Difference between revisions of "Granular cell tumour"
m (→Microscopic) |
|||
| (35 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
The '''granular cell tumour''' is a rare | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | |||
| Image = Granular_cell_tumor_(3)_skin.jpg | |||
| Width = | |||
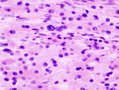
| Caption = Granular cell tumour. [[H&E stain]]. | |||
| Micro = cells (usually epithelioid) with (usually abundant) eosinophilic granular cytoplasm (granules ~ 1-3 micrometers, poorly demarcated on LM), +/-[[pseudoepitheliomatous hyperplasia]] | |||
| Subtypes = benign (common), malignant (uncommon) | |||
| LMDDx = [[squamous cell carcinoma]], [[oncocytoma]], adjacent ulcer, [[xanthoma]], [[melanocytic nevus]] with neurotization | |||
| Stains = PAS +ve | |||
| IHC = S-100 +ve, CD68 +ve (cytoplasmic), vimentin +ve (membranous), calretinin +ve (usually) | |||
| EM = abundant lysosomes | |||
| Molecular = | |||
| IF = | |||
| Gross = yellow nodule | |||
| Grossing = | |||
| Site = typically [[head and neck pathology|head and neck]] - other sites: [[breast]], [[skin]], tongue, [[esophagus]] + more | |||
| Assdx = | |||
| Syndromes = [[LEOPARD syndrome]] | |||
| Clinicalhx = | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = rare | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = usually good (benign) | |||
| Other = | |||
| ClinDDx = xanthoma, other [[skin]] lesions | |||
| Tx = complete excision (benign) or wide excision (malignant) | |||
}} | |||
The '''granular cell tumour''' is a rare histomorphologically distinctive neoplasm found at many sites. The classic location is the [[head and neck pathology|head and neck]]. | |||
==General== | ==General== | ||
*A nerve shealth tumour.<ref name=pmid22668577>{{cite journal |authors=Izquierdo F, Suárez-Vilela D, Honrado E |title=Perineurial cells in granular cell tumors and neoplasms with perineural invasion: an immunohistochemical study |journal=Am J Dermatopathol |volume=34 |issue=8 |pages=800–9 |date=December 2012 |pmid=22668577 |doi=10.1097/DAD.0b013e31824ba93b |url=}}</ref> | |||
*Rare. | *Rare. | ||
*Usually benign. | *Usually benign. | ||
*May seen in the context of ''[[LEOPARD syndrome]]'' and a mutation in the ''PTPN11 gene''.<ref name=pmid19054014>{{Cite journal | last1 = Schrader | first1 = KA. | last2 = Nelson | first2 = TN. | last3 = De Luca | first3 = A. | last4 = Huntsman | first4 = DG. | last5 = McGillivray | first5 = BC. | title = Multiple granular cell tumors are an associated feature of LEOPARD syndrome caused by mutation in PTPN11. | journal = Clin Genet | volume = 75 | issue = 2 | pages = 185-9 | month = Feb | year = 2009 | doi = 10.1111/j.1399-0004.2008.01100.x | PMID = 19054014 }}</ref> | |||
**PTPN11 = protein-tyrosine phosphatase non-receptor type 11.<ref>{{OMIM|176876}}</ref> | |||
***Gene implicated in ''[[Noonan syndrome]] 1''. | |||
*May mimic (well-differentiated) [[squamous cell carcinoma]] - histopathologically. | *May mimic (well-differentiated) [[squamous cell carcinoma]] - histopathologically. | ||
