Difference between revisions of "Prostate cancer grading"
(→Order of Gleason score components changed: +upgrade based on nodule) |
|||
| Line 321: | Line 321: | ||
*[[Prostate cancer staging]]. | *[[Prostate cancer staging]]. | ||
*[[Cancer staging systems]]. | *[[Cancer staging systems]]. | ||
*[[Cribriform pattern within invasive prostate carcinoma]]. | |||
==References== | ==References== | ||
Revision as of 20:36, 13 April 2018
This article deals with prostate cancer grading.
It covers the Gleason system and the proposed Prostate cancer grading system endorsed by the WHO.
Prostate cancer is dealt with in the prostate cancer article.
Gleason grading system
- AKA modified Gleason grading system.
- It could be called the modified modified Gleason grading system, as it has been changed twice.
Overview
- There is consensus on how it is done.[1]
- Score range: 6-10.
- Technically 2-10... but almost no one uses 2-5.
- Reported on biopsy (and TURP) as: (primary pattern) + (highest non-primary pattern) = sum.
- Gleason score 3+4=7 means: pattern 3 is present and dominant, pattern 4 is the remainder of the tumour - but present in a lesser amount than pattern 3.
- Gleason score 4+5=9 means: pattern 4 is present and dominant, pattern 5 is present in a lesser amount that pattern 4. Pattern 3 may be present in a quantity less than pattern 4 or is absent.
- If a lower grade pattern is present and less than 5% it is ignored.
- A biopsy with 98% Gleason pattern 4 and 2% Gleason pattern 3 would be graded as 8/10 (4+4).
- Reported as on prostatectomies as: (primary pattern) + (secondary pattern) = sum, (tertiary pattern)
Tertiary Gleason pattern
- Unfortunately there is no consensus definition for tertiary Gleason pattern.[2]
- The Foundation series GU book (1st Ed.) defines Tertiary Gleason pattern as:[3] a pattern that is seen in less than 5% of the tumour that is of a higher grade than the two dominant patterns.
- Koloffa et al[2] notes that some define it as: the third most prevalent pattern and most require that it is a higher grade than the two dominant patterns.
- Parsed with the all the subtleties a working definition could be: The third most prevalent pattern and a higher grade than the two dominant patterns or a pattern that is seen in less than 5% of the tumour and of higher grade than one pattern that comprises >95% of the tumour.
Significance:
- The presence of a tertiary patterns adversely affect the prognosis; however, the prognosis is not as bad as when the tertiary pattern is the secondary pattern, i.e. 3+4 tertiary 5 has a better prognosis than 3+5 (with some small amount of pattern 4).[3]
Use:
- It is only used for prostatectomies.
Examples
- A biopsy with 80% pattern 4, 16% pattern 3 and 4% pattern 5... would be reported as: 4+5=9.
- A biopsy with 92% pattern 4, and 8% pattern 3... would be reported as: 4+3=7.
- A biopsy with 98% pattern 4, and 2% pattern 3... would be reported as: 4+4=8.
- A prostatectomy with 80% pattern 4, 16% pattern 3 and 4% pattern 5... would be reported as: 4+3=7 with tertiary pattern 5.
Note:
- Based on the various definitions of tertiary pattern:[2]
- A prostatectomy with 75% pattern 4, 15% pattern 3 and 10% pattern 5 could be reported as: 4+3=7 with tertiary pattern 5 or 4+5=9.
- As there is no consensus on this, it is probably best to report the percentages of the various patterns if this situation arises.
- A prostatectomy with 75% pattern 4, 15% pattern 3 and 10% pattern 5 could be reported as: 4+3=7 with tertiary pattern 5 or 4+5=9.
Gleason patterns (modified)
Gleason pattern 1 & 2
- Use strongly discouraged by a number of GU pathology experts.
Notes:
- Gleason pattern 1 - probably represents what today would be called adenosis.
- Should never be used.
- Gleason pattern 2 - used by few GU pathology experts occasionally.
