Difference between revisions of "Low-grade squamous intraepithelial lesion"
| Line 71: | Line 71: | ||
Features:<ref name=Ref_PBoD1075-6>{{Ref PBoD|1075-6}}</ref> | Features:<ref name=Ref_PBoD1075-6>{{Ref PBoD|1075-6}}</ref> | ||
*"Koilocytic atypia":<ref name=Ref_GP146>{{Ref GP|146}}</ref> | *"Koilocytic atypia":<ref name=Ref_GP146>{{Ref GP|146}}</ref> | ||
** | **Clear cytoplasmic halos (perinuclear clearing). | ||
**Nuclear enlargement >=3:1 enlarged nucleus:normal nucleus. | **Nuclear enlargement. | ||
**Nuclear membrane irregularities. | ***Classically >=3:1 enlarged nucleus:normal nucleus. | ||
**Nuclear hyperchromasia. | ***May be mild (superficial cells = size of basal cells). | ||
**Nuclear membrane irregularities - '''important'''. | |||
**Nuclear hyperchromasia - '''important'''. | |||
**Coarse chromatin. | **Coarse chromatin. | ||
**Binucleation may be seen (cytopathic effect of [[HPV]]).<ref name=pmid11491378>{{cite journal |author=Roteli-Martins CM, Derchain SF, Martinez EZ, Siqueira SA, Alves VA, Syrjänen KJ |title=Morphological diagnosis of HPV lesions and cervical intraepithelial neoplasia (CIN) is highly reproducible |journal=Clin Exp Obstet Gynecol |volume=28 |issue=2 |pages=78–80 |year=2001 |pmid=11491378 |doi= |url=}}</ref> | **+/-Binucleation may be seen (cytopathic effect of [[HPV]]).<ref name=pmid11491378>{{cite journal |author=Roteli-Martins CM, Derchain SF, Martinez EZ, Siqueira SA, Alves VA, Syrjänen KJ |title=Morphological diagnosis of HPV lesions and cervical intraepithelial neoplasia (CIN) is highly reproducible |journal=Clin Exp Obstet Gynecol |volume=28 |issue=2 |pages=78–80 |year=2001 |pmid=11491378 |doi= |url=}}</ref> | ||
***Useful when present. | |||
Note: | Note: | ||
| Line 91: | Line 94: | ||
Koilocytes: | Koilocytes: | ||
*Perinuclear clearing. | *Perinuclear clearing. | ||
*Nuclear changes. | **Halo should be crystal clear. | ||
*Nuclear changes - '''key feature'''. | |||
**Size similar (or larger) to those in the basal layer of the epithelium. | **Size similar (or larger) to those in the basal layer of the epithelium. | ||
**Nuclear enlargement should be evident on low power, i.e. 25x. <ref>V. Dube 2008.</ref> | ***Nuclear enlargement should be evident on low power, i.e. 25x.<ref>V. Dube 2008.</ref> | ||
**Central location - nucleus should be | **Nuclear hyperchromasia. | ||
**Central location - nucleus should be in the middle of the cell. | |||
***Benign cells have a small nucleus that is peripheral. | |||
===Images=== | ===Images=== | ||
Revision as of 12:25, 31 January 2014
| Low-grade squamous intraepithelial lesion | |
|---|---|
| Diagnosis in short | |
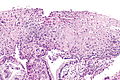
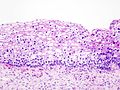
 LSIL. H&E stain. | |
|
| |
| LM | nuclear membrane irregularies, nuclear hyperchromasia, +/-clear perinuclear halos (koilocytic change), +/-nuclear enlargement, large NC ratio (usually ~ 1:3), +/-mitoses (lower third) |
| LM DDx | high-grade squamous intraepithelial lesion, squamous metaplasia, reactive changes, normal cervix |
| IHC | p16 -ve (or lower 1/3 +ve), Ki-67 occasional cells - lower half |
| Site | uterine cervix |
|
| |
| Signs | acetowhite lesion |
| Prevalence | common |
| Prognosis | benign, usually regresses |
| Clin. DDx | squamous metaplasia |
| Treatment | follow-up - unless persistent |
Low-grade squamous intraepithelial lesion, abbreviated LSIL, is a pre-cancerous lesions of the uterine cervix.
Increasingly, the term is being applied to other anatomical sites, e.g. vagina.
It is in the larger category of squamous intraepithelial lesion, abbreviated SIL.
General
- Precursor lesion of cervical squamous cell carcinoma.
- Usually associated with human papilloma virus.
SIL is divided into grades:
- Low-grade.
- High-grade.
The new and old terminology
| SIL (current terminology) | LSIL | HSIL |
|---|---|---|
| Recent terminology | CIN I | CIN II, CIN III |
| Very old terminology | mild dysplasia | moderate dysplasia, severe dysplasia |
Treatment
Overview:
- LSIL: follow-up unless persistent. It usually regresses on its own.
Gross
Microscopic
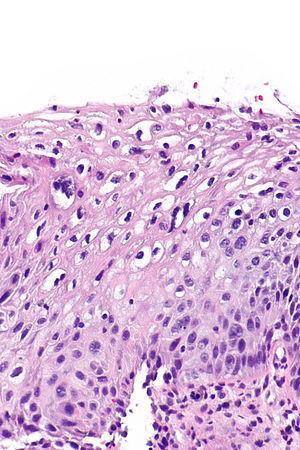
Features:[2]
- "Koilocytic atypia":[3]
- Clear cytoplasmic halos (perinuclear clearing).
- Nuclear enlargement.
- Classically >=3:1 enlarged nucleus:normal nucleus.
- May be mild (superficial cells = size of basal cells).
- Nuclear membrane irregularities - important.