**There is a well-described phenomenon called ''pseudoepitheliomatous hyperplasia''.<ref name=pmid16487362>{{cite journal |author=Abu-Eid R, Landini G |title=Morphometrical differences between pseudoepitheliomatous hyperplasia in granular cell tumours and squamous cell carcinomas |journal=Histopathology |volume=48 |issue=4 |pages=407–16 |year=2006 |month=March |pmid=16487362 |doi=10.1111/j.1365-2559.2006.02350.x |url=}}</ref> | **There is a well-described phenomenon called ''[[pseudoepitheliomatous hyperplasia]]''.<ref name=pmid16487362>{{cite journal |author=Abu-Eid R, Landini G |title=Morphometrical differences between pseudoepitheliomatous hyperplasia in granular cell tumours and squamous cell carcinomas |journal=Histopathology |volume=48 |issue=4 |pages=407–16 |year=2006 |month=March |pmid=16487362 |doi=10.1111/j.1365-2559.2006.02350.x |url=}}</ref> | ||
Treatment: | |||
* | *Complete excision.<ref>{{cite journal |author=Toelen C, Goovaerts G, Huyghe M |title=Granular cell tumor of the abdominal wall: case report and review of the literature |journal=Acta Chir. Belg. |volume=113 |issue=5 |pages=364–6 |year=2013 |pmid=24294803 |doi= |url=}}</ref><ref>{{cite journal |author=Emesz M, Arlt EM, Krall EM, ''et al.'' |title=[Granular cell tumors of the orbit : Diagnostics and therapeutic aspects exemplified by a case report.] |journal=Ophthalmologe |volume= |issue= |pages= |year=2013 |month=November |pmid=24173669 |doi=10.1007/s00347-013-2972-1 |url=}}</ref> | ||
* | *Followup.<ref name=pmid24652564>{{cite journal |author=Paksoy M, Eken M, Ayduran E, Altin G |title=Two cases of granular cell tumors of the head and neck at different sites |journal=Ear Nose Throat J |volume=93 |issue=3 |pages=E15–7 |year=2014 |month=March |pmid=24652564 |doi= |url=}}</ref> | ||
* | |||
* | ===Sites=== | ||
* | May be seen in any number of sites: | ||
*[[Granular cell tumour of the breast]]. | |||
*Granular cell tumour of the [[skin]]. | |||
*Granular cell tumour of the tongue. | |||
*Granular cell tumour of the [[esophagus]]. | |||
==Gross== | ==Gross== | ||
*Yellow nodule. | *Yellow nodule. | ||
DDx of yellow nodule: | |||
*Granular cell tumour. | |||
*[[Lipoma]]. | |||
*[[Xanthoma]]. | |||
==Microscopic== | ==Microscopic== | ||
Features: | Features: | ||
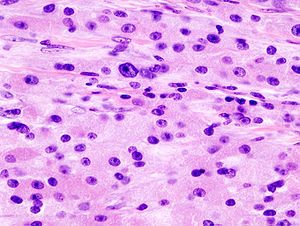
*Cells | *Cells eosinophilic or grey granular cytoplasm - '''key feature'''. | ||
**Granules: | **Cytoplasm usually abundant. | ||
**Granules (represent abundant lysosomes<ref name=pmid10410172/>): | |||
***Size: 1-3 micrometers. | ***Size: 1-3 micrometers. | ||
***Poorly demarcated. | ***Poorly demarcated (on light microscopy). | ||
*Nested architecture. | **Poorly defined cellular borders. | ||
*Nested architecture or syncytial growth pattern. | |||
*+/-Pustulo-ovoid bodies (focal eosinophilic granules surrounded by a clear halo).<ref name=pmid22760808>{{Cite journal | last1 = Fernandes | first1 = BF. | last2 = Belfort Neto | first2 = R. | last3 = Odashiro | first3 = AN. | last4 = Pereira | first4 = PR. | last5 = Burnier | first5 = MN. | title = Clinical and histopathological features of orbital granular cell tumor: case report. | journal = Arq Bras Oftalmol | volume = 75 | issue = 2 | pages = 137-9 | month = | year = | doi = | PMID = 22760808 }}</ref> | |||
*+/-Pseudoepitheliomatous hyperplasia. | |||
**May mimic [[SCC]]. | |||
DDx: | |||
*[[Squamous cell carcinoma]]. | |||
*[[Oncocytoma]]. | |||
*[[Melanocytic nevus]] with neurotization. | |||
