Difference between revisions of "Autoimmune hepatitis"
Jump to navigation
Jump to search
(split out) |
m (tweak) |
||
| Line 28: | Line 28: | ||
| ClinDDx = [[primary biliary cirrhosis]], [[primary sclerosing cholangitis]] | | ClinDDx = [[primary biliary cirrhosis]], [[primary sclerosing cholangitis]] | ||
}} | }} | ||
'''Autoimmune hepatitis''', abbreviated ''AIH'', in an uncommon [[medical liver disease]] that occurs in adults and children. | '''Autoimmune hepatitis''', abbreviated ''AIH'', in an uncommon [[medical liver disease]] that occurs in adults and children. | ||
Revision as of 11:01, 9 August 2013
| Autoimmune hepatitis | |
|---|---|
| Diagnosis in short | |
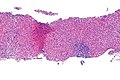
 Autoimmune hepatitis. H&E stain. | |
|
| |
| LM | interface hepatitis with plasma cells, +/- bile duct injury |
| LM DDx | primary biliary cirrhosis |
| Site | liver |
|
| |
| Blood work | ANA +ve, LKM-1 +ve, IgG +ve, SMA +ve, HBV -ve, HCV -ve, HIV -ve |
| Clin. DDx | primary biliary cirrhosis, primary sclerosing cholangitis |
Autoimmune hepatitis, abbreviated AIH, in an uncommon medical liver disease that occurs in adults and children.
General
- Several criteria exist to diagnose and histology (alone) is not sufficient.
Diagnosis
Simplifed diagnostic criteria (2008):[1]
- Antibody titer.
- Elevated IgG.
- Liver pathology.
- Exclusion of viral hepatitis.
Details (scoring):[1]
| Finding | Score |
| ANA or SMA 1:40 | 1 point |
| ANA or SMA 1:80 | 2 points |
| LKM-1 1:40 | 2 points |
| IgG upper normal | 1 point |
| IgG 1.1x upper limit | 2 points |
| Histology compatible | 1 point |
| Typical AIH histo. | 2 points |
| No viral hepatitis | 2 points |
Interpretation: Definite >= 7 points. Probable = 6 points.
Notes:
- Autoantibodies may be seen in HCV.[1]
- A normal IgG is very unusual in AIH - but may be seen in atypical variants with zone III involvment.
Abbreviations:
- ANA = anti-nuclear antibody.
- SMA = smooth muscle antibody.
- LKM-1 = liver kidney microsomal type 1 antibody.
Treatment
- Immunosuppresants (prednisone, azathioprine).[2]
Microscopic
Classification:[1]
- Typical:
- Interface hepatitis (zone 1).
- Lymphoplasmacytic infiltration of portal tracts / lobule.
- Periportal plasma cells - key feature.[3]
- Lymphoplasmacytic infiltration of portal tracts / lobule.
- Emperipolesis - one cell penetrates into another one (uncommon finding).
- Hepatic rosette - inflammatory cells around reactive hepatocytes.[4]
- Interface hepatitis (zone 1).
- Compatible:
- Chronic hepatitis - lymphocytic dominant.
- Atypical:
- Signs of an other disease.
Notes:
- PAS stain may be useful - find plasma cells.[5]
- Lots of plasma cells should prompt consideration of AIH.
- Atypical Autoimmune hepatitis may have zone III involvment (lymphoplasmacytic infiltrate)[2] and a normal IgG.[6]
Images
www:
Emperipolesis:
Sign out
LIVER, RIGHT LOBE, CORE BIOPSY: - LIVER WITH INTERFACE HEPATITIS (GRADE 2/4) WITH PLASMA CELLS. - MODERATE FIBROSIS (STAGE 2/4). COMMENT: The histologic findings are compatible with autoimmune hepatitis. Serologic findings (ANA positive, IgG positive, viral serology negative) are noted. Correlation with LKM-1 serology is suggested, if not done. The histology is not suggestive of primary biliary cirrhosis.
Micro
The sections show two cores of liver with an interface hepatitis with plasma cells. Numerous eosinophils are seen focally in the portal tract. The number of ducts is focally increased in several portal tracts and associated with neutrophils (ductular reaction). Size of biopsy: adequate. Fragmentation: absent. Fibrosis: Stage 2/4. Fibrous septa: present. Septa with curved contours: present, focally only. Large droplet steatosis (% of hepatocytes): minimal <5%. Ballooning of hepatocytes: absent. Mallory-Denk bodies: absent. Portal inflammation: present (1/4). Interface activity: mild (1/4). Lobular necroinflammation: not identified. Ducts: numbers within normal limits. Duct injury: present. Ductular reaction: present. Cholestasis: not apparent. Terminal hepatic venules: present. Iron stain: absent. Ground glass cells with routine stains: absent.
See also
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 Scoring systems for the diagnosis of autoimmune hepatitis: past, present, and future. Wiegard C, Schramm C, Lohse AW. Semin Liver Dis. 2009 Aug;29(3):254-61. Epub 2009 Aug 12. PMID 19675998
- ↑ Jump up to: 2.0 2.1 Non-classical phenotypes of autoimmune hepatitis and advances in diagnosis and treatment. Czaja AJ, Bayraktar Y. World J Gastroenterol. 2009 May 21;15(19):2314-28. Review. PMID 19452572.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 448. ISBN 978-1416054542.
- ↑ Jump up to: 4.0 4.1 Malik, TA.; Saeed, S. (May 2010). "Autoimmune hepatitis: a review.". J Pak Med Assoc 60 (5): 381-7. PMID 20527613. http://www.jpma.org.pk/full_article_text.php?article_id=2051.
- ↑ URL: http://iv.iiarjournals.org/content/19/6/1097.abstract. Accessed on: 9 December 2010.
- ↑ FW. 21 September 2009.