- Nuclear hyperchromasia - important.
- Coarse chromatin.
- +/-Binucleation may be seen (cytopathic effect of HPV).[4]
- Useful when present.
Note:
- Atypical cells usually close to basement membrane.
- May be seen, focally, in the upper layers.[3]
DDx:
- High-grade squamous intraepithelial lesion.
- Squamous metaplasia of the uterine cervix.
- Reactive squamous epithelium of the uterine cervix.
- Normal cervix.
Koilocytes versus benign squamous
Koilocytes:
- Perinuclear clearing.
- Halo should be crystal clear.
- Nuclear changes - key feature.
- Size similar (or larger) to those in the basal layer of the epithelium.
- Nuclear enlargement should be evident on low power, i.e. 25x.[5]
- Nuclear hyperchromasia.
- Central location - nucleus should be in the middle of the cell.
- Benign cells have a small nucleus that is peripheral.
- Size similar (or larger) to those in the basal layer of the epithelium.
Images
www:
IHC
Features:[6]
- p16.
- Diffuse strong staining involving at least all of the basal aspect of the epithelium = CIN II or CIN III.
- Patchy, weak positive staining = CIN I or squamous metaplasia.
- Ki-67.
- Several positive cells above basal layer suggests CIN II or CIN III.
Notes:
- Both p16 and Ki-67 are usually negative in CIN I -- 75% of cases.[7]
- CIN I with p16 staining appears to have a higher risk of progression the p16 negative CIN I.[8]
Sign-out
ECC - cannot grade
UTERINE CERVIX, BIOPSY: - FRAGEMENTS OF SQUAMOUS EPITHELIUM SHOWING DYSPLASIA, SEE COMMENT. COMMENT: The fragments of squamous epithelium do not show full epithelial thickness. Thus, while dysplasia is apparent, it is not possible to distinguish low-grade from high-grade in this specimen. That said, there is at least low grade-dysplasia. Follow-up is recommended with re-biopsy if clinically indicated.
Cervical biopsy
UTERINE CERVIX, BIOPSY: - LOW-GRADE SQUAMOUS INTRAEPITHELIAL LESION (LSIL). - NO ENDOCERVICAL EPITHELIUM IDENTIFIED.
UTERINE CERVIX, BIOPSY: - LOW-GRADE SQUAMOUS INTRAEPITHELIAL LESION (LSIL). - TRANSFORMATION ZONE PRESENT.
UTERINE CERVIX, BIOPSY: - LOW-GRADE SQUAMOUS INTRAEPITHELIAL LESION (LSIL). - CERVICITIS, CHRONIC. - NO ENDOCERVICAL EPITHELIUM IDENTIFIED.
UTERINE CERVIX, BIOPSY: - LOW-GRADE SQUAMOUS INTRAEPITHELIAL LESION (LSIL). - TRANSFORMATION ZONE PRESENT. COMMENT: A p16 stain is patchy and confined mostly to the lower aspect of the squamous epithelium.
CIN 1
UTERINE CERVIX, BIOPSY: - CERVICAL INTRAEPITHELIAL NEOPLASIA 1 (MILD DYSPLASIA). - TRANSFORMATION ZONE PRESENT.
COMMENT: The Ki-67 positive cells are confined to the lower aspect of the squamous epithelium. A p16 stain is negative.
Micro
The sections show the transformation zone. The squamous epithelium has cells with an increased nuclear size, nuclear hyperchromasia, perinuclear clearing and irregularities in the nuclear membrane. The nucleus-to-cytoplasm ratio is mildly increased. Occasional binucleation is identified. Mitoses are seen in the low third of the epithelium. Nucleoli are not apparent. No columnar dysplasia is identified.
See also
References
- ↑ Li, W.; Venkataraman, S.; Gustafsson, U.; Oyama, JC.; Ferris, DG.; Lieberman, RW.. "Using acetowhite opacity index for detecting cervical intraepithelial neoplasia.". J Biomed Opt 14 (1): 014020. doi:10.1117/1.3079810. PMID 19256708.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1075-6. ISBN 0-7216-0187-1.
- ↑ 3.0 3.1 Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 146. ISBN 978-0443069208.
- ↑ Roteli-Martins CM, Derchain SF, Martinez EZ, Siqueira SA, Alves VA, Syrjänen KJ (2001). "Morphological diagnosis of HPV lesions and cervical intraepithelial neoplasia (CIN) is highly reproducible". Clin Exp Obstet Gynecol 28 (2): 78–80. PMID 11491378.
- ↑ V. Dube 2008.
- ↑ Singh, M.; Mockler, D.; Akalin, A.; Burke, S.; Shroyer, A.; Shroyer, KR. (Feb 2012). "Immunocytochemical colocalization of P16(INK4a) and Ki-67 predicts CIN2/3 and AIS/adenocarcinoma.". Cancer Cytopathol 120 (1): 26-34. doi:10.1002/cncy.20188. PMID 22162342.
- ↑ Jackson, JA.; Kapur, U.; Erşahin, Ç. (Apr 2012). "Utility of p16, Ki-67, and HPV test in diagnosis of cervical intraepithelial neoplasia and atrophy in women older than 50 years with 3- to 7-year follow-up.". Int J Surg Pathol 20 (2): 146-53. doi:10.1177/1066896911427703. PMID 22104735.
- ↑ del Pino, M.; Garcia, S.; Fusté, V.; Alonso, I.; Fusté, P.; Torné, A.; Ordi, J. (Nov 2009). "Value of p16(INK4a) as a marker of progression/regression in cervical intraepithelial neoplasia grade 1.". Am J Obstet Gynecol 201 (5): 488.e1-7. doi:10.1016/j.ajog.2009.05.046. PMID 19683687.