Dysplastic nevus
| Dysplastic nevus | |
|---|---|
| Diagnosis in short | |
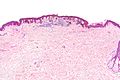
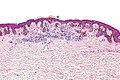
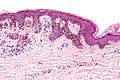
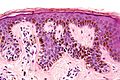
 Dysplastic nevus. H&E stain. | |
|
| |
| LM | "bridges" between the sides of the rete ridges, draping fibrous tissue/fibrous tissue wraps around the rete ridges ("lamellar fibrosis"), nuclear atypia - see grading section, +/-junctional component (cells in the epidermis at the DE junction) larger than the intradermal component - shoulder phenomenon |
| Subtypes | junctional, compound |
| LM DDx | melanoma in situ, malignant melanoma, compound melanocytic nevus, atypical lentiginous nevus |
| Stains | Fontana-Masson stain +ve |
| IHC | S-100 +ve, HMB-45 +ve, MART-1 +ve, MITF +ve |
| Gross | "ugly duckling sign" - lesion looks different than the rest, ABCD criteria of melanoma, usually greater than 5 mm |
| Site | skin - see melanocytic lesions |
|
| |
| Syndromes | dysplastic nevus syndrome |
|
| |
| Signs | ABCDEs of melanoma (asymmetry, border, colour, diameter, evolution) |
| Prevalence | common |
| Prognosis | benign, increased risk of melanoma |
| Clin. DDx | melanoma in situ, other pigmented lesions |
Dysplastic nevus, abbreviated DN, is a common melanocytic lesion that is closely associated with malignant melanoma.
It is also known as atypical nevus, dysplastic melanocytic nevus, Clark nevus, and nevus with architectural disorder.
In 1992, the term nevus with architectural disorder was recommended by the American National Institutes of Health (NIH);[1] however, it is not widely adopted.[2] Also, based on a 2003 survey, it is the preferred term by only 15% of dermatologists.[3]
General
- Benign.
- Dysplastic nevi are considered a risk factor for melanoma and may be a precursor of melanoma, as the name dysplastic nevus suggests.[4]
- Most melanoma cases do not have evidence of a pre-existing (dysplastic) nevus.[5]
- Large numbers of these nevi (10-100) are seen in dysplastic nevus syndrome.[6]
- Individuals with this syndrome have an increased risk of melanoma and approximately one third of their melanomas arise from a dysplastic nevus. The other two thirds arise de novo.
Clinical:[7]
- Associated with sun exposure.
Treatment:
- Dysplastic nevi with severe nuclear atypia are typically treated like melanoma in situ - complete excision with a 5 mm margin.[8]
- Dysplastic nevi with moderate nuclear atypia with margin involvement are re-excised.[8]
Gross
Features:[7]
- "Ugly duckling sign" - lesion looks different than the rest.
- ABCD criteria of melanoma.
- Tend to be greater than 5 mm - important.† [9]
Note:
- † Size matters - things smaller than 4 mm are usually not a dysplastic nevus.
Microscopic
Features:[10]
- Melanocytes "bridges" between sides of rete ridges.
- Joining of three or more adjacent rete ridges = suspicious for melanoma.[8]
- Draping fibrous tissue - "lamellar fibrosis" - collagen deep to epidermis.
- Nuclear atypia - often moderate (small nucleoli visible with 20x objective) - see grading section.
- +/-Junctional component (cells in the epidermis at the DE junction) larger than the intradermal component - shoulder phenomenon.
DDx:
- Melanoma in situ - especially on sun damaged skin (lentigo maligna).[11][12]
- Malignant melanoma - especially on sun damaged skin (lentigo maligna melanoma).
- Compound melanocytic nevus.
- Atypical lentiginous nevus.
Images
Grading
These lesions are often graded § :[13]
| Grade | Size of nucleus | Other features |
|---|---|---|
| Mild | 1x keratinocyte nucleus | no nucleoli/very small nucleoli †,[14] slight hyperchromasia |
| Moderate | 1-2x keratinocyte nucleus | small nucleoli †, irregular nuclear contours |
| Severe | >2x keratinocyte nucleus | prominent nucleoli †‡ |
† The sizes "very small", "small" and "prominent" are not defined; it is suggested that "very small" is visible with the 40x objective, "small" with the 20x objective and "prominent" with the 10x objective. Focal, rare small nucleoli are not significant; they can be seen in benign melanocytic nevi.
‡ Prominent nucleoli (alone) is considered enough to call "severe".[13]
Notes:
- § There is no consensus on this and practise (embarrassingly) is all over the map.[2]
- A two-tier grading system also exists (low-grade (leave it alone) / high-grade (cut it out)).
- Some pathologists do not grade dysplastic nevi.
- Normal melanocytes have a nucleus that is ~70% the size of a resting basal keratocyte nucleus.