- Generally, should not be diagnosed on core biopsies.[4]
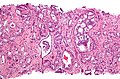
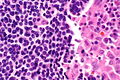
Gleason pattern 3
- Glands smaller than normal prostate glands + loss of epithelial folding.
- Can draw a line around each gland.
- May have gland branching.
- Glands have a X, U, V or Y shape.
Notes:
- Gland lumina should be seen.
- All cribriform is now, generally, classified as Gleason pattern 4.[4]
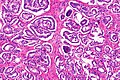
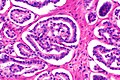
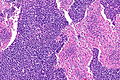
Gleason pattern 4
- Loss of gland lumina.
- Gland fusion.
- Benign looking cords ('hypernephroid pattern').
- Cribriform.
- Glomeruloid pattern - resembles a glomerulus.
Notes:
- One gland is not enough to call Gleason 4.
Images
www:
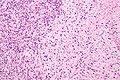
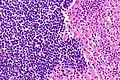
Gleason pattern 5
- Sheets.
- Must be differentiated from intraductal growth (which like in the breast are well circumscribed nests).
- Single cells.
- May be confused with stromal/lymphocytic infiltration.
- Look for nucleoli, cells should be round (prostatic stroma cells are spindle cells).
- May be confused with stromal/lymphocytic infiltration.
- Cords (strands).
- Line of cells.
- Should not be intermixed with clumps of cells (pattern 4).
- Nests of cells with necrosis (at the centre) (comedonecrosis) or (intraluminal) necrosis in a cribriform pattern.[1]
- Necrosis:
- Nuclear changes:
- Karyorrhexis (nuclear fragmentation).
- Pynosis (nuclear shrinkage).
- Karyolysis (nuclear dissolution).
- Cell ghosts (cells without a nucleus).
- Nuclear changes:
- Necrosis:
Notes:
- Pattern 5 may be under-diagnosed.
- Single cells is the most commonly missed pattern.[5]
Images
www:
Gleason pattern for special types
Special types of prostate cancer have suggested Gleason patterns:[6]
| Special type | Gleason pattern | Comment |
|---|---|---|
| Ductal carcinoma | 4 | may be graded 3 or 5[7] |
| Mucinous carcinoma | 3 or 4 - dependent on morphology[8][9] | some advocate grade 4[6] |
| Sarcomatoid carcinoma | 5 | glands graded separately |
| Signet ring cell carcinoma | 5 | |
| Small cell carcinoma | not graded (ISUP 2005 consensus[1]) | may be graded 5[7] |
| Adenosquamous and squamous carcinoma | not graded | |
| Lymphoepithelioma-like carcinoma | not graded | |
| Adenoid cystic carcinoma | not graded | |
| Urothelial carcinoma | not graded | |
| Undifferentiated carcinoma, NOS | not graded |
How to remember the ones that aren't graded - think of Ur Lung carcinomas (Urothelial carcinoma, Lymphoepithelioma-like carcinoma):
- Small cell carcinoma.
- Squamous cell carcinoma.
- Adenosquamous carcinoma.
- Adenoid cystic carcinoma.
Biopsy-prostatectomy concordance of Gleason score
- Discordance is common.
- Upgrade on prostatectomy: 25-40%.
- Downgrade on prostatectomy: 5-15%.
Selected studies on concordance:
| Study | Upgrade | Downgrade | Notes |
|---|---|---|---|
| Sfoungaristos et al.[10] | 42.1% | 13.7% | high volume of tumour predicts upgrade |
| Thomas et al.[11] | 38.1% | 4.7% | |
| Truesdale et al.[12] | 23% | 11% |
Sign out
Upgrading
Gleason score upgrading on prostatectomy is considered relatively common; it is reported to occur in 23% to 42.1% of cases.[1][2] 1. BJU Int. 2011 107 (5): 749-54. 2. Can Urol Assoc J. 2012 Jan 24:1-5.
Downgrading
Gleason score downgrading on prostatectomy is considered uncommon; however, it is reported in 4.7% to 13.7% of cases.[1][2] 1. BJU Int. 2012 Jan; 109(2):214-9. 2. Can Urol Assoc J. 2012 Jan; 24;1-5.
