Difference between revisions of "Ovary"
Jump to navigation
Jump to search
(→Benign mesothelial inclusion cyst: +pregnancy luteoma) |
m |
||
| (24 intermediate revisions by one other user not shown) | |||
| Line 1: | Line 1: | ||
The '''ovary''' has a wealth of pathology. It has benign tumours and malignant ones. | The '''ovary''' has a wealth of [[pathology]]. It has benign tumours and malignant ones. It is a significant part of [[gynecologic pathology]]. | ||
=Normal ovary= | |||
*Corpora albicans - pale/white body with lobulated contour. | *Corpora albicans - pale/white body with lobulated contour. | ||
**Involuted corpus luteum. | |||
**Not seen pre-pubertal. | |||
**Number increase with age. | |||
*Ovarian follicles. | *Ovarian follicles. | ||
*Stroma - '''hyperchromatic''' - spindle morphology, whorling. | *Stroma - '''hyperchromatic''' - spindle morphology, whorling. | ||
**If the cells have a round morphology... think about endometriosis. | **If the cells have a round morphology... think about [[endometriosis]]. | ||
===Images=== | |||
www: | |||
*[http://media.photobucket.com/image/ovary%20histology/lovesthesunset/anatomy%20and%20physiology/ovarycorpusluteum.jpg Ovarian stroma (photobucket.com)]. | *[http://media.photobucket.com/image/ovary%20histology/lovesthesunset/anatomy%20and%20physiology/ovarycorpusluteum.jpg Ovarian stroma (photobucket.com)]. | ||
<gallery> | |||
Image:Corpus_albicans.JPG| Corpus albicans. (WC) | |||
</gallery> | |||
== | =Cysts - overview= | ||
General | ==General== | ||
*Very common. | *Very common. | ||
| Line 23: | Line 30: | ||
*Endometrioma (see [[endometriosis]]). | *Endometrioma (see [[endometriosis]]). | ||
*Simple cyst. | *Simple cyst. | ||
*[[Corpus luteum cyst]]. | |||
*Cancerous cyst (see [[ovarian cancer]]). | *Cancerous cyst (see [[ovarian cancer]]). | ||
Notes | Notes: | ||
*Epithelium is often lost in processing - may make interpretation challenging | *Epithelium is often lost in processing - may make interpretation challenging | ||
*Ovarian surface epithelium (previously call ''germinal epithelium'') - covers the ovary | *Ovarian surface epithelium (previously call ''germinal epithelium'') - covers the ovary | ||
**Cuboidal/flat epithelium.<ref>{{cite journal |author=Auersperg N, Wong AS, Choi KC, Kang SK, Leung PC |title=Ovarian surface epithelium: biology, endocrinology, and pathology |journal=Endocr. Rev. |volume=22 |issue=2 |pages=255–88 |year=2001 |month=April |pmid=11294827 |doi= |url=http://edrv.endojournals.org/cgi/pmidlookup?view=long&pmid=11294827}}</ref> | **Cuboidal/flat epithelium.<ref>{{cite journal |author=Auersperg N, Wong AS, Choi KC, Kang SK, Leung PC |title=Ovarian surface epithelium: biology, endocrinology, and pathology |journal=Endocr. Rev. |volume=22 |issue=2 |pages=255–88 |year=2001 |month=April |pmid=11294827 |doi= |url=http://edrv.endojournals.org/cgi/pmidlookup?view=long&pmid=11294827}}</ref> | ||
**Has ovarian stroma underneath. | **Has ovarian stroma underneath. | ||
** | **Hobnail morphology (free surface larger than basement membrane surface).<ref>ALS. 5 February 2009.</ref> | ||
Ovarian surface vs. mesothelium: | Ovarian surface vs. mesothelium: | ||
| Line 36: | Line 44: | ||
*Image: [http://internetattitude.com/bioimage/OldSlides/bio231histo800x600/Mesothelium%20Simple%20Squamous%20x440.JPG mesothelium] - internetattitude.com. | *Image: [http://internetattitude.com/bioimage/OldSlides/bio231histo800x600/Mesothelium%20Simple%20Squamous%20x440.JPG mesothelium] - internetattitude.com. | ||
