Paraganglioma
| Paraganglioma | |
|---|---|
| Diagnosis in short | |
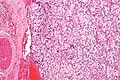
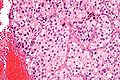
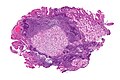
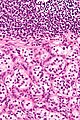
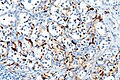
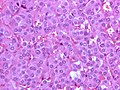
 Paraganglioma. H&E stain. | |
|
| |
| LM | Zellballen (nests of cells), fibrovascular septae, salt-and-pepper nuclei, +/-hemorrhage (very common) |
| LM DDx | neuroendocrine tumour, pheochromocytoma (paraganglioma of the adrenal gland), gangliocytic paraganglioma |
| IHC | chromogranin +ve, synaptophysin +ve, CD56 +ve |
| Gross | dusky colour |
| Site | abdomen (adrenal gland paraganglioma = pheochromocytoma), head and neck (carotid body tumour) |
|
| |
| Syndromes | von Hippel Lindau, hereditary paragangliomatosis, neurofibromatosis type 1 (von Recklinghausen disease), MEN 2A, MEN 2B, Carney-Stratakis syndrome, Carney triad |
|
| |
| Prevalence | uncommon |
| Prognosis | usually good, rarely malignant |
Paraganglioma is a rare tumour arising from the paraganglion. A paraganglioma arising in the adrenal gland is known as a pheochromocytoma.
General
- Definition: tumour of paraganglion.
- Can be sympathetic or parasympathetic.
- Most common paraganglioma = pheochromocytoma.[1]
- Head & neck most common site - after abdomen.
- Carotid body tumour = paraganglioma of carotid body.
Epidemiology
- Rare.
- Rarely malignant.
Familial syndromes associated with paragangliomas:[2]
- von Hippel Lindau.
- Hereditary paragangliomatosis.
- Neurofibromatosis type 1 (von Recklinghausen disease).
- MEN 2A.
- MEN 2B.
- Carney-Stratakis syndrome - GISTs and paraganglioma.[3]
- SDH mutation associated (SDHB, SDHC and SDHD).[4]
Other associations - not proven to be genetic:
Clinical
- 10% bilateral, multiple, familial, pediatric and malignant.[5]
- Not quite true... more than 10% are familial - see pheochromocytoma article.
Gross
- Dusky colour.
Note:
- Pheo (in pheochromocytoma) is dusky; chromo is colour.
Image:
Microscopic
Features:[6]
- Zellballen - nests of cells - key low power feature.
- Zellballen is "cell balls" in German.
- Fibrovascular septae.
- Finely granular cytoplasm (salt-and-pepper nuclei).
- +/-Hemorrhage - very common.
DDx:
- Neuroendocrine tumour - nests surrounded by stroma/do not touch.
- Pheochromocytoma - paraganglioma of the adrenal gland.
- Gangliocytic paraganglioma - has schwannian component and ganglion cells, usu. duodenum.
Images
Carotid body tumour:
Duodenal paraganglioma - uncommon location:
Other:
www:
IHC
Features:[7]
EM
Features:[8]
- Neurosecretory granules.
- Electron dense core.
- Typically perinuclear location.
Image:
See also
References
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 327. ISBN 978-0443066856.
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 328. ISBN 978-0443066856.
- ↑ Blay, JY.; Blomqvist, C.; Bonvalot, S.; Boukovinas, I.; Casali, PG.; De Alava, E.; Dei Tos, AP.; Dirksen, U. et al. (Oct 2012). "Gastrointestinal stromal tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up.". Ann Oncol 23 Suppl 7: vii49-55. doi:10.1093/annonc/mds252. PMID 22997454. http://annonc.oxfordjournals.org/content/23/suppl_7/vii49.full.
- ↑ Lefebvre, M.; Foulkes, WD. (Feb 2014). "Pheochromocytoma and paraganglioma syndromes: genetics and management update.". Curr Oncol 21 (1): e8-e17. doi:10.3747/co.21.1579. PMID 24523625.
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 327. ISBN 978-0443066856.
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 329-332. ISBN 978-0443066856.
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 335. ISBN 978-0443066856.
- ↑ 8.0 8.1 URL: http://path.upmc.edu/cases/case408.html. Accessed on: 16 January 2012.