Extramammary Paget disease
(Redirected from EMPD)
Jump to navigation
Jump to search
| Extramammary Paget disease | |
|---|---|
| Diagnosis in short | |
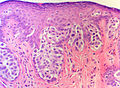
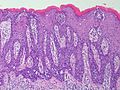
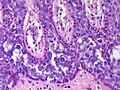
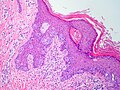
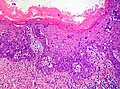
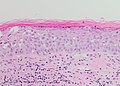
 Extramammary Paget's disease. H&E stain. | |
|
| |
| LM | large epithelioid cells - nested or single - in the epidermis, clear/pale cytoplasm (occasionally eosinophilic), large nucleoli |
| LM DDx | benign Toker cell hyperplasia, malignant melanoma, Bowen's disease, apocrine carcinoma of the skin |
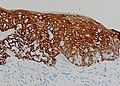
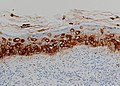
| IHC | CK7 +ve, CEA +ve, S-100 -ve, CK5/6 -ve, HER2 +ve |
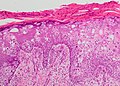
| Gross | erythema, +/-weeping, +/-crusted |
| Site | vulva, penis, scrotum, others |
|
| |
| Symptoms | pruritis (itchy) |
| Prognosis | typically benign - usually not associated with an underlying malignancy (unlike Paget's disease of the breast) |
| Clin. DDx | contact dermatitis, lichen sclerosus |
Extramammary Paget disease, abbreviated EMPD, is a skin disease. As the name suggests, there is also a Paget disease of the breast.
There is also a Paget disease of the bone - just to make things confusing. This is dealt with in the bone article and has nothing (from a pathologic perspective) to do with the Paget disease discussed in this article
General
- Two types
- Primary Extramammary Paget disease - thought to be an intraepidermal carcinoma arising from cutaneous apocrine glands
- Arises in apocrine rich areas - usually the vulva but also the groin, inguinal area, perineum, penis[1] or scrotum [2] and rarely axilla or eye.
- Usually entirely intraepidermal but may rarely be associated with an underlying apocrine gland carcinoma (in contrast to mammary Paget disease which is usually associated with underlying mammary carcinoma).
- Secondary Extramammary Paget disease - intraepidermal spread from a distant tumour
- Usually of urothelial or colorectal origin.
- Arises in the perineal areas near these organs.
- Primary Extramammary Paget disease - thought to be an intraepidermal carcinoma arising from cutaneous apocrine glands
Clinical:
- Pruritis.
- R/O VIN.
- R/O vulvitis.
Gross
Features:[2]
- Plaque with an irregular border.
- Erythematous or white.
Clinical DDx:
- Lichen sclerosus.[3]
- Vulvar intraepithelial neoplasia
- Vulvar squamous cell carcinoma in situ
- Other vulvitis
Images
Microscopic
Features:
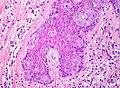
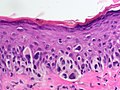
- Epitheliod morphology (round/ovoid).
- Cells nested or single.
- Classically Paget cells ride above the basal cell layer
- But the process can fill the entire epidermis
- Clear/pale cytoplasm key feature - may also be eosinophilic.
- Large nucleoli.
Images
DDx
- Malignant melanoma in situ - atypical cells are mostly basilar with upward migration.
- Squamous cell carcinoma in situ "Bowen disease"
- Pagetoid squamous cell carcinoma in situ can look identical to extramammary Paget disease
- But should have some areas of typical SCCIS with full thickness cohesive atypia
- Pagetoid vulvar/anal/penil HPV associated intraepithelial neoplasia - Pagetoid areas often merge into areas of typical VIN
- 'Paget disease' associated with an underlying local carcinoma - apocrine, Bartholin's duct etc (rare).
- Notice that mammary Paget disease and Toker cell hyperplasia are not part of this DDX (wrong location) except possibly in the rare case of EMPD arising in the axilla where mammary Paget disease arising from a ectopic nipple or ectopic breast tissue may be a consideration.
- Notice that EMPD is not really part of the DDX of pagetoid cutaneous squamous cell carcinoma arising on typical sun damaged skin (arm, cheek, leg) - if it's not from an apocrine rich area (and these are usually in the shade) - it's not EMPD.
Stains
- Mucicarmine stain +ve.
IHC
- Extramammary Paget disease is a 'big' diagnosis in that the diagnosis will have significant clinical consequences. So a large panel of immuno is required to nail down the diangosis.
