Trophoblast
Trophoblast is part of a normal pregnancy. Trophoblasts are derived from the conceptus, i.e. not maternal. Part of the trophoblast forms chorionic villi.
Tumours arising from the trophoblast are dealt with in gestational trophoblastic disease.
Trophoblast table
Based on Shih et al.:[1]
| Cytotrophoblast | Syncytiotrophoblast | Villous intermediate trophoblast |
Implantation site intermediate trophoblast |
Chorionic-type intermediate trophoblast | |
| Nuclear features | round, small | multinucleated | polyhedral | pleomorphic +/-multinucleation (occasional), +/-nucleoli |
round / polyhedral |
| Cell borders | well-defined | poorly defined (?) | well-defined | moderately-defined | poorly defined (?) |
| Cytoplasm | minimal, clear to granular | abundant, vacuolated, basophilic (???) | abundant & eosinophilic to clear | abundant & eosinophilic | abundant & eosinophilic |
| Location | villi - deep to syncytiotrophoblast |
villi - superficial to cytotrophoblast - nearest to maternal blood |
villi | implanatation site | chorion |
| Function | stem cell, produces beta-hCG[2] | produces hormones | ??? | anchor placenta | ??? |
| IHC | beta-hCG -ve (???), p63 +ve[3] | beta-hCG +ve | p63 +ve,[3] PLAP +ve | inhibin +ve, hPL +ve, beta-hCG -ve[4] CD146+,[5] p63 -ve | hPL +ve/-ve, p63 +ve, CD146 -ve |
| Image | ST (jhu.edu)[6] | CT (jhu.edu)[6] | (WC) | ||
| Associated tumour | Choriocarcinoma | Choriocarcinoma | ? | Placental site trophoblastic tumour | Epithelioid trophoblastic tumour |
hPL = human placental lactogen.
Notes:
- Keratin is positive in all trophoblastic tissue and negative in decidual tissue.[4]
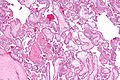
Chorionic villi
Chorionic villi 101
- Maternal blood is around villi.
- Fetal blood (nucleated (fetal) RBCs) in the villi.
Basic histology
- Syncytiotrophoblasts: outer layer of villus / closer to mother.
- Cytotrophoblasts: inner layer of villus / closer to fetus.
- Hofbauer cells: cells in the stroma of the villi, abundant bubbly cytoplasm - villus macrophages.[7]
Images
www:
Chorionic villi 102
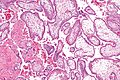
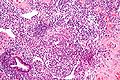
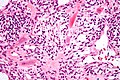
Syncytiotrophoblasts
- Multiple hyperchromatic nuclei, eosinophilic cytoplasm with vacuoles (contain hCG).
- Large + many irreg. or lobular hyperchromatic nuclei.
- Eosinophilic vacuolated cytoplasm (contains hCG).
- Closest to mom - covers cytotrophoblast.[8]
Cytotrophoblasts
- Polygonal shape, distinct borders, clear cytoplasm, in cords, single nucleus.
- Polygonal shaped cells in cords/masses.
- Distinct cell borders.
- Covered by syncytiobrophoblast[9] - closer to fetus than syncytiotrophoblasts.
- Clear cytoplasm.
- Single uniform nucleus.
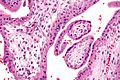
Age of villi
Young villi
- Few blood vessels, central location.
- Few syncytial knots.
Old villi
- Blood vessels present and at the periphery of villi.
- Syncytial knots.
Villi and age - table
| Gestational age | Nucleated RBCs | Cytotrophoblast / syncytiotrophoblast |
Villi size | Vessels | Other |
| First trimester (<13 weeks[10]) | present | both can be identified | large | few; location central | |
| Second trimester (>=13 weeks and <28 weeks[11]) | rare | cytotrophoblast difficult to identify; syncytial knots uncommon | intermediate | intermediate; location: central/periphery | |
| Third trimester | absent | cytotrophoblast indistinct; syncytial knots common | small | abundant; location: periphery of villi | focal calcifications |
Notes:
- The villi size is not very helpful in differentiating second and trimester placentas.
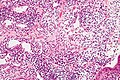
Intermediate trophoblast
- Abbreviated: IT.
General
- Thought to be the cell of origin for:[1]
- Exaggerated placental site (EPS).
- Placental site nodule (PSN).
- Placental site trophoblastic tumour (PSTT).
- Epithelioid trophoblastic tumour (ETT).
