Difference between revisions of "Steatosis"
Jump to navigation
Jump to search
(tweak) |
|||
| (One intermediate revision by the same user not shown) | |||
| Line 7: | Line 7: | ||
| Micro = fatty change (macrovesicular or microvesicular and periportal or centrilobular), negative for ballooning degeneration, negative for significant inflammation - esp. [[neutrophils]] | | Micro = fatty change (macrovesicular or microvesicular and periportal or centrilobular), negative for ballooning degeneration, negative for significant inflammation - esp. [[neutrophils]] | ||
| Subtypes = macrovesicular steatosis (periportal, centrilobular), microvesicular steatosis | | Subtypes = macrovesicular steatosis (periportal, centrilobular), microvesicular steatosis | ||
| LMDDx = [[steatohepatitis]] (ASH, | | LMDDx = [[steatohepatitis]] (ASH, MASH), [[drug-induced liver injury]] | ||
| Stains = | | Stains = | ||
| IHC = | | IHC = | ||
| Line 28: | Line 28: | ||
| Prognosis = dependent on underlying cause | | Prognosis = dependent on underlying cause | ||
| Other = | | Other = | ||
| ClinDDx = [[ASH]], [[ | | ClinDDx = [[ASH]], [[MASH]], [[drug-induced liver injury]] | ||
| Tx = dependent on underlying cause | | Tx = dependent on underlying cause | ||
}} | }} | ||
| Line 77: | Line 77: | ||
Centrilobular predominant (zone III) - ''DOA'':<ref name=pcddx_steatosis/> | Centrilobular predominant (zone III) - ''DOA'':<ref name=pcddx_steatosis/> | ||
*[[Diabetes mellitus]]. | *[[Diabetes mellitus]]. | ||
*[[Obesity]], | *[[Obesity]], metabolic dysfunction-associated steatohepatitis ([[MASH]]). | ||
*[[Alcoholic liver disease]], alcoholic steatohepatitis (ASH). | *[[Alcoholic liver disease]], alcoholic steatohepatitis (ASH). | ||
| Line 96: | Line 96: | ||
*Greasy/slippery feeling. | *Greasy/slippery feeling. | ||
*Enlarged. | *Enlarged. | ||
Note: | |||
*May be estimated on MRI by proton density fat fraction (PDFF).<ref name=pmid23382291>{{Cite journal | last1 = Tang | first1 = A. | last2 = Tan | first2 = J. | last3 = Sun | first3 = M. | last4 = Hamilton | first4 = G. | last5 = Bydder | first5 = M. | last6 = Wolfson | first6 = T. | last7 = Gamst | first7 = AC. | last8 = Middleton | first8 = M. | last9 = Brunt | first9 = EM. | title = Nonalcoholic fatty liver disease: MR imaging of liver proton density fat fraction to assess hepatic steatosis. | journal = Radiology | volume = 267 | issue = 2 | pages = 422-31 | month = May | year = 2013 | doi = 10.1148/radiol.12120896 | PMID = 23382291 }}</ref> | |||
==Microscopic== | ==Microscopic== | ||
Latest revision as of 19:22, 16 May 2024
| Steatosis | |
|---|---|
| Diagnosis in short | |
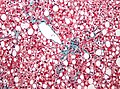
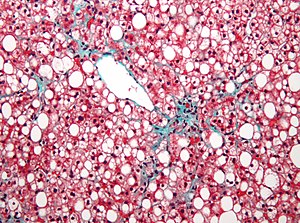 Steatosis. Elastic Masson's trichrome stain. | |
|
| |
| Synonyms | fatty liver |
|
| |
| LM | fatty change (macrovesicular or microvesicular and periportal or centrilobular), negative for ballooning degeneration, negative for significant inflammation - esp. neutrophils |
| Subtypes | macrovesicular steatosis (periportal, centrilobular), microvesicular steatosis |
| LM DDx | steatohepatitis (ASH, MASH), drug-induced liver injury |
| Gross | yellow colour, greasy/slippery feeling, enlarged |
| Site | liver - see medical liver disease |
|
| |
| Associated Dx | obesity, alcoholism |
| Prevalence | very common |
| Radiology | may be estimated by proton density fat fraction (PDFF) |
| Prognosis | dependent on underlying cause |
| Clin. DDx | ASH, MASH, drug-induced liver injury |
| Treatment | dependent on underlying cause |
Steatosis, also fatty liver, is a fatty change in the liver associated with a number of underlying (medical) causes.
General
Classification
Can be divided into:
- Macrovesicular steatosis.
- Common.
- Microvesicular steatosis.
- Rare.