- Is the lesion epithelial or melanocytic? (S100, Melan A)
- Is the lesion adenocarcinoma or squamous cell carcinoma?
- Low molecular weight (CK7, cam5.2) or high molecular weight keratins (34BE12, CK5/6)?
- Don't rely entirely on the cytokeratin profile
- Pagetoid squamous cell carcinoma in situ can lose HMW keratins and produce a LMW profile.
- Adenocarcinoma markers? - CEA, BerEP4
- Nuclear differentiation markers? - p63 or p40 (squamous) vs GATA3 (adnexal)
- Low molecular weight (CK7, cam5.2) or high molecular weight keratins (34BE12, CK5/6)?
- Is the lesion primary or secondary?
- Secondary extramammary Paget disease may be CK20 positive (urothelial or rectal)
- Primary cutaneous extramammary Paget disease is always CK20 negative.
- If CK20 is positive are other organ specific markers positive? - CDX2 - colorectal or GATA3 - urothelial
Panel: You can not rely on any one marker - a panel is required
- A carcinoma marker - CEA or BerEP4 or both
- Differential keratins - low molecular weight (glandular) cam5.2, CK7 vs high molecular weight (squamous) 34BE12, CK5/6[4]
- CK7 and CK20 - where does it come from?
- S100 and Melan A - exclude melanoma in situ
- Differentiation markers; GATA - apocrine and urothelial, p63 and p40 - squamous, CDX2 - colorectal
- Notice urothelial origin Paget can show immunos patterns "transitional" between glandular and squamous epithelium
- A CK20 negative urothelial origin EMPD could show a similar immunoprofile as a primary cutaneous EMPD.
- Notice that you do not need to include markers for mammary Paget disease or Toker cells.
- Do not rely on CK7 alone as CK7 may be positive in pagetoid squamous cell carcinoma in situ or extramammary Paget disease [5]
- p16 is not helpful in this DDX as VIN, EMPD and urothelial carcioma can be positive for this marker [6]
Roughly and with caveats........
- Primary cutaneous extramammary Paget disease - CK7+, CK20-, BerEP4+, CEA+, S100-, MelanA-, 34BE12-, CK5/6-, p63-, GATA+, CDX2-
- Secondary extramammary Paget disease - colorectal origin - CK7-, CK20+, BerEP4+, CEA+, S100-, MelanA-, 34BE12-, CK5/6-, p63-, GATA-, CDX2+
- Secondary extramammary Paget disease - urothelial origin - CK7+, CK20+/-, BerEP4-/+, CEA-/+, S100-, MelanA-, 34BE12+, CK5/6+/-, p63+, GATA+, CDX2-
- Pagetoid VIN or squamous cell carcinoma in situ - CK7-, CK20-, BerEP4-, CEA-, S100-, MelanA-, 34BE12+, CK5/6+ p63+, GATA-, CDX2-
- Melanoma in situ - CK7-, CK20-, BerEP4-, CEA-, S100+, MelanA+, 34BE12-, CK5/6- p63-, GATA-, CDX2-
Sometimes it's helpful to lower the condenser when viewing this immunopanel - with a refractile background, the cell borders are highlighted and the large Paget cells stand out from the keratinocytes.
See also
References
- ↑ Ekwueme, KC.; Zakhour, HD.; Parr, NJ. (2009). "Extramammary Paget's disease of the penis: a case report and review of the literature.". J Med Case Reports 3: 4. doi:10.1186/1752-1947-3-4. PMID 19126202.
- ↑ 2.0 2.1 2.2 Guerra, R.; Misra, S. (2013). "Management of Extramammary Paget's Disease: A Case Report and Review of the Literature.". Case Rep Dermatol Med 2013: 436390. doi:10.1155/2013/436390. PMID 24349803.
- ↑ Bansal, D.; Bowman, CA. (Feb 2004). "Extramammary Paget's disease masquerading as lichen sclerosus.". Int J STD AIDS 15 (2): 141-2. doi:10.1258/095646204322764361. PMID 15006079.
- ↑ RS. May 2010.
- ↑ Raju, RR.; Goldblum, JR.; Hart, WR. (Apr 2003). "Pagetoid squamous cell carcinoma in situ (pagetoid Bowen's disease) of the external genitalia.". Int J Gynecol Pathol 22 (2): 127-35. PMID 12649666.
- ↑ Sah, SP.; McCluggage, WG. (Mar 2013). "Florid vulval Paget disease exhibiting p16 immunoreactivity and mimicking classic VIN.". Int J Gynecol Pathol 32 (2): 221-7. doi:10.1097/PGP.0b013e31825909f6. PMID 23370646.