=Specific benign diagnoses= | |||
==Endometriosis== | ==Endometriosis== | ||
{{main|Endometriosis}} | {{main|Endometriosis}} | ||
== | ==Corpus luteum cyst== | ||
===General=== | |||
*Normal in childbearing age women. | |||
===Gross=== | |||
*Classically yellow. | |||
===Microscopic=== | |||
Features: | |||
*Pseudocyst lined by stratified, pale staining (luteinized) cells. | |||
*+/-Hemorrhagic centre. | |||
Images: | |||
*[http://commons.wikimedia.org/wiki/File:Luteinized_follicular_cyst.jpg Luteinized cells in a follicular cyst (WC)]. | |||
*[http://php.med.unsw.edu.au/embryology/index.php?title=File:Ovary_corpus_luteum.jpg Corpus luteum (unsw.edu.au)]. | |||
==Benign mesothelial inclusion cyst== | ==Benign mesothelial inclusion cyst== | ||
=== | *[[AKA]] ''mesothelial inclusion cyst''. | ||
* | *[[AKA]] ''[[peritoneal inclusion cyst]]''.{{fact}} | ||
*[[AKA]] ''cortical inclusion cyst''.<ref name=pmid11207821>{{Cite journal | last1 = Feeley | first1 = KM. | last2 = Wells | first2 = M. | title = Precursor lesions of ovarian epithelial malignancy. | journal = Histopathology | volume = 38 | issue = 2 | pages = 87-95 | month = Feb | year = 2001 | doi = | PMID = 11207821 }}</ref>{{fact}} | |||
*[[AKA]] ''surface epithelial inclusion cyst''. | |||
===General=== | |||
*May be found incidentally, e.g. during C-section. | *May be found incidentally, e.g. during C-section. | ||
Epidemiology: | |||
*Associated with previous surgery. | |||
===Gross=== | ===Gross=== | ||
| Line 58: | Line 85: | ||
*Benign mesothelium. | *Benign mesothelium. | ||
**Single layer of squamoid or cuboid mesothelial cells.<ref name=pmid16092670/> | **Single layer of squamoid or cuboid mesothelial cells.<ref name=pmid16092670/> | ||
DDx: | |||
*[[Serous cystadenoma of the ovary]] - must be >=1 cm.<ref name=Ref_GP384>{{Ref GP|384}}</ref> | |||
Image: | |||
*[http://www.jultrasoundmed.org/content/27/3/327/F3.expansion.html Cortical inclusion cyst (jultrasounmed.org)].<ref name=pmid18314510>{{Cite journal | last1 = Asch | first1 = E. | last2 = Levine | first2 = D. | last3 = Kim | first3 = Y. | last4 = Hecht | first4 = JL. | title = Histologic, surgical, and imaging correlations of adnexal masses. | journal = J Ultrasound Med | volume = 27 | issue = 3 | pages = 327-42 | month = Mar | year = 2008 | doi = | PMID = 18314510 }}</ref> | |||
===[[IHC]]=== | ===[[IHC]]=== | ||
*[[CK]] +ve, [[calretinin]] +ve.<ref name=pmid16092670/> | *[[CK]] +ve, [[calretinin]] +ve.<ref name=pmid16092670/> | ||
===Sign out=== | |||
<pre> | |||
OVARY, LEFT, BIOPSY: | |||
- BENIGN CORTICAL INCLUSION CYST. | |||
</pre> | |||
==Ovarian infarct== | |||
{{Main|Ovarian infarct}} | |||
==Pregnancy luteoma== | ==Pregnancy luteoma== | ||
*[[AKA]] ''luteoma of [[pregnancy]]''. | |||
* | {{Main|Pregnancy luteoma}} | ||
== | =Ovarian tumours= | ||
{{main|Ovarian tumours}} | |||
For a ''very'' brief overview of gynecologic tumours see: ''[[Gynecologic pathology]]''. | |||
=See also= | |||
*[[Gynecologic pathology]]. | *[[Gynecologic pathology]]. | ||
*[[Testis]]. | *[[Testis]]. | ||
=References= | |||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Gynecologic pathology]] | [[Category:Gynecologic pathology]] | ||
Latest revision as of 10:08, 5 August 2017
The ovary has a wealth of pathology. It has benign tumours and malignant ones. It is a significant part of gynecologic pathology.
