Difference between revisions of "Warthin tumour"
Jump to navigation
Jump to search
(chg name) |
|||
| (22 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Papillary_cystadenoma_lymphomatosum2.jpg | |||
| Width = | |||
| Caption = Warthin tumour. [[H&E stain]]. | |||
| Micro = papillae with a two rows of pink (eosinophilic) epithelial cells (with cuboidal basal cells and columnar luminal cells), fibrous capsule, cystic space filled with debris, lymphoid stroma | |||
| Subtypes = | |||
| LMDDx = lymphoepithelial cyst, [[oncocytoma of the salivary gland]], lymphoma associated with Warthin tumour | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = classically cystic, motor oil-like fluid | |||
| Grossing = | |||
| Site = [[salivary gland]] - parotid gland only | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = strong association with [[smoking]] | |||
| Signs = mass lesion | |||
| Symptoms = | |||
| Prevalence = common benign salivary gland lesion | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = good, benign | |||
| Other = | |||
| ClinDDx = other [[salivary gland]] tumours | |||
}} | |||
'''Warthin tumour''' is a relative common benign tumour of the parotid gland. It is also known as '''papillary cystadenoma lymphomatosum'''. | |||
==General== | |||
*Benign. | |||
Epidemiology: | |||
*May be multicentric ~ 15% of the time. | |||
*Bilateral ~6% of the time.<ref name=pmid21710045/> | |||
*Classically: male > female - changing with more women smokers. | |||
*Smokers - almost 80% of patients is a series of 70 cases.<ref name=pmid21710045>{{Cite journal | last1 = Chedid | first1 = HM. | last2 = Rapoport | first2 = A. | last3 = Aikawa | first3 = KF. | last4 = Menezes | first4 = Ados S. | last5 = Curioni | first5 = OA. | title = Warthin's tumor of the parotid gland: study of 70 cases. | journal = Rev Col Bras Cir | volume = 38 | issue = 2 | pages = 90-4 | month = | year = | doi = | PMID = 21710045 }}</ref> | |||
*Old - usually 60s,<ref>{{Cite journal | last1 = Dăguci | first1 = L. | last2 = Simionescu | first2 = C. | last3 = Stepan | first3 = A. | last4 = Munteanu | first4 = C. | last5 = Dăguci | first5 = C. | last6 = Bătăiosu | first6 = M. | title = Warthin tumor--morphological study of the stromal compartment. | journal = Rom J Morphol Embryol | volume = 52 | issue = 4 | pages = 1319-23 | month = | year = 2011 | doi = | PMID = 22203940 }} | |||
</ref> very rarely < 40 years old. | |||
Notes: | |||
*No malignant transformation. | |||
*Not in submandibular gland. | |||
*Not in sublingual gland. | |||
*Not in children. | |||
==Gross== | |||
Features: | |||
*Motor oil-like fluid.<ref name=pmid16390238 >{{Cite journal | last1 = Hunt | first1 = JL. | title = Warthin tumors do not have microsatellite instability and express normal DNA mismatch repair proteins. | journal = Arch Pathol Lab Med | volume = 130 | issue = 1 | pages = 52-6 | month = Jan | year = 2006 | doi = 10.1043/1543-2165(2006)130[52:WTDNHM]2.0.CO;2 | PMID = 16390238 }}</ref> | |||
*Cystic component larger in larger lesions. | |||
**Small lesions may be solid. | |||
Image: | |||
*[http://www.flickr.com/photos/bc_the_path/2510239905/in/photostream/ Warthin tumour (flickr.com)]. | |||
==Microscopic== | |||
Features: | |||
* Papillae (nipple-shaped structures) with a two rows of pink (eosinophilic) epithelial cells (with cuboidal basal cells and columnar luminal cells) - '''key feature'''. | |||
* Fibrous capsule - pink & homogenous on [[H&E stain]]. | |||
* Cystic space filled with debris ''in situ'' (not [[necrosis]]). | |||
* Lymphoid stroma. | |||
Notes: | |||
*+/-Squamous differentiation. | |||
