Prostate cancer staging
(Redirected from SVI)
Jump to navigation
Jump to search
The article deals with prostate cancer staging. A general discussion about staging is found in cancer staging.
An introduction to prostate cancer is found in the prostate cancer article.
General
- Important for prognosis and treatment.
TNM staging system
Tumour
| Stage | Criteria | Notes |
|---|---|---|
| T2 | confined to prostate | subdivision based on bilateral/unilateral involvement not predictive |
| T3a | extension into periprostatic soft tissue (see extraprostatic extension) or bladder neck invasion | |
| T3b | extension into the muscle of the seminal vesicles (see seminal vesicle invasion) | |
| T4 | extension into a surrounding anatomical structure, e.g. urinary bladder | bladder neck invasion is T3b |
Extraprostatic extension
- Abbreviated EPE.
General
- Extraprostatic extension (EPE) is difficult to assess in prostatectomy specimens.[1]
- The prostate does NOT have a well defined capsule.
- Intraobserver agreement for EPE is fair-moderate and lower than for the surgical margin.[2]
- The prostate does NOT have a well defined capsule.
- EPE, typically, upstages tumours from T2x to T3a.
Prostatectomy specimens
EPE is present in a prostatectomy if there is either:
- A "significant bulge" in the contour of the prostate at low power and no fibromuscular tissue surrounding the malignant cells.
- Malignant cells directly adjacent to peri-prostatic adipose tissue.
Notes:
- The apex of the prostate gland may have some skeletal muscle. Thus, it is difficult to define extension at this site. EPE is not called at the apex by some pathologists; however, it is generally believed to exist.[1]
- The anterior prostate has fibromuscular stroma that is difficult to separate from the extraprostatic tissue.[3]
- Anterior fibromuscular stroma (AFMS) versus extraprostatic extension (EPE): true EPE is proposed to be into the fat or thick rounded muscle bundles.[3]
Prostate biopsy
EPE is present in prostate biopsy if:
- Tumour touches adipose tissue.[4]
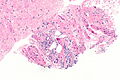
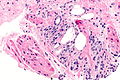
Images
Bladder neck invasion
- Defined as tumour within the thick muscle bundles of the bladder neck or at the bladder neck margin.[citation needed]
- Bladder neck invasion is pT3a.[5]
- Seen in approximately 1% of prostatectomies.[6]
- Bladder neck involvement can be seen without extraprostatic extension.[7]
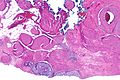
Image
www:
Seminal vesicle invasion
- Abbreviated SVI.
General:
- Typically upstages to pT3b.
- Associations:[8]
- Most SVI is by direct extension ~90%.
- Approximately 20% of patients with pT3x have SVI.
- Usually associated with a large tumour volume (22% versus 12%).
Microscopic:
- Tumour must be in the muscle surrounding the epithelial component; tumour in the adventitia (the loose connective tissue surrounding the seminal vesicles) does not count.[9][10]
Notes:
- Invasion of the adventitia (only) would quality as EPE; this is, usually, T3a.
- Immunostains useful to separate prostate carcinoma from SV are discussed in the seminal vesicle article.
- It is not possible to differentiate the seminal vesicles and ejaculatory ducts based only on histology; thus, on biopsy one can generally comment only on seminal vesicle/ejaculatory duct invasion.
- SVI has been subdivided into three types by pattern of spread (type I: spread along ejaculatory duct complex and into SV, type II: through prostate capsule and then into SV; type III: discontinuous spread/metastasis).[11]
Lymph node
Note:
- Lymph node metastases essentially never happen in Gleason score 6 cancers.
- A study of over 14,000 Gleason score <=6 cases found 22 cases with lymph node metastases -- all of the 19 cases available for review were determined to have a higher Gleason score and some Gleason pattern 4 or 5.[12]
See also
References
- ↑ 1.0 1.1 1.2 Magi-Galluzzi, C.; Evans, AJ.; Delahunt, B.; Epstein, JI.; Griffiths, DF.; van der Kwast, TH.; Montironi, R.; Wheeler, TM. et al. (Jan 2011). "International Society of Urological Pathology (ISUP) Consensus Conference on Handling and Staging of Radical Prostatectomy Specimens. Working group 3: extraprostatic extension, lymphovascular invasion and locally advanced disease.". Mod Pathol 24 (1): 26-38. doi:10.1038/modpathol.2010.158. PMID 20802467.