*[[Xanthoma]]. | |||
===Malignant features=== | |||
Features of malignancy (3 of 6 required):<ref name=pmid9669341>{{cite journal |author=Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG |title=Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation |journal=Am. J. Surg. Pathol. |volume=22 |issue=7 |pages=779–94 |year=1998 |month=July |pmid=9669341 |doi= |url=}}</ref> | |||
*[[Necrosis]]. | |||
*Spindled tumour cells. | |||
*Vesciular nuclei with large [[nucleoli]]. | |||
*Mitoses (>2/10 [[HPF]] at 200x). | |||
*High [[NC ratio]]. | |||
*Pleomorphism. | |||
Predictive of poor outcome:<ref name=pmid9669341/> | |||
*Ki-67 >10%. | |||
==Special stains== | ==Special stains== | ||
*PAS +ve. | *PAS +ve. | ||
*PASD +ve (pustulo-ovoid bodies). | |||
==IHC== | ==IHC== | ||
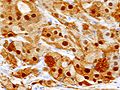
| Line 36: | Line 100: | ||
*CD68 +ve (cytoplasmic). | *CD68 +ve (cytoplasmic). | ||
*Vimentin +ve (membranous). | *Vimentin +ve (membranous). | ||
*Calretinin +ve (90-95%).<ref name=pmid12579997>{{Cite journal | last1 = Fine | first1 = SW. | last2 = Li | first2 = M. | title = Expression of calretinin and the alpha-subunit of inhibin in granular cell tumors. | journal = Am J Clin Pathol | volume = 119 | issue = 2 | pages = 259-64 | month = Feb | year = 2003 | doi = 10.1309/GRH4-JWX6-J9J7-QQTA | PMID = 12579997 }} | *Calretinin +ve (90-95%).<ref name=pmid12579997>{{Cite journal | last1 = Fine | first1 = SW. | last2 = Li | first2 = M. | title = Expression of calretinin and the alpha-subunit of inhibin in granular cell tumors. | journal = Am J Clin Pathol | volume = 119 | issue = 2 | pages = 259-64 | month = Feb | year = 2003 | doi = 10.1309/GRH4-JWX6-J9J7-QQTA | PMID = 12579997 }}</ref> | ||
</ref> | *SOX10 +ve (11 of 11 cases).<ref name=pmid37026754>{{cite journal |authors=Malik F, Bernieh A, Saad AG |title=Esophageal Granular Cell Tumor in Children: A Clinicopathologic Study of 11 Cases and Review of the Literature |journal=Am J Clin Pathol |volume=160 |issue=1 |pages=106–112 |date=July 2023 |pmid=37026754 |doi=10.1093/ajcp/aqad025 |url=}}</ref> | ||
===Images=== | |||
<gallery> | |||
Image:Granular_cell_tumor_(3)_skin.jpg | GCT. (WC) | |||
Image:Granular_cell_tumor_(4)_S-100.JPG | GCT - S-100. (WC) | |||
</gallery> | |||
==EM== | |||
*Abundant lysosomes.<ref name=pmid10410172>{{Cite journal | last1 = Ordóñez | first1 = NG. | title = Granular cell tumor: a review and update. | journal = Adv Anat Pathol | volume = 6 | issue = 4 | pages = 186-203 | month = Jul | year = 1999 | doi = | PMID = 10410172 }}</ref> | |||
**Round structures with variable (electron) density. | |||
Images: | Images: | ||
*[http:// | *[http://pathhsw5m54.ucsf.edu/cts/grancell.html Granular cell tumour - several LM and EM images (ucsf.edu)]. | ||
==Sign out== | |||
<pre> | |||
SKIN LESION, NECK, EXCISION: | |||
- GRANULAR CELL TUMOUR WITH BENIGN FEATURES, INCOMPLETELY EXCISED. | |||
COMMENT: | |||
The lesional cells stain as follows: | |||
POSITIVE: S-100, CD68, vimentin, calretinin. | |||
NEGATIVE: HMB-45. | |||
A conservative re-excision is recommended. | |||
</pre> | |||
===Micro=== | |||