Order of Gleason score components changed
COMMENT: The change in the order of the Gleason score components (3+4 on prostatectomy versus 4+3 on core biopsy) may be explained by sampling.
Separate nodule upgrades prostatectomy
A tumour nodule in the left mid portion of the gland (1.2 cm) is predominantly 4+3; the Gleason score for the case is assigned on the basis of the tumour nodule as Gleason score 7/10 (4+3). Overall, Gleason pattern 3 represents 65% of the cancer in the prostate, and Gleason pattern 4 represents 35% of the cancer in the prostate.
Prostate cancer grading system endorsed by the WHO
- AKA WHO prostate cancer grading system or WHO system.
- AKA ISUP prostate grading.
- AKA grade groupings.
- AKA prognostic Gleason grade groupings.
- AKA a contemporary prostate cancer grading system, abbreviated CPCGS.
- AKA Gleason group.[13]
This system has been proposed. Currently, it is not widely used. The name of the system is not completely settled. This system has been proposed. Currently, it is not widely used. The name of the system is not completely settled.
WHO prostate cancer grading system & Gleason score
Proposed new system (endorsed by the WHO[14]) and old (modified) Gleason score:[15][16]
| WHO grade | Gleason score |
|---|---|
| I | 6 (3+3) |
| II | 3+4 |
| III | 4+3 |
| IV | 8 (4+4, 3+5, 5+3) |
| V | 9 or 10 (4+5, 5+4, 5+5) |
Rationale:
- Patients won't be told they have a 6 out of 10 cancer, and then think it is an intermediate grade cancer that is worrisome. Instead, they will be told they have a 1 out of 5 cancer.[15]
- Gleason score 7 is split into two separate groups, as the follow-up data suggests they should be.
Prognostication
Recurrence free progression stratified by the system endorsed by the WHO:[16]
| WHO grade | Hazard ratio compared to Group I |
|---|---|
| I | (1.0) |
| II | 1.9 |
| III | 5.1 |
| IV | 8.0 |
| V | 11.7 |
Sign out
- The language is still evolving as this is relatively new.
- As of 2017, many pathologists continue to predominantly use (modified) Gleason grading, and add a comment about (the equivalent grade in) the new grading system.
Reporting examples
Within a synoptic report:
Grade group: Grade Group 3, Gleason score 4+3=7.
As a comment:
The World Health Organization (WHO) grade is: 3 out of 5. Gleason pattern 3 represents 30% of the tumour, and Gleason pattern 4 represents 70% of the tumour.
Alternates
The World Health Organization (WHO) prostate cancer grade is: 3 out of 5. Gleason pattern 3 represents 30% of the tumour, and Gleason pattern 4 represents 70% of the tumour.
Gleason pattern 3 represents 30% of the tumour, and Gleason pattern 4 represents 70% of the tumour. The World Health Organization (WHO) endorsed prostate cancer grade grouping is: 3 out of 5.
See also
- Prostate cancer.
- Prostate cancer staging.
- Cancer staging systems.
- Cribriform pattern within invasive prostate carcinoma.
References
- ↑ 1.0 1.1 1.2 Epstein, JI.; Allsbrook, WC.; Amin, MB.; Egevad, LL. (Sep 2005). "The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma.". Am J Surg Pathol 29 (9): 1228-42. PMID 16096414.
- ↑ 2.0 2.1 2.2 Koloffa, ZB; Hamstrab, DA; Weia, JT; Montgomerya, JS et al (2015). "Impact of tertiary Gleason pattern 5 on prostate cancer aggressiveness: Lessons from a contemporary single institution radical prostatectomy series". Asian Journal of Urology 2 (1): 53–58. doi:10.1016/j.ajur.2015.04.007. http://www.sciencedirect.com/science/article/pii/S2214388215000302.
- ↑ 3.0 3.1 Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 72. ISBN 978-0443066771.