Normal ovary
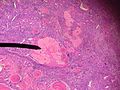
- Corpora albicans - pale/white body with lobulated contour.
- Involuted corpus luteum.
- Not seen pre-pubertal.
- Number increase with age.
- Ovarian follicles.
- Stroma - hyperchromatic - spindle morphology, whorling.
- If the cells have a round morphology... think about endometriosis.
Images
www:
Cysts - overview
General
- Very common.
Most common:
- Serous cystadenoma.
- Usually uniloculated.
- Morphology: ciliated, columnar.
- Mucinous cystadenoma.
- Usually multiloculated.[1]
- Memory device: multiloculated = mucinous.
- Usually multiloculated.[1]
- Endometrioma (see endometriosis).
- Simple cyst.
- Corpus luteum cyst.
- Cancerous cyst (see ovarian cancer).
Notes:
- Epithelium is often lost in processing - may make interpretation challenging
- Ovarian surface epithelium (previously call germinal epithelium) - covers the ovary
Ovarian surface vs. mesothelium:
- Image: ovarian surface epithelium - endojournals.org.
- Image: mesothelium - internetattitude.com.
Specific benign diagnoses
Endometriosis
Main article: Endometriosis
Corpus luteum cyst
General
- Normal in childbearing age women.
Gross
- Classically yellow.
Microscopic
Features:
- Pseudocyst lined by stratified, pale staining (luteinized) cells.
- +/-Hemorrhagic centre.
Images:
Benign mesothelial inclusion cyst
- AKA mesothelial inclusion cyst.
- AKA peritoneal inclusion cyst.[citation needed]
- AKA cortical inclusion cyst.[4][citation needed]
- AKA surface epithelial inclusion cyst.
General
- May be found incidentally, e.g. during C-section.
Epidemiology:
- Associated with previous surgery.
Gross
Microscopic
Features:
- Benign mesothelium.
- Single layer of squamoid or cuboid mesothelial cells.[6]
DDx:
- Serous cystadenoma of the ovary - must be >=1 cm.[7]
Image:
IHC
- CK +ve, calretinin +ve.[6]
Sign out
OVARY, LEFT, BIOPSY: - BENIGN CORTICAL INCLUSION CYST.
Ovarian infarct
Main article: Ovarian infarct
Pregnancy luteoma
Main article: Pregnancy luteoma
Ovarian tumours
Main article: Ovarian tumours
For a very brief overview of gynecologic tumours see: Gynecologic pathology.
See also
References
- ↑ IAV. 6 February 2009.
- ↑ Auersperg N, Wong AS, Choi KC, Kang SK, Leung PC (April 2001). "Ovarian surface epithelium: biology, endocrinology, and pathology". Endocr. Rev. 22 (2): 255–88. PMID 11294827. http://edrv.endojournals.org/cgi/pmidlookup?view=long&pmid=11294827.
- ↑ ALS. 5 February 2009.
- ↑ Feeley, KM.; Wells, M. (Feb 2001). "Precursor lesions of ovarian epithelial malignancy.". Histopathology 38 (2): 87-95. PMID 11207821.
- ↑ GAG 26 Feb 2009.
- ↑ 6.0 6.1 6.2 Urbanczyk K, Skotniczny K, Kucinski J, Friediger J (2005). "Mesothelial inclusion cysts (so-called benign cystic mesothelioma)--a clinicopathological analysis of six cases". Pol J Pathol 56 (2): 81-7. PMID 16092670.
- ↑ Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 384. ISBN 978-0443069208.
- ↑ Asch, E.; Levine, D.; Kim, Y.; Hecht, JL. (Mar 2008). "Histologic, surgical, and imaging correlations of adnexal masses.". J Ultrasound Med 27 (3): 327-42. PMID 18314510.