The sections show skin with nests of cells in the mid dermis, extending to the subcutis. The cells that make up the nests are epithelioid and have an abundant granular grey cytoplasm, and round regular nuclei without obvious nucleoli. No mitotic activity is readily apparent. No necrosis is identified. No nuclear pleomorphism is apparent. The lesional cells focally wrap around nerve. The lesion is completely excised in the plane of section. | |||
==See also== | ==See also== | ||
Latest revision as of 19:21, 24 April 2024
| Granular cell tumour | |
|---|---|
| Diagnosis in short | |
 Granular cell tumour. H&E stain. | |
|
| |
| LM | cells (usually epithelioid) with (usually abundant) eosinophilic granular cytoplasm (granules ~ 1-3 micrometers, poorly demarcated on LM), +/-pseudoepitheliomatous hyperplasia |
| Subtypes | benign (common), malignant (uncommon) |
| LM DDx | squamous cell carcinoma, oncocytoma, adjacent ulcer, xanthoma, melanocytic nevus with neurotization |
| Stains | PAS +ve |
| IHC | S-100 +ve, CD68 +ve (cytoplasmic), vimentin +ve (membranous), calretinin +ve (usually) |
| EM | abundant lysosomes |
| Gross | yellow nodule |
| Site | typically head and neck - other sites: breast, skin, tongue, esophagus + more |
|
| |
| Syndromes | LEOPARD syndrome |
|
| |
| Prevalence | rare |
| Prognosis | usually good (benign) |
| Clin. DDx | xanthoma, other skin lesions |
| Treatment | complete excision (benign) or wide excision (malignant) |
The granular cell tumour is a rare histomorphologically distinctive neoplasm found at many sites. The classic location is the head and neck.
General
- A nerve shealth tumour.[1]
- Rare.
- Usually benign.
- May seen in the context of LEOPARD syndrome and a mutation in the PTPN11 gene.[2]
- PTPN11 = protein-tyrosine phosphatase non-receptor type 11.[3]
- Gene implicated in Noonan syndrome 1.
- PTPN11 = protein-tyrosine phosphatase non-receptor type 11.[3]
- May mimic (well-differentiated) squamous cell carcinoma - histopathologically.
- There is a well-described phenomenon called pseudoepitheliomatous hyperplasia.[4]
Treatment:
Sites
May be seen in any number of sites:
- Granular cell tumour of the breast.
- Granular cell tumour of the skin.
- Granular cell tumour of the tongue.
- Granular cell tumour of the esophagus.
Gross
- Yellow nodule.
DDx of yellow nodule:
Microscopic
Features:
- Cells eosinophilic or grey granular cytoplasm - key feature.
- Cytoplasm usually abundant.
- Granules (represent abundant lysosomes[8]):
- Size: 1-3 micrometers.
- Poorly demarcated (on light microscopy).
- Poorly defined cellular borders.
- Nested architecture or syncytial growth pattern.
- +/-Pustulo-ovoid bodies (focal eosinophilic granules surrounded by a clear halo).[9]
- +/-Pseudoepitheliomatous hyperplasia.
- May mimic SCC.
DDx:
- Squamous cell carcinoma.
- Oncocytoma.
- Melanocytic nevus with neurotization.
- Xanthoma.
Malignant features
Features of malignancy (3 of 6 required):[10]
- Necrosis.
- Spindled tumour cells.
- Vesciular nuclei with large nucleoli.
- Mitoses (>2/10 HPF at 200x).
- High NC ratio.
- Pleomorphism.
Predictive of poor outcome:[10]
- Ki-67 >10%.
Special stains
- PAS +ve.
- PASD +ve (pustulo-ovoid bodies).
IHC
Features:[11]
- S100 +ve.
- CD68 +ve (cytoplasmic).
- Vimentin +ve (membranous).
- Calretinin +ve (90-95%).[12]
- SOX10 +ve (11 of 11 cases).[13]
Images
EM
- Abundant lysosomes.[8]
- Round structures with variable (electron) density.