- Potentially life threatening.[1]
Note:
- It is considered technically incorrect to say the liver, in steatosis/steatohepatitis, contains adipocytes; they are lipid-laden hepatocytes,[2] despite that:
- Histologically, these cells look like adipocytes.
- Lipid-laden hepatocytes have gene activations suggestive of adipogenic-like transformation.[3]
Etiology
Microvesicular steatosis
Microvesicular steatosis DDx:[4]
- Acute fatty liver of pregnancy,
- Reye's syndrome.
- Drug toxicity:
- Sodium valproate toxicity.
- High-dose tetracycline toxicity.
- Jamaican vomiting sickness.
- Congenital defects of urea cycle enzymes.
Less common causes:
- Alcoholism.
- Hepatitis D.
- Weird stuff:
- Congenital defects of fatty acid beta oxidation.
- Cholesterol ester storage disease.
- Wolman disease and Alpers syndrome.
The classic causes of microvesicular steatosis are:[5]
- Fatty liver of pregnancy.
- Aspirin (Reye's syndrome).
- Tetracycline.
It was once thought that all other causes of fatty liver produce macrovesicular steatosis.
Macrovesicular steatosis
Can sometimes be divided into centrilobular predominant and periportal predominant.[6]
Centrilobular predominant (zone III) - DOA:[6]
- Diabetes mellitus.
- Obesity, metabolic dysfunction-associated steatohepatitis (MASH).
- Alcoholic liver disease, alcoholic steatohepatitis (ASH).
Periportal predominant (zone I) - TAPES:[6]
- Total parenteral nutrition (TPN).
- AIDS.
- Phosphorus poisoning.
- Exogenous steroids.
- Starvation.[7]
Notes:
- HCV genotype 3 is reported to cause periportal steatosis.[8]
- Donor livers with more macrovescicular steatosis = worse outcome.
- More than 30% means the liver is undesirable for transplantation.[9]
Gross
- Yellow colour.
- Greasy/slippery feeling.
- Enlarged.
Note:
- May be estimated on MRI by proton density fat fraction (PDFF).[10]
Microscopic
Features - macrovesicular steatosis.
- One large vacuoles - similar to mature adipose tissue.
- Nucleus is eccentric.
Features - microvesicular steatosis.
- Multiple small (clear) cytoplasmic vacuoles - similar to brown fat, as seen in a hibernoma.
- Nucleus is central.[11]
Grading
Quantity of fat is usually given as a percentage and graded mild, moderate, or marked.
- Mild <33%, moderate >33% & <66%, marked >66%.[12]
Images
See also
References
- ↑ Jolly, RA.; Ciurlionis, R.; Morfitt, D.; Helgren, M.; Patterson, R.; Ulrich, RG.; Waring, JF.. "Microvesicular steatosis induced by a short chain fatty acid: effects on mitochondrial function and correlation with gene expression.". Toxicol Pathol 32 Suppl 2: 19-25. PMID 15503661.
- ↑ Guindi, M. September 2009.
- ↑ URL: http://www.jci.org/articles/view/20513/version/1. Accessed on: 23 September 2009.
- ↑ Hautekeete ML, Degott C, Benhamou JP (1990). "Microvesicular steatosis of the liver". Acta Clin Belg 45 (5): 311–26. PMID 2177300.
- ↑ http://www.mailman.srv.ualberta.ca/pipermail/patho-l/1996-June/001788.html
- ↑ 6.0 6.1 6.2 Steatosis. pathconsultddx.com. URL: http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675%2806%2970840-3. Accessed on: 2 Sep 2009.
- ↑ Nagy, I.; Németh, J.; Lászik, Z. (Jan 2000). "Effect of L-aminocarnitine, an inhibitor of mitochondrial fatty acid oxidation, on the exocrine pancreas and liver in fasted rats.". Pharmacol Res 41 (1): 9-17. doi:10.1006/phrs.1999.0565. PMID 10600264.
- ↑ Yoon EJ, Hu KQ. Hepatitis C virus (HCV) infection and hepatic steatosis. Int J Med Sci. 2006;3(2):53-6. Epub 2006 Apr 1. PMID 16614743. Avialable at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1415843. Accessed on: September 9, 2009.
- ↑ STC. 6 December 2010.
- ↑ Tang, A.; Tan, J.; Sun, M.; Hamilton, G.; Bydder, M.; Wolfson, T.; Gamst, AC.; Middleton, M. et al. (May 2013). "Nonalcoholic fatty liver disease: MR imaging of liver proton density fat fraction to assess hepatic steatosis.". Radiology 267 (2): 422-31. doi:10.1148/radiol.12120896. PMID 23382291.
- ↑ STC. 6 December 2010.
- ↑ Guindi, M. September 17, 2009.