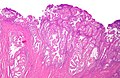
Endometrioid endometrial carcinoma
| Endometrioid endometrial carcinoma | |
|---|---|
| Diagnosis in short | |
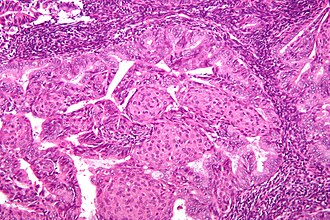 Endometrioid endometrial adenocarcinoma. H&E stain. | |
|
| |
| Synonyms | endometrioid endometrial adenocarcinoma |
| LM DDx | complex endometrial hyperplasia, microglandular hyperplasia of the cervix, endocervical adenocarcinoma, serous carcinoma of the endometrium - esp. for high-grade tumours, clear cell carcinoma of the endometrium, simple endometrial hyperplasia, endometrium with squamous morules |
| IHC | ER +ve, PR +ve, vimentin +ve, p16 -ve, CEA -ve |
| Gross | endometrial thickening |
| Grossing notes | hysterectomy for endometrial cancer grossing |
| Site | endometrium - see endometrial carcinoma |
|
| |
| Associated Dx | obesity |
| Syndromes | Lynch syndrome, Cowden syndrome |
|
| |
| Signs | abnormal uterine bleeding (AUB) |
| Prevalence | common |
| Prognosis | good - esp. low-grade |
| Treatment | usu. total hysterectomy |
Endometrioid endometrial carcinoma, abbreviated EEC, is the most common type of endometrial carcinoma. It is strongly associated with obesity.
It is also known as endometrioid endometrial adenocarcinoma.
General
- Good prognosis - usually.
- Women in 40s & 50s.
- Associated with estrogen excess (unopossed estrogen stimulation).
- Typical patient is obese.
Associated syndromes:
Gross
- Thickened endometrium.
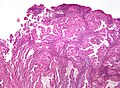
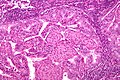
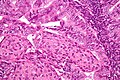
Microscopic
Features:
- Atypical (ovoid) glands with - one of the following four:[3][4][5]
- Desmoplastic stromal response.
- Confluent cribriform growth. †
- Extensive papillary growth. †
- Severe cytologic atypia. †
- Endometrioid features:
- +/-Low-grade nuclear features.
- Squamous metaplasia - very common.
- Look for squamous morules:
- Ball of cells with an intensely eosinophilic cytoplasm - key feature.
- Central nucleus.
- Intercellular bridges - may be hard to find.
- +/-Dyskeratotic cells.
- Look for squamous morules:
Notes:
- † There is a size cut-off for criteria 2, 3 and 4: > 2.1 mm.[4]
- Dyskeratosis = abnormal keratinization;[6] classically have intensely eosinophilic cytoplasm +/- nuclear fragmentation (karyorrhexis) - see: several dyskeratotic cells.
- Squamous metaplasia != neoplastic -- it may occur due to hormones.[7]
- Squamous morules in endometrioid endometrial carcinoma - not associated with HPV infection.[8]
DDx:
- Complex endometrial hyperplasia with atypia.
- Complex endometrial hyperplasia.
- Microglandular hyperplasia of the cervix.
- Endocervical adenocarcinoma.
- Serous carcinoma of the endometrium - esp. if high-grade nuclear features are present diffusely.
- Clear cell carcinoma of the endometrium - esp. when clear cells present.
Grading
- FIGO system most commonly used.
- Based on gland formation & adjusted by nuclear pleomorphism.
Preliminary grade based on gland formation:[9][10][11][12]
- Grade 1: <5% solid component.
- Grade 2: 5-50% solid component.
- Grade 3: >50% solid component.
Modifiers/adjustment:
- High grade nuclei upgrades cancer by one.
- Tadrous says: high grade nuclei = increased size, irregular large nucleoli, irregular chromatin pattern (clumped, coarse).[13]
- Winham et al. describe it as: nuclear pleomorphism identifiable with the 10× objective or enlarged nuclei (1.5-2× normal) with prominent nucleoli, irregular nuclear contours, and dispersed chromatin.[14]
Images
www:
IHC
- Vimentin +ve.
- ER +ve.
- PR +ve.
Others:
- p16 -ve -- positive in serous endometrial carcinoma[15] and endocervical adenocarcinoma.
- CEA -ve.
Sign out
Biopsy
Endometrium, Curettage: - ENDOMETRIOID ENDOMETRIAL ADENOCARCINOMA, preliminary FIGO grade I.
Endometrium, Curettage: - ENDOMETRIOID ENDOMETRIAL ADENOCARCINOMA, preliminary FIGO grade II. Comment: The architecture is in keeping with FIGO I; however, nuclear atypia is present and therefore it is FIGO II.
Block letters
ENDOMETRIUM, BIOPSY: - ENDOMETRIOID ENDOMETRIAL ADENOCARCINOMA, FIGO GRADE I/III.