Images:
Sign out
SKIN LESION, NECK, EXCISION: - GRANULAR CELL TUMOUR WITH BENIGN FEATURES, INCOMPLETELY EXCISED. COMMENT: The lesional cells stain as follows: POSITIVE: S-100, CD68, vimentin, calretinin. NEGATIVE: HMB-45. A conservative re-excision is recommended.
Micro
The sections show skin with nests of cells in the mid dermis, extending to the subcutis. The cells that make up the nests are epithelioid and have an abundant granular grey cytoplasm, and round regular nuclei without obvious nucleoli. No mitotic activity is readily apparent. No necrosis is identified. No nuclear pleomorphism is apparent. The lesional cells focally wrap around nerve. The lesion is completely excised in the plane of section.
See also
References
- ↑ Izquierdo F, Suárez-Vilela D, Honrado E (December 2012). "Perineurial cells in granular cell tumors and neoplasms with perineural invasion: an immunohistochemical study". Am J Dermatopathol 34 (8): 800–9. doi:10.1097/DAD.0b013e31824ba93b. PMID 22668577.
- ↑ Schrader, KA.; Nelson, TN.; De Luca, A.; Huntsman, DG.; McGillivray, BC. (Feb 2009). "Multiple granular cell tumors are an associated feature of LEOPARD syndrome caused by mutation in PTPN11.". Clin Genet 75 (2): 185-9. doi:10.1111/j.1399-0004.2008.01100.x. PMID 19054014.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 176876
- ↑ Abu-Eid R, Landini G (March 2006). "Morphometrical differences between pseudoepitheliomatous hyperplasia in granular cell tumours and squamous cell carcinomas". Histopathology 48 (4): 407–16. doi:10.1111/j.1365-2559.2006.02350.x. PMID 16487362.
- ↑ Toelen C, Goovaerts G, Huyghe M (2013). "Granular cell tumor of the abdominal wall: case report and review of the literature". Acta Chir. Belg. 113 (5): 364–6. PMID 24294803.
- ↑ Emesz M, Arlt EM, Krall EM, et al. (November 2013). "[Granular cell tumors of the orbit : Diagnostics and therapeutic aspects exemplified by a case report.]". Ophthalmologe. doi:10.1007/s00347-013-2972-1. PMID 24173669.
- ↑ Paksoy M, Eken M, Ayduran E, Altin G (March 2014). "Two cases of granular cell tumors of the head and neck at different sites". Ear Nose Throat J 93 (3): E15–7. PMID 24652564.
- ↑ 8.0 8.1 Ordóñez, NG. (Jul 1999). "Granular cell tumor: a review and update.". Adv Anat Pathol 6 (4): 186-203. PMID 10410172.
- ↑ Fernandes, BF.; Belfort Neto, R.; Odashiro, AN.; Pereira, PR.; Burnier, MN.. "Clinical and histopathological features of orbital granular cell tumor: case report.". Arq Bras Oftalmol 75 (2): 137-9. PMID 22760808.
- ↑ 10.0 10.1 Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG (July 1998). "Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation". Am. J. Surg. Pathol. 22 (7): 779–94. PMID 9669341.
- ↑ Rekhi, B.; Jambhekar, NA. (Jun 2010). "Morphologic spectrum, immunohistochemical analysis, and clinical features of a series of granular cell tumors of soft tissues: a study from a tertiary referral cancer center.". Ann Diagn Pathol 14 (3): 162-7. doi:10.1016/j.anndiagpath.2010.01.005. PMID 20471560.
- ↑ Fine, SW.; Li, M. (Feb 2003). "Expression of calretinin and the alpha-subunit of inhibin in granular cell tumors.". Am J Clin Pathol 119 (2): 259-64. doi:10.1309/GRH4-JWX6-J9J7-QQTA. PMID 12579997.
- ↑ Malik F, Bernieh A, Saad AG (July 2023). "Esophageal Granular Cell Tumor in Children: A Clinicopathologic Study of 11 Cases and Review of the Literature". Am J Clin Pathol 160 (1): 106–112. doi:10.1093/ajcp/aqad025. PMID 37026754.