*+/-Goblet cell differentiation. | |||
DDx: | |||
*Lymphoepithelial cyst. | |||
**Cyst within a lymph node. | |||
*Lymphoma associated with Warthin tumour - case reports.<ref name=pmid31183747>{{Cite journal | last1 = Alnoor | first1 = F. | last2 = Gandhi | first2 = JS. | last3 = Stein | first3 = MK. | last4 = Gradowski | first4 = JF. | title = Follicular Lymphoma Diagnosed in Warthin Tumor: A Case Report and Review of the Literature. | journal = Head Neck Pathol | volume = | issue = | pages = | month = Jun | year = 2019 | doi = 10.1007/s12105-019-01045-x | PMID = 31183747 }}</ref><ref name=pmid28978260>{{Cite journal | last1 = Jawad | first1 = H. | last2 = McCarthy | first2 = P. | last3 = O'Leary | first3 = G. | last4 = Heffron | first4 = CC. | title = Presentation of Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma in a Warthin Tumor: Case Report and Literature Review. | journal = Int J Surg Pathol | volume = 26 | issue = 3 | pages = 256-260 | month = May | year = 2018 | doi = 10.1177/1066896917734371 | PMID = 28978260 }}</ref> | |||
*[[Oncocytoma of the salivary gland]]. | |||
===Images=== | |||
====Case 1==== | |||
<gallery> | |||
Image:Papillary_cystadenoma_lymphomatosum1.jpg | Warthin tumour - low mag. (WC/Nephron) | |||
Image:Papillary_cystadenoma_lymphomatosum2.jpg | Warthin tumour - intermed. mag. (WC/Nephron) | |||
Image:Papillary_cystadenoma_lymphomatosum3.jpg | Warthin tumour - high mag. (WC/Nephron) | |||
</gallery> | |||
====Case 2==== | |||
<gallery> | |||
Image: Warthin tumor (1).jpg | Warthin tumour. (WC/KGH) | |||
Image: Warthin tumor (2).jpg | Warthin tumour. (WC/KGH) | |||
</gallery> | |||
===Sign out=== | |||
<pre> | |||
Parotid Gland, Left, Excision: | |||
- Warthin's tumour (papillary cystadenoma lymphomatosum). | |||
- NEGATIVE for malignancy. | |||
</pre> | |||
====Block letters==== | |||
<pre> | |||
PAROTID GLAND, RIGHT, EXCISION: | |||
- WARTHIN TUMOUR. | |||
</pre> | |||
====Micro==== | |||
The sections show a cystic tumour with lymphoid tissue associated with benign salivary gland tissue. The lymphoid tissue is composed of small cells and forms morphologically unremarkable follicles. The cyst-lining epithelium has a bilayered appearance and is composed of cells with abundant eosinophilic cytoplasm and nucleoli. The tumour focally extends to the edge of the tissue (ink present on tumour). | |||
==See also== | |||
*[[Salivary glands]]. | |||
*[[Head and neck pathology]]. | |||
*[[Papillary thyroid carcinoma Warthin-like variant]]. | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Diagnosis]] | |||
[[Category:Salivary gland]] | |||
[[Category:Head and neck pathology]] | |||
Latest revision as of 18:20, 10 February 2021
Warthin tumour is a relative common benign tumour of the parotid gland. It is also known as papillary cystadenoma lymphomatosum.
| Warthin tumour | |
|---|---|
| Diagnosis in short | |
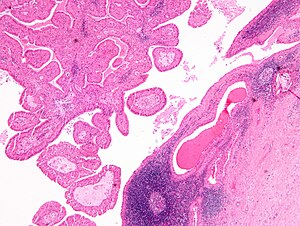 Warthin tumour. H&E stain. | |
|
| |
| LM | papillae with a two rows of pink (eosinophilic) epithelial cells (with cuboidal basal cells and columnar luminal cells), fibrous capsule, cystic space filled with debris, lymphoid stroma |
| LM DDx | lymphoepithelial cyst, oncocytoma of the salivary gland, lymphoma associated with Warthin tumour |
| Gross | classically cystic, motor oil-like fluid |
| Site | salivary gland - parotid gland only |
|
| |
| Clinical history | strong association with smoking |
| Signs | mass lesion |
| Prevalence | common benign salivary gland lesion |
| Prognosis | good, benign |
| Clin. DDx | other salivary gland tumours |
General
- Benign.
