Difference between revisions of "Pulmonary embolism"
Jump to navigation
Jump to search
| Line 6: | Line 6: | ||
*Pulmonary bone marrow embolism. | *Pulmonary bone marrow embolism. | ||
*Pulmonary tumour embolism. | *Pulmonary tumour embolism. | ||
*Pulmonary amniotic fluid embolism. | |||
PE usually refers to '''pulmonary venous thromboembolism''', abbreviated '''VTE''', if not otherwise specified. | PE usually refers to '''pulmonary venous thromboembolism''', abbreviated '''VTE''', if not otherwise specified. | ||
Revision as of 07:32, 17 November 2014
Pulmonary embolism, abbreviated PE, is often on the differential in autopsies, as it is not easy to diagnose clinically. Pulmonary embolism is a non-specific term; it may refer to a number of things, including:
- Pulmonary venous thromboembolism.
- Pulmonary fat embolism.
- Pulmonary foreign body embolism.
- Pulmonary septic embolism.
- Pulmonary bone marrow embolism.
- Pulmonary tumour embolism.
- Pulmonary amniotic fluid embolism.
PE usually refers to pulmonary venous thromboembolism, abbreviated VTE, if not otherwise specified.
General
- Relatively uncommon ~ 1 in 1000 adults per year.[1]
- Diagnosis in life dependent on strong clinical suspicion and radiology.
Clinical
- Shortness of breath (dyspnea) - classic symptom.
- Tachycardia.
- Chest pain.
- Findings associated with deep vein thrombosis.
- Leg pain.
- Leg swelling.
Notes:
- Venous thrombosis OR~=12 for PE.[2]
Mechanism
The classic factors are given by Virchow's triad:[3][1]
- Hypercoagulability.
- Endothelial dysfunction/injury.
- Stasis.
Note:
- The triad has a limited practical use. Like many questions about mechanism, the greatest utility, as far as I can determine, is pimping medical students and residents.
Risks factors venous thromboembolism
A general mnemonic for hypercoagulable states PIANO:[4]
- Pregnancy.
- Immobility.
- Accidental injury.
- Nephrotic syndrome.
- Oral contraceptive pills.
Hypercoagulable states due to intrinsic causes (memory device CALM SHAPES):[5]
- Protein C deficiency.
- Antiphospholipid antibody syndrome (APLA).
- Leiden factor V deficiency.
- Malignancy.
- Protein S deficiency.
- Homocystinemia.
- Antithrombin III deficiency.
- Prothrombin G20210A.[6]
- Excess factor VIII.
- Sticky platelet syndrome.
Gross (VTE)
Features:
- Intravascular spaghetti (multiple cylindrical clots - from smaller vessels) with cream sauce (gray fibrin).
- Leg swelling.
- Lines of Zahn.[7]
- Pale layers consisting of platelets and fibrin alternating with layers of RBCs; components layer during blood flow.
Notes:
- Post-mortem thrombi: one (superior) yellow portion (called "chicken fat") and one (dependent) red portion (RBCs); components layer due to gravity.
Pre- and post-mortem clots
| Feature/time | Pre-mortem | Post-mortem |
| Shininess | dull | shiny |
| Adherent to wall | yes | no |
| Colour | gray | dark purple or bilayered red/yellow |
| Pressurized | yes; "ejects itself" from lumen | no; needs to be pulled-out |
| Consistency -elastic modulus (E) -fracture toughness (K) |
firm (high E) brittle (low K) |
jello (low E) elastic (high K) |
| Image - gross | thrombus (pathguy.com), thrombus (thrombosisadviser.com) |
coronary thrombus (luc.edu)[8] |
| Image - micro. | pre- & post-mortem (elsevier.es)[9] | thrombus (oxfordjournals.org), thrombi (ucsf.edu) |
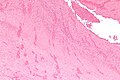
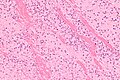
Microscopic (VTE)
Features:
- Layers consisting of platelets and fibrin alternating with layers of RBCs - known as Lines of Zahn.[7]
Note:
- Multiple laminations (layers), in general, suggest that clot was formed in a dynamic environment, i.e. in the context of blood flow.
Images
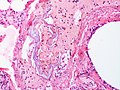
Microscopic (fat embolism)
Features:
- Fat in vessels.
Images:
Microscopic (amniotic fluid)
Images:
See also
References
- ↑ 1.0 1.1 Meetoo, D.. "In too deep: understanding, detecting and managing DVT.". Br J Nurs 19 (16): 1021-7. PMID 20852464.
- ↑ Reissig A, Haase U, Schulze E, Lehmann T, Kroegel C (July 2010). "[Diagnosis and therapy of pulmonary embolism prior to death]" (in German). Dtsch. Med. Wochenschr. 135 (30): 1477–83. doi:10.1055/s-0030-1262435. PMID 20648405.
- ↑ Reitsma, PH.; Versteeg, HH.; Middeldorp, S. (Mar 2012). "Mechanistic view of risk factors for venous thromboembolism.". Arterioscler Thromb Vasc Biol 32 (3): 563-8. doi:10.1161/ATVBAHA.111.242818. PMID 22345594.
- ↑ URL: http://www.usmle-forums.com/usmle-step-1-mnemonics/252-causes-hypercoagulable-states.html. Accessed on: 8 December 2011.
- ↑ Thomas RH (November 2001). "Hypercoagulability syndromes". Arch. Intern. Med. 161 (20): 2433–9. PMID 11700155. http://archinte.highwire.org/cgi/content/full/161/20/2433.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 176930
- ↑ 7.0 7.1 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 124. ISBN 978-1416031215.
- ↑ URL: http://www.meddean.luc.edu/lumen/meded/mech/cases/case1/list.htm. Accessed on 8 October 2010.
- ↑ URL: http://www.elsevier.es/cardio_eng/ctl_servlet?_f=40&ident=13142654. Accessed on: 8 October 2010.
- ↑ URL: http://library.med.utah.edu/WebPath/EXAM/IMGQUIZ/fofrm.html. Accessed on: 6 December 2010.