Sign out
Compound
SKIN LESION, BACK, EXCISION: - DYSPLASTIC COMPOUND NEVUS WITH MILD CYTOLOGIC ATYPIA AND MILD ARCHITECTURAL ATYPIA, COMPLETELY EXCISED IN THE PLANE OF SECTION (2 MM CLEARANCE).
SKIN LESION, CENTRAL BACK, EXCISION: - DYSPLASTIC COMPOUND NEVUS WITH MILD CYTOLOGIC ATYPIA. - NEAREST MARGIN (LATERAL MARGIN) 6 MM.
Micro
The sections show hair-bearing skin with a compound melanocytic lesion. The epidermal component extends at least three rete ridges further than the dermal component (shoulder phenomenon). There is bridging between the sides of the rete ridges and lamellar fibrosis. The melanocyte nuclei are approximately the size of the keratinocyte nuclei, and do not have a prominent nucleolus (mild cytologic atypia).
There is no upward scatter of melanocytes and melanocytes in the dermis are mature. No mitotic activity is appreciated.
Junctional
SKIN LESION, LOWER BACK, EXCISION: - DYSPLASTIC JUNCTIONAL MELANOCYTIC NEVUS WITH MILD NUCLEAR ATYPIA. - NEAREST MARGIN (LATERAL MARGIN) 1 MM.
A comment for lesions with mild cytologic atypia:
COMMENT: Excision of any clinically apparent residual components of the lesion is suggested.
Micro
The sections show hair-bearing skin with a junctional melanocytic lesion. There is bridging between the sides of the rete ridges and lamellar fibrosis. The melanocyte nuclei are approximately the size of the keratinocyte nuclei, and do not have a prominent nucleolus (mild nuclear atypia).
There is no upward scatter of melanocytes. No mitotic activity is appreciated.
See also
References
- ↑ "Diagnosis and treatment of early melanoma. NIH Consensus Development Conference. January 27-29, 1992.". Consens Statement 10 (1): 1-25. PMID 1515516.
- ↑ 2.0 2.1 Elston, D. (Jul 2012). "Practical advice regarding problematic pigmented lesions.". J Am Acad Dermatol 67 (1): 148-55. doi:10.1016/j.jaad.2012.04.006. PMID 22703907.
- ↑ Fung, MA. (Oct 2003). "Terminology and management of dysplastic nevi: responses from 145 dermatologists.". Arch Dermatol 139 (10): 1374-5. doi:10.1001/archderm.139.10.1374. PMID 14568850.
- ↑ Rezze, GG.; Leon, A.; Duprat, J. (Dec 2010). "Dysplastic nevus (atypical nevus).". An Bras Dermatol 85 (6): 863-71. PMID 21308311.
- ↑ Longo, C.; Rito, C.; Beretti, F.; Cesinaro, AM.; Piñeiro-Maceira, J.; Seidenari, S.; Pellacani, G. (Sep 2011). "De novo melanoma and melanoma arising from pre-existing nevus: in vivo morphologic differences as evaluated by confocal microscopy.". J Am Acad Dermatol 65 (3): 604-14. doi:10.1016/j.jaad.2010.10.035. PMID 21715047.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 155600
- ↑ 7.0 7.1 Dediol, I.; Bulat, V.; Zivković, MV.; Marković, BM.; Situm, M. (Sep 2011). "Dysplastic nevus--risk factor or disguise for melanoma.". Coll Antropol 35 Suppl 2: 311-3. PMID 22220461.
- ↑ 8.0 8.1 8.2 Culpepper, KS.; Granter, SR.; McKee, PH. (Nov 2004). "My approach to atypical melanocytic lesions.". J Clin Pathol 57 (11): 1121-31. doi:10.1136/jcp.2003.008516. PMID 15509670.
- ↑ Barnhill, RL.; Hurwitz, S.; Duray, PH.; Arons, MS. (Feb 1988). "The dysplastic nevus: recognition and management.". Plast Reconstr Surg 81 (2): 280-9. PMID 3275948.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 502. ISBN 978-0781765275.
- ↑ Farrahi, F.; Egbert, BM.; Swetter, SM. (Jul 2005). "Histologic similarities between lentigo maligna and dysplastic nevus: importance of clinicopathologic distinction.". J Cutan Pathol 32 (6): 405-12. doi:10.1111/j.0303-6987.2005.00355.x. PMID 15953373.
- ↑ Edwards, SL.; Blessing, K. (Jun 2000). "Problematic pigmented lesions: approach to diagnosis.". J Clin Pathol 53 (6): 409-18. PMID 10911797.
- ↑ 13.0 13.1 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 447-8. ISBN 978-0443066542.
- ↑ Arumi-Uria, M.; McNutt, NS.; Finnerty, B. (Aug 2003). "Grading of atypia in nevi: correlation with melanoma risk.". Mod Pathol 16 (8): 764-71. doi:10.1097/01.MP.0000082394.91761.E5. PMID 12920220.