- ↑ Evans, AJ.; Henry, PC.; Van der Kwast, TH.; Tkachuk, DC.; Watson, K.; Lockwood, GA.; Fleshner, NE.; Cheung, C. et al. (Oct 2008). "Interobserver variability between expert urologic pathologists for extraprostatic extension and surgical margin status in radical prostatectomy specimens.". Am J Surg Pathol 32 (10): 1503-12. doi:10.1097/PAS.0b013e31817fb3a0. PMID 18708939.
- ↑ 3.0 3.1 Fine SW, Al-Ahmadie HA, Gopalan A, Tickoo SK, Scardino PT, Reuter VE (November 2007). "Anatomy of the anterior prostate and extraprostatic space: a contemporary surgical pathology analysis". Adv Anat Pathol 14 (6): 401–7. doi:10.1097/PAP.0b013e3181597a9c. PMID 18049129.
- ↑ Epstein, JI.; Srigley, J.; Grignon, D.; Humphrey, P. (Sep 2007). "Recommendations for the reporting of prostate carcinoma.". Hum Pathol 38 (9): 1305-9. doi:10.1016/j.humpath.2007.05.015. PMID 17707261.
- ↑ Chung, MS.; Lee, SH.; Lee, DH.; Chung, BH. (Feb 2013). "Evaluation of the 7th American Joint Committee on cancer TNM staging system for prostate cancer in point of classification of bladder neck invasion.". Jpn J Clin Oncol 43 (2): 184-8. doi:10.1093/jjco/hys196. PMID 23225909.
- ↑ Pierorazio, PM.; Epstein, JI.; Humphreys, E.; Han, M.; Walsh, PC.; Partin, AW. (Jan 2010). "The significance of a positive bladder neck margin after radical prostatectomy: the American Joint Committee on Cancer Pathological Stage T4 designation is not warranted.". J Urol 183 (1): 151-7. doi:10.1016/j.juro.2009.08.138. PMID 19914651.
- ↑ Poulos, CK.; Koch, MO.; Eble, JN.; Daggy, JK.; Cheng, L. (Oct 2004). "Bladder neck invasion is an independent predictor of prostate-specific antigen recurrence.". Cancer 101 (7): 1563-8. doi:10.1002/cncr.20551. PMID 15378493.
- ↑ Sapre, N.; Pedersen, J.; Hong, MK.; Harewood, L.; Peters, J.; Costello, AJ.; Hovens, CM.; Corcoran, NM. (Dec 2012). "Re-evaluating the biological significance of seminal vesicle invasion (SVI) in locally advanced prostate cancer.". BJU Int 110 Suppl 4: 58-63. doi:10.1111/j.1464-410X.2012.11477.x. PMID 23194127.
- ↑ Lester, Susan Carole (2010). Manual of Surgical Pathology (3rd ed.). Saunders. pp. 409. ISBN 978-0-323-06516-0.
- ↑ Berney, DM.; Wheeler, TM.; Grignon, DJ.; Epstein, JI.; Griffiths, DF.; Humphrey, PA.; van der Kwast, T.; Montironi, R. et al. (Jan 2011). "International Society of Urological Pathology (ISUP) Consensus Conference on Handling and Staging of Radical Prostatectomy Specimens. Working group 4: seminal vesicles and lymph nodes.". Mod Pathol 24 (1): 39-47. doi:10.1038/modpathol.2010.160. PMID 20818343.
- ↑ Potter, SR.; Epstein, JI.; Partin, AW. (2000). "Seminal vesicle invasion by prostate cancer: prognostic significance and therapeutic implications.". Rev Urol 2 (3): 190-5. PMID 16985773.
- ↑ Ross, HM.; Kryvenko, ON.; Cowan, JE.; Simko, JP.; Wheeler, TM.; Epstein, JI. (Sep 2012). "Do adenocarcinomas of the prostate with Gleason score (GS) ≤6 have the potential to metastasize to lymph nodes?". Am J Surg Pathol 36 (9): 1346-52. doi:10.1097/PAS.0b013e3182556dcd. PMID 22531173.