Epidemiology:
- May be multicentric ~ 15% of the time.
- Bilateral ~6% of the time.[1]
- Classically: male > female - changing with more women smokers.
- Smokers - almost 80% of patients is a series of 70 cases.[1]
- Old - usually 60s,[2] very rarely < 40 years old.
Notes:
- No malignant transformation.
- Not in submandibular gland.
- Not in sublingual gland.
- Not in children.
Gross
Features:
- Motor oil-like fluid.[3]
- Cystic component larger in larger lesions.
- Small lesions may be solid.
Image:
Microscopic
Features:
- Papillae (nipple-shaped structures) with a two rows of pink (eosinophilic) epithelial cells (with cuboidal basal cells and columnar luminal cells) - key feature.
- Fibrous capsule - pink & homogenous on H&E stain.
- Cystic space filled with debris in situ (not necrosis).
- Lymphoid stroma.
Notes:
- +/-Squamous differentiation.
- +/-Goblet cell differentiation.
DDx:
- Lymphoepithelial cyst.
- Cyst within a lymph node.
- Lymphoma associated with Warthin tumour - case reports.[4][5]
- Oncocytoma of the salivary gland.
Images
Case 1
Case 2
Sign out
Parotid Gland, Left, Excision: - Warthin's tumour (papillary cystadenoma lymphomatosum). - NEGATIVE for malignancy.
Block letters
PAROTID GLAND, RIGHT, EXCISION: - WARTHIN TUMOUR.
Micro
The sections show a cystic tumour with lymphoid tissue associated with benign salivary gland tissue. The lymphoid tissue is composed of small cells and forms morphologically unremarkable follicles. The cyst-lining epithelium has a bilayered appearance and is composed of cells with abundant eosinophilic cytoplasm and nucleoli. The tumour focally extends to the edge of the tissue (ink present on tumour).
See also
References
- ↑ 1.0 1.1 Chedid, HM.; Rapoport, A.; Aikawa, KF.; Menezes, Ados S.; Curioni, OA.. "Warthin's tumor of the parotid gland: study of 70 cases.". Rev Col Bras Cir 38 (2): 90-4. PMID 21710045.
- ↑ Dăguci, L.; Simionescu, C.; Stepan, A.; Munteanu, C.; Dăguci, C.; Bătăiosu, M. (2011). "Warthin tumor--morphological study of the stromal compartment.". Rom J Morphol Embryol 52 (4): 1319-23. PMID 22203940.
- ↑ Hunt, JL. (Jan 2006). "Warthin tumors do not have microsatellite instability and express normal DNA mismatch repair proteins.". Arch Pathol Lab Med 130 (1): 52-6. doi:10.1043/1543-2165(2006)130[52:WTDNHM]2.0.CO;2. PMID 16390238.
- ↑ Alnoor, F.; Gandhi, JS.; Stein, MK.; Gradowski, JF. (Jun 2019). "Follicular Lymphoma Diagnosed in Warthin Tumor: A Case Report and Review of the Literature.". Head Neck Pathol. doi:10.1007/s12105-019-01045-x. PMID 31183747.
- ↑ Jawad, H.; McCarthy, P.; O'Leary, G.; Heffron, CC. (May 2018). "Presentation of Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma in a Warthin Tumor: Case Report and Literature Review.". Int J Surg Pathol 26 (3): 256-260. doi:10.1177/1066896917734371. PMID 28978260.