- ↑ 4.0 4.1 Epstein, JI. (Feb 2010). "An update of the Gleason grading system.". J Urol 183 (2): 433-40. doi:10.1016/j.juro.2009.10.046. PMID 20006878.
- ↑ Fajardo, DA.; Miyamoto, H.; Miller, JS.; Lee, TK.; Epstein, JI. (Nov 2011). "Identification of Gleason pattern 5 on prostatic needle core biopsy: frequency of underdiagnosis and relation to morphology.". Am J Surg Pathol 35 (11): 1706-11. doi:10.1097/PAS.0b013e318228571d. PMID 21997691.
- ↑ 6.0 6.1 Grignon DJ (March 2004). "Unusual subtypes of prostate cancer". Mod. Pathol. 17 (3): 316–27. doi:10.1038/modpathol.3800052. PMID 14976541.
- ↑ 7.0 7.1 URL: https://www.bostwicklaboratories.com/global/physicians/medical-library/articles/gleason-grading.aspx. Accessed on: 26 November 2011.
- ↑ Osunkoya, AO.; Adsay, NV.; Cohen, C.; Epstein, JI.; Smith, SL. (Jul 2008). "MUC2 expression in primary mucinous and nonmucinous adenocarcinoma of the prostate: an analysis of 50 cases on radical prostatectomy.". Mod Pathol 21 (7): 789-94. doi:10.1038/modpathol.2008.47. PMID 18487999.
- ↑ Osunkoya, AO.; Nielsen, ME.; Epstein, JI. (Mar 2008). "Prognosis of mucinous adenocarcinoma of the prostate treated by radical prostatectomy: a study of 47 cases.". Am J Surg Pathol 32 (3): 468-72. doi:10.1097/PAS.0b013e3181589f72. PMID 18300802.
- ↑ Sfoungaristos, S.; Perimenis, P. (Jan 2012). "Clinical and pathological variables that predict changes in tumour grade after radical prostatectomy in patients with prostate cancer.". Can Urol Assoc J: 1-5. doi:10.5489/cuaj.11067. PMID 22277633.
- ↑ Thomas, C.; Pfirrmann, K.; Pieles, F.; Bogumil, A.; Gillitzer, R.; Wiesner, C.; Thüroff, JW.; Melchior, SW. (Jan 2012). "Predictors for clinically relevant Gleason score upgrade in patients undergoing radical prostatectomy.". BJU Int 109 (2): 214-9. doi:10.1111/j.1464-410X.2011.10187.x. PMID 21592293.
- ↑ Truesdale, MD.; Cheetham, PJ.; Turk, AT.; Sartori, S.; Hruby, GW.; Dinneen, EP.; Benson, MC.; Badani, KK. (Mar 2011). "Gleason score concordance on biopsy-confirmed prostate cancer: is pathological re-evaluation necessary prior to radical prostatectomy?". BJU Int 107 (5): 749-54. doi:10.1111/j.1464-410X.2010.09570.x. PMID 20840549.
- ↑ URL: http://www.cancer.net/cancer-types/prostate-cancer/stages-and-grades. Accessed on: May 1, 2017.
- ↑ Epstein, JI.; Egevad, L.; Amin, MB.; Delahunt, B.; Srigley, JR.; Humphrey, PA. (Feb 2016). "The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of Grading Patterns and Proposal for a New Grading System.". Am J Surg Pathol 40 (2): 244-52. doi:10.1097/PAS.0000000000000530. PMID 26492179.
- ↑ 15.0 15.1 URL: http://urology.jhu.edu/newsletter/2014/prostate_cancer_2014_19.php. Accessed on: 28 March 2015.
- ↑ 16.0 16.1 Epstein, JI.; Zelefsky, MJ.; Sjoberg, DD.; Nelson, JB.; Egevad, L.; Magi-Galluzzi, C.; Vickers, AJ.; Parwani, AV. et al. (Jul 2015). "A Contemporary Prostate Cancer Grading System: A Validated Alternative to the Gleason Score.". Eur Urol. doi:10.1016/j.eururo.2015.06.046. PMID 26166626.