Difference between revisions of "Vascular thrombus"
Jump to navigation
Jump to search
(+dx) |
|||
| (5 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Laminations_in_a_thrombus_-_high_mag.jpg | |||
| Width = | |||
| Caption = Thrombus with laminations. [[H&E stain]]. (WC/Nephron) | |||
| Synonyms = | |||
| Micro = layers consisting of platelets and fibrin - classically alternating with layers of RBCs (known as ''lines of Zahn'') | |||
| Subtypes = | |||
| LMDDx = tumour embolus, thromboembolus, fat embolism, amniotic fluid embolus, stasis (post-mortem) | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Staging = | |||
| Site = [[blood vessels]] | |||
| Assdx = atrial fibrillation, hypercoagulable states (e.g. cancer) | |||
| Syndromes = | |||
| Clinicalhx = | |||
| Signs = dependent on severity and location | |||
| Symptoms = | |||
| Prevalence = | |||
| Bloodwork = D-dimer +ve | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = dependent on severity, location and underlying cause (if present) | |||
| Other = | |||
| ClinDDx = | |||
| Tx = clot buster, thrombectomy, anticoagulants | |||
}} | |||
'''Vascular thrombus''' is an uncommon [[pathology]] specimen that may be from an artery or vein. | |||
''Venous thrombus'' and ''arterial thrombus'' redirect here. ''Pulmonary embolism'' is dealt with separately in the [[pulmonary embolism]] article. | |||
==General== | |||
*Uncommonly comes to [[pathology]]. | |||
Risk factors - think [[Virchow's triad]]: | |||
*Stasis, e.g. atrial fibrillation. | |||
*Hypercoagulable states, e.g. cancer - see ''[[risks factors venous thromboembolism]]''. | |||
*Endothelial injury. | |||
Clinical: | |||
*D-dimer elevated.<ref name=pmid23784703>{{Cite journal | last1 = Kleinegris | first1 = MC. | last2 = ten Cate | first2 = H. | last3 = ten Cate-Hoek | first3 = AJ. | title = D-dimer as a marker for cardiovascular and arterial thrombotic events in patients with peripheral arterial disease. A systematic review. | journal = Thromb Haemost | volume = 110 | issue = 2 | pages = 233-43 | month = Aug | year = 2013 | doi = 10.1160/TH13-01-0032 | PMID = 23784703 }}</ref> | |||
==Gross== | |||
: See ''[[pulmonary embolism]]''. | |||
Features: | |||
*Dull appearance. | |||
*Laminations. | |||
==Microscopic== | |||
Features: | |||
*Layers consisting of platelets and fibrin. | |||
**Classically alternating with layers of RBCs - known as ''Lines of Zahn''.<ref name=Ref_PBoD8_124>{{Ref PBoD8|124}}</ref> | |||
Note: | |||
*Multiple laminations (layers), in general, suggest that clot was formed in a dynamic environment, i.e. in the context of blood flow. | |||
DDx: | |||
*Tumour embolus - malignant cells. | |||
*Thromboembolus - may require [[clinical history]]. | |||
*[[Fat embolism]]. | |||
*Amniotic fluid embolus - in the context of pregnancy/postpartum. | |||
*Foreign body. | |||
===Images=== | |||
<gallery> | |||
Image:Laminations_in_a_thrombus_-_low_mag.jpg | Laminated thrombus - low mag. (WC) | |||
Image:Laminations_in_a_thrombus_-_high_mag.jpg | Laminated thrombus - high mag. (WC) | |||
</gallery> | |||
====www==== | |||
*[http://library.med.utah.edu/WebPath/ATHHTML/ATH031.html Lines of Zahn (utah.edu)]. | |||
*[http://pathhsw5m54.ucsf.edu/case9/image94.html Lines of Zahn (ucsf.edu)]. | |||
==Sign out== | |||
<pre> | |||
BLOOD CLOT, LEFT ILIAC ARTERY, THROMBECTOMY: | |||
- THROMBUS. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
<pre> | |||
BLOOD CLOT, LEFT ARM - BRACHIAL ARTERY, THROMBECTOMY/EMBOLECTOMY: | |||
- THROMBUS. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
===Micro=== | |||
The sections show layers of red blood cells alternating with fibrin and white blood cells (Lines of Zahn). | |||
==See also== | |||
*[[Cardiovascular pathology]]. | |||
*[[Ditzels]]. | |||
==References== | |||
{{Reflist|1}} | |||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
[[Category:Ditzels]] | |||
[[Category:Cardiovascular pathology]] | |||
Latest revision as of 13:10, 6 April 2016
Vascular thrombus is an uncommon pathology specimen that may be from an artery or vein.
| Vascular thrombus | |
|---|---|
| Diagnosis in short | |
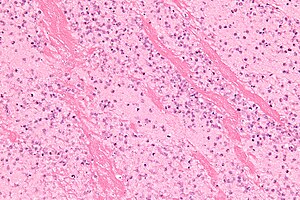 Thrombus with laminations. H&E stain. (WC/Nephron) | |
|
| |
| LM | layers consisting of platelets and fibrin - classically alternating with layers of RBCs (known as lines of Zahn) |
| LM DDx | tumour embolus, thromboembolus, fat embolism, amniotic fluid embolus, stasis (post-mortem) |
| Site | blood vessels |
|
| |
| Associated Dx | atrial fibrillation, hypercoagulable states (e.g. cancer) |
| Signs | dependent on severity and location |
| Blood work | D-dimer +ve |
| Prognosis | dependent on severity, location and underlying cause (if present) |
| Treatment | clot buster, thrombectomy, anticoagulants |
Venous thrombus and arterial thrombus redirect here. Pulmonary embolism is dealt with separately in the pulmonary embolism article.
General
- Uncommonly comes to pathology.
Risk factors - think Virchow's triad:
- Stasis, e.g. atrial fibrillation.
- Hypercoagulable states, e.g. cancer - see risks factors venous thromboembolism.
- Endothelial injury.
Clinical:
- D-dimer elevated.[1]
Gross
- See pulmonary embolism.
Features:
- Dull appearance.
- Laminations.
Microscopic
Features:
- Layers consisting of platelets and fibrin.
- Classically alternating with layers of RBCs - known as Lines of Zahn.[2]
Note:
- Multiple laminations (layers), in general, suggest that clot was formed in a dynamic environment, i.e. in the context of blood flow.
DDx:
- Tumour embolus - malignant cells.
- Thromboembolus - may require clinical history.
- Fat embolism.
- Amniotic fluid embolus - in the context of pregnancy/postpartum.
- Foreign body.
Images
www
Sign out
BLOOD CLOT, LEFT ILIAC ARTERY, THROMBECTOMY: - THROMBUS. - NEGATIVE FOR MALIGNANCY.
BLOOD CLOT, LEFT ARM - BRACHIAL ARTERY, THROMBECTOMY/EMBOLECTOMY: - THROMBUS. - NEGATIVE FOR MALIGNANCY.
Micro
The sections show layers of red blood cells alternating with fibrin and white blood cells (Lines of Zahn).
See also
References
- ↑ Kleinegris, MC.; ten Cate, H.; ten Cate-Hoek, AJ. (Aug 2013). "D-dimer as a marker for cardiovascular and arterial thrombotic events in patients with peripheral arterial disease. A systematic review.". Thromb Haemost 110 (2): 233-43. doi:10.1160/TH13-01-0032. PMID 23784703.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 124. ISBN 978-1416031215.