignant mesenchymoma.". Int J Gynecol Pathol 31 (5): 453-7. doi:10.1097/PGP.0b013e318246977d. PMID 22833086.
- ↑ URL: http://surgpathcriteria.stanford.edu/softsmoothmuscle/soft_tissue_leiomyosarcoma/differentialdiagnosis.html. Accessed on: 10 May 2013.
- ↑ Guo, L.; Liu, T.; Huang, H. (Oct 1996). "[Reappraisal of the pathological criteria for uterine leiomyosarcoma].". Zhonghua Bing Li Xue Za Zhi 25 (5): 266-9. PMID 9388868.
- ↑ 7.0 7.1 7.2 7.3 Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 284. ISBN 978-0443069208.