Hysterectomy
UTERUS WITH CERVIX AND FALLOPIAN TUBES, TOTAL HYSTERECTOMY AND BILATERAL SALPINGECTOMY: - ENDOMETRIOID ENDOMETRIAL ADENOCARCINOMA, FIGO GRADE I/III, pT2, pNx. -- SURGICAL MARGINS NEGATIVE. -- PLEASE SEE TUMOUR SUMMARY. - LEIOMYOMAS WITH HYALINIZATION. - FALLOPIAN TUBES WITHOUT SIGNIFICANT PATHOLOGY.
Micro
The sections show endometrium with complex, fused and cribriform glands with scant intervening stroma over a region measuring greater than 2.1 millimetres. Focally, a desmoplastic stroma is also identified. No nuclear atypia is appreciated.
A subtle pattern of myoinvasion in low grade endometrial endometrioid carcinomas, microcystic, elongated and fragmented (MELF) should be searched for in the absence of frank invasion. At low power, microcystic tumor glands lie separated by muscle from non-invasive carcinoma in edematous stroma. At higher power lie microcystic glands with neutrophils, as well as elongated glands lined by flattened tumor cells. Eosinophilic tumor cells or squamous cells can often be seen within the lumens. [16]
Endocervical versus endometrial - biopsy
The foamy histiocytes in the stroma and lack of desmoplasia slightly favour an endometrial origin; however, the lesion would be best classified with an excisional specimen and in conjunction with the clinical impression.
See also
- Endometrial carcinoma.
- Endometrial hyperplasia.
- Ductal adenocarcinoma of the prostate gland.
- Microcystic elongated and fragmented glands in endometrioid endometrial carcinoma (MELF).
References
- ↑ Lax, SF. (Jan 2002). "[Dualistic model of molecular pathogenesis in endometrial carcinoma].". Zentralbl Gynakol 124 (1): 10-6. doi:10.1055/s-2002-20303. PMID 11873308.
- ↑ Karamurzin, Y.; Soslow, RA.; Garg, K. (Apr 2013). "Histologic evaluation of prophylactic hysterectomy and oophorectomy in Lynch syndrome.". Am J Surg Pathol 37 (4): 579-85. doi:10.1097/PAS.0b013e3182796e27. PMID 23426126.
- ↑ Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 239. ISBN 978-0443069208.
- ↑ 4.0 4.1 Kurman, RJ.; Norris, HJ. (Jun 1982). "Evaluation of criteria for distinguishing atypical endometrial hyperplasia from well-differentiated carcinoma.". Cancer 49 (12): 2547-59. PMID 7074572.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Endometrium_11protocol.pdf. Accessed on: 12 January 2012.
- ↑ URL: http://dictionary.reference.com/browse/dyskeratosis. Accessed on: 5 September 2011.
- ↑ Miranda, MC.; Mazur, MT. (May 1995). "Endometrial squamous metaplasia. An unusual response to progestin therapy of hyperplasia.". Arch Pathol Lab Med 119 (5): 458-60. PMID 7748076.
- ↑ Chinen, K.; Kamiyama, K.; Kinjo, T.; Arasaki, A.; Ihama, Y.; Hamada, T.; Iwamasa, T. (Sep 2004). "Morules in endometrial carcinoma and benign endometrial lesions differ from squamous differentiation tissue and are not infected with human papillomavirus.". J Clin Pathol 57 (9): 918-26. doi:10.1136/jcp.2004.017996. PMID 15333650.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1087-8. ISBN 0-7216-0187-1.
- ↑ URL: http://www.pathologyoutlines.com/uterus.html#endometrialcarc.
- ↑ URL: http://www.emedicine.com/med/topic2832.htm.
- ↑ Ayhan A, Taskiran C, Yuce K, Kucukali T (January 2003). "The prognostic value of nuclear grading and the revised FIGO grading of endometrial adenocarcinoma". Int. J. Gynecol. Pathol. 22 (1): 71–4. PMID 12496701.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 240. ISBN 978-0470519035.
- ↑ Winham, WM.; Lin, D.; Stone, PJ.; Nucci, MR.; Quick, CM. (Mar 2014). "Architectural versus nuclear atypia-defined FIGO grade 2 endometrial endometrioid adenocarcinoma (EEC): a clinicopathologic comparison of 154 cases with clinical follow-up.". Int J Gynecol Pathol 33 (2): 120-6. doi:10.1097/PGP.0b013e31828bb4ed. PMID 24487465.
- ↑ Chiesa-Vottero, AG.; Malpica, A.; Deavers, MT.; Broaddus, R.; Nuovo, GJ.; Silva, EG. (Jul 2007). "Immunohistochemical overexpression of p16 and p53 in uterine serous carcinoma and ovarian high-grade serous carcinoma.". Int J Gynecol Pathol 26 (3): 328-33. doi:10.1097/01.pgp.0000235065.31301.3e. PMID 17581420.
- ↑ Murray SK, Young RH, Scully RE (2003). "Unusual epithelial and stromal changes in myoinvasive endometrioid adenocarcinoma: a study of their frequency, associated diagnostic problems, and prognostic significance". Int J Gynecol Pathol 22: 324-333. doi:10.1097/01.pgp.0000092161.33490.a9. PMID 14501811.