Subtypes
Three subtypes of IT are recognized:[1]
- Implanation site IT.
- Villous IT.
- Chorionic-type IT.
Microscopic
Features:
- Large cells.
- Eosinophilic cytoplasm.
- May be multi-nucleated.
Images
www:
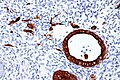
IHC
Features:[4]
- hPL (human placental lactogen) +ve.
- beta-hCG -ve.
- Keratin +ve.
- CK7 +ve.[12]
- EMA +ve in 2nd & 3rd trimester.
- CD146 +ve.[13]
Notes:
- Cytotrophoblast and syncytiotrophoblast - keratin +ve.[4]
See also
- Endometrium.
- Products of conception.
- Ectopic pregnancy.
- Choriocarcinoma.
- Arias-Stella reaction - benign atypical changes associated with chorionic tissue.
References
- ↑ 1.0 1.1 1.2 Shih IM, Kurman RJ (January 2001). "The pathology of intermediate trophoblastic tumors and tumor-like lesions". Int. J. Gynecol. Pathol. 20 (1): 31–47. PMID 11192071.
- ↑ Kovalevskaya, G.; Genbacev, O.; Fisher, SJ.; Caceres, E.; O'Connor, JF. (Aug 2002). "Trophoblast origin of hCG isoforms: cytotrophoblasts are the primary source of choriocarcinoma-like hCG.". Mol Cell Endocrinol 194 (1-2): 147-55. PMID 12242037.
- ↑ 3.0 3.1 Zhang, HJ.; Xue, WC.; Siu, MK.; Liao, XY.; Ngan, HY.; Cheung, AN. (Mar 2009). "P63 expression in gestational trophoblastic disease: correlation with proliferation and apoptotic dynamics.". Int J Gynecol Pathol 28 (2): 172-8. doi:10.1097/PGP.0b013e318189555b. PMID 19188816.
- ↑ 4.0 4.1 4.2 4.3 Yeh IT, O'Connor DM, Kurman RJ (May 1990). "Intermediate trophoblast: further immunocytochemical characterization". Mod. Pathol. 3 (3): 282–7. PMID 1694585.
- ↑ Shih, IM. (Sep 1999). "The role of CD146 (Mel-CAM) in biology and pathology.". J Pathol 189 (1): 4-11. doi:10.1002/(SICI)1096-9896(199909)189:14::AID-PATH3323.0.CO;2-P. PMID 10451481.
- ↑ 6.0 6.1 URL: http://pathology2.jhu.edu/trophoblast/introduction.cfm. Accessed on: 13 August 2011.
- ↑ Tang, Z.; Abrahams, VM.; Mor, G.; Guller, S. (Mar 2011). "Placental Hofbauer cells and complications of pregnancy.". Ann N Y Acad Sci 1221: 103-8. doi:10.1111/j.1749-6632.2010.05932.x. PMID 21401637.
- ↑ http://upload.wikimedia.org/wikipedia/commons/4/45/Gray37.png
- ↑ http://upload.wikimedia.org/wikipedia/commons/4/45/Gray37.png
- ↑ Haggerty, CL.; Seifert, ME.; Tang, G.; Olsen, J.; Bass, DC.; Karumanchi, SA.; Ness, RB. (Apr 2012). "Second trimester anti-angiogenic proteins and preeclampsia.". Pregnancy Hypertens 2 (2): 158-163. doi:10.1016/j.preghy.2012.01.005. PMID 22712058.
- ↑ Grewal, E.; Kansara, S.; Kachhawa, G.; Ammini, AC.; Kriplani, A.; Aggarwal, N.; Gupta, N.; Khadgawat, R. (May 2012). "Prediction of gestational diabetes mellitus at 24 to 28 weeks of gestation by using first-trimester insulin sensitivity indices in Asian Indian subjects.". Metabolism 61 (5): 715-20. doi:10.1016/j.metabol.2011.10.009. PMID 22146095.
- ↑ Trenkić, M.; Basić, M.; Milentijević, M.; Petrović, A.; Zivković, V.; Lazarević, V. (Nov 2008). "Immunohistohemical evidences of pregnancy in uterine curettage tissue by the use of a double immunocytochemical staining technique using cytokeratin 7 and vimentin antibodies.". Vojnosanit Pregl 65 (11): 810-3. PMID 19069710.
- ↑ URL: http://www.epitomics.com/diagnostics/product/5618. Accessed on: 14 August 2011.