Difference between revisions of "Orchiectomy grossing"
Jump to navigation
Jump to search
| Line 44: | Line 44: | ||
*The tumour should be [[submitted in total]] if this can be done in less than 10 cassettes. | *The tumour should be [[submitted in total]] if this can be done in less than 10 cassettes. | ||
*Lester's book (2nd Ed.) recommends 1 cassette per cm of maximal tumour dimension.<ref>{{Ref Lester|409}}</ref> | *Lester's book (2nd Ed.) recommends 1 cassette per cm of maximal tumour dimension.<ref>{{Ref Lester|409}}</ref> | ||
====Staging==== | |||
*pT2 - into tunica vaginalis or [[lymphovascular invasion]].<ref name=cancer_org>URL: [http://www.cancer.org/cancer/testicularcancer/detailedguide/testicular-cancer-staging http://www.cancer.org/cancer/testicularcancer/detailedguide/testicular-cancer-staging]. Accessed on: 15 December 2014.</ref> | |||
*pT3 - into spermatic cord.<ref name=cancer_org/> | |||
Notes:<ref name=cancer_org/> | |||
*Invasion into the [[epididymis]] or tunica albuginea does not change the [[cancer staging|stage]]. | |||
===Alternate approaches=== | ===Alternate approaches=== | ||
Revision as of 02:30, 16 December 2014
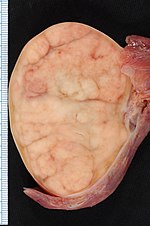
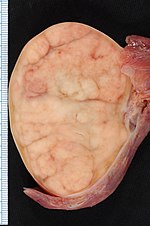
Orchiectomy specimen showing testis replaced by tumour (proven to be seminoma).
This article deals with orchiectomy grossing.
Introduction
Orchiectomies are typically done for testicular tumours.
They may be done for chronic pain or to control prostate cancer.
Protocol
Dimensions and weight:
- Laterality: [ left / right ].
- Weight: ___ grams.
- Testis: ___ x ___ x ___ cm.
- Epididymis: ___ x ___ x ___ cm.
- Spermatic cord - length: __ cm, diameter: ___ cm.
- Inking: [colour].
Tumour:
- Size: ___ x ___ x ___ cm.
- Colour: [ tan / white / variable ].
- Firmness: [ firm / soft ].
- Morphology: [solid / cystic / solid and cystic - with ___ % cystic].
- Circumscription: [circumscribed / infiltrative border ].
- Hemorrhage: [ absent / present ].
- Necrosis: [ absent / present ].
- Extension into tunica albuginea: [ not identified / indeterminate / present ].
- Extension into the epididymis: [ not identified / indeterminate / present ].
Other - after sectioning:
- Testicular parenchyma: [ brown-tan, unremarkable / ___ ].
- Spermatic cord: [ unremarkable / ___ ].
Representative sections are submitted as follow:
- Spermatic cord resection margin, en face.
- Spermatic cord mid-section, cross section.
- Spermatic cord close to testis.
- Tumour in relation to epididymis.
- Tumour and rete testis.
- Tumour with testicular coverings.
- Additional tumour sections.
- Testis distant from the tumour.
Protocol notes
- The tumour should be submitted in total if this can be done in less than 10 cassettes.
- Lester's book (2nd Ed.) recommends 1 cassette per cm of maximal tumour dimension.[1]
Staging
- pT2 - into tunica vaginalis or lymphovascular invasion.[2]
- pT3 - into spermatic cord.[2]
Notes:[2]
- Invasion into the epididymis or tunica albuginea does not change the stage.
Alternate approaches
See also
Related protocols
References
- ↑ Lester, Susan Carole (2005). Manual of Surgical Pathology (2nd ed.). Saunders. pp. 409. ISBN 978-0443066450.
- ↑ 2.0 2.1 2.2 URL: http://www.cancer.org/cancer/testicularcancer/detailedguide/testicular-cancer-staging. Accessed on: 15 December 2014.