Gastrointestinal cytopathology
(Redirected from GI cytology)
Jump to navigation
Jump to search
Gastrointestinal cytopathology, also known as GI cytology, is a relatively small part of cytopathology.
This article deals only with gastrointestinal cytopathology. An introduction to cytopathology is in the cytopathology article. Histopathology of the gastrointestinal tract is dealt with in gastrointestinal pathology.
Liver
Brief DDx:
- Metastatic adenocarcinoma, usu. colorectal adenocarcinoma.
- Hepatocellular carcinoma.
Others:
- Cholangiocarcinoma - usu. adenocarcinoma NOS, i.e. non-specific.
- Epithelioid hemangioendothelioma.
- Angiomyolipoma.
Normal liver
Cytology
Features:
- Hepatocytes:
- Abundant cytoplasm
- central nucleus +/- binucleation.
- +/-Yellow granular pigment (bile).
- Bile ductules between adjacent cells.
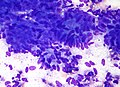
Hepatocellular carcinoma
Main article: Hepatocellular carcinoma
Cytology
Features:
- Architecture - single cells and large clusters:
- Cohesive clusters of cells (hepatocytes) surrounded by endothelial cells - diagnostic.[1]
- Capillaries traversing the fragments.
- Cells:
- Central nucleus +/-prominent nucleoli,[2] +/-nuclear inclusions.
- +/-Multinucleation.
- +/-Yellow cytoplasmic pigment (bile).
- +/-Nuclear atypia.
- +/-High NC ratio.
Notes:
- Low grade HCC is composed of cytologically normal appearing cells; the arrangement is what is diagnostic of malignancy.[1]
- Fibrolamellar HCC has very large cells.
Images:
Cholangiocarcinoma
Main article: Cholangiocarcinoma
Cytology
Features:
- Looks like an adenocarcinoma:
- Eccentric nuclei, one nucleolus per cell, abundant cytoplasm, nuclear size var. cell-to-cell, irregular nuclear membrane, irregular/uneven chromatin pattern.
Epithelioid hemangioendothelioma
Main article: Epithelioid hemangioendothelioma
General
- Rare.
Cytology
Features:
- Large atypical cells with:
- Nuclear inclusions
- Moderate cytoplasm.
- +/-Multinucleation.
IHC
- Factor VIII +ve.
Common bile duct
Normal:
- Monolayer of small blue cells.
Notes:
- Caution is advised when calling malignancy in the setting of a stent or stones.
Adenocarcinoma
Features:
- Hyperchromasia.
- Pencil-shaped nuclei.
- Nuclear membrane irregularities.
Images
www
Stomach
Normal stomach
General
- Important as it may be a contaminant in a pancreatic FNA.
Cytology
Features:
- Bland cells with round nuclei.
- Granular cells with red cytoplasm (on Pap stain) - parietal cells - distinctive.
Note:
- May be difficult to distinguish from pancreas ductal epithelium.[4]
Small bowel
Epithelium:[4]
- Orderly flat sheets of smaller (blue) cells without atypia.[3]
- "Orderly" = nuclei do not overlapped.
- Goblet cells - key feature.
Notes:
- May appear to be similar to stomach and pancreatic duct.[4]
Images
www
Esophagus
- Cytology may be done to look for candida.
- Report should comment on the presence of candida - if it is seen.
A short DDx:
Pancreas
A short DDx:
- Normal:
- Duct.
- Acini.
- Cystic lesions:
- Others:
Normal pancreas
Cytology
Features - duct:
- 2-D sheet of cells - equally spaced.
- Moderate-to-abundant cytoplasm.
Features - acini:
- Clustered cells +/- nuclear overlap.
- Round bland nuclei.
- Small nucleoli.
- Moderate cytoplasm.
Pancreatic pseudocyst
General
- Symptomatic, e.g. abdominal pain.
- Asymptomatic pseudocysts are typically observed, as a large number resolve spontaneously.[5]
- Classically associated with pancreatitis secondary to alcohol.[6]
- Pathologic diagnosis of exclusion.
Cytology
Features:
- Histiocytes.
- Should be paucicellular otherwise.
- Necrotic debris - granular.
Note:
- Pseudocysts, by definition, do not have an epithelial lining.
- Luminal GI tract contamination - may lead to confusion with mucinous neoplasm.
DDx:
- Mucinous neoplasm.
- Serous neoplasm.
Serous neoplasm
General
- May be associated with von Hippel-Lindau syndrome.
- Usu. body or tail.
- Classically have a central stellate scar - seen radiologically.
Cytology
Features:
- Cuboidal/flat cells in clusters or sheets.
- +/-Nuclear grooves.
Stains
- PAS +ve.
- PASD -ve.
Mucinous neoplasm
General
- Pancreatic head: classically IPMN.
- IPMN assoc. with colloid carcinoma.
- Pancreatic body & tail: mucinous tumour.
Cytology
Features:
- Clusters or sheets of mucinous cells.
- +/-Nuclear atypia.
- +/-Thick mucin.
- Suggestive of IPMN.
Notes:
- In the body & tail mucinous cells may be contamination from the stomach.
- Lesions in the pancreatic head are approached from the duodenum - do not have this problem.
- Ovarian stroma is not seen on cytology.
- Thick mucin may be from stomach.
Image:
Solid pseudopapillary neoplasm
Main article: Solid pseudopapillary neoplasm
- Abbreviated SPN.
General
- Young women.
- Tail of pancreas.
Cytology
Features:[8]
- Papillary formations - composed of small cells with:
- Scant cytoplasm.
- +/-Nuclear grooves.
- +/-Cholesterol clefts.
Note:
- There are no true papillae in SPN.
DDx:
- Pancreatic pseudocyst.
- Pancreatic neuroendocrine tumour - single cells, classically plasmacytoid.
IHC
- PR +ve.
- Beta-catenin +ve.
- CD10 +ve.
Others:
- Chromogranin A -ve.
Pancreatic neuroendocrine tumour
Main article: Pancreatic neuroendocrine tumour
- Previously known as islet cell tumour of the pancreas.
General
- Classically solid.
- May be cystic.
Cytology
Features:
- Round nuclei with salt and pepper chromatin.
- Moderate nuclear size variation.
- Classically single cells with plasmacytoid morphology.
DDx:
IHC
- Chromogranin A +ve.
- Synaptophysin +ve.
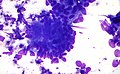
Pancreatic adenocarcinoma
Main article: Invasive ductal carcinoma of the pancreas
- AKA ductal carcinoma.
Cytology
Features:
- Single cells.
- Should be present.
- Monolayer of irregularly spaced cells - described as "drunken honeycomb".
- Nuclear atypia +/-grooves, +/-chromatin clearing.
- Significant atypia: >=4:1 ratio between the nuclear diameter of cells.
Image:
- Pancreatic adenocarcinoma - marked nuclear atypia - low mag. (flickr.com/euthman).
- Pancreatic adenocarcinoma - marked nuclear atypia - high mag. (flickr.com/euthman).
- Pancreatic adenocarcinoma - drunken honeycomb - low mag. (flickr.com/euthman).
- Pancreatic adenocarcinoma - drunken honeycomb - high mag. (flickr.com/euthman).
Acinar cell carcinoma
Main article: Acinar cell carcinoma of the pancreas
General
- Very rare.
Cytology
Features:
- High cellularity - important feature.
- Lack of ducts.
- Single cells and small cell clusters with abundant granular (metachromatic) cytoplasm - similar to normal pancreatic acini.
- Naked nuclei.
Note:
- Considered to be a difficult diagnosis.
See also
References
- ↑ 1.0 1.1 Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 679. ISBN 978-1416025887.
- ↑ 2.0 2.1 URL: http://moon.ouhsc.edu/kfung/jty1/CytoLearn/CytoQuiz/CQ-021-040/CQ-034-M.htm. Accessed on: 9 April 2012.
- ↑ 3.0 3.1 3.2 Conrad, R.; Cobb, C.; Raza, A. (Sep 2012). "Role of cytopathology in the diagnosis and management of gastrointestinal tract cancers.". J Gastrointest Oncol 3 (3): 285-98. doi:10.3978/j.issn.2078-6891.2012.023. PMID 22943018.
- ↑ 4.0 4.1 4.2 Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 680 (Q23). ISBN 978-1416025887.
- ↑ Gumaste, VV.; Aron, J.. "Pseudocyst management: endoscopic drainage and other emerging techniques.". J Clin Gastroenterol 44 (5): 326-31. doi:10.1097/MCG.0b013e3181cd9d2f. PMID 20142757.
- ↑ Andrén-Sandberg, A.; Dervenis, C. (Jan 2004). "Pancreatic pseudocysts in the 21st century. Part I: classification, pathophysiology, anatomic considerations and treatment.". JOP 5 (1): 8-24. PMID 14730118.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/OPAQ/PNPT/PN-NS01-Ans.htm. Accessed on: 22 February 2012.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/CytoLearn/CytoQuiz/CQ-021-040/CQ-029-M.htm. Accessed on: 9 April 2012.