Difference between revisions of "Oral pathology"
| (6 intermediate revisions by the same user not shown) | |||
| Line 52: | Line 52: | ||
Features: | Features: | ||
*+/-Ulceration.<ref name=pmid2234878>{{Cite journal | last1 = Hay | first1 = KD. | last2 = Greig | first2 = DE. | title = Propolis allergy: a cause of oral mucositis with ulceration. | journal = Oral Surg Oral Med Oral Pathol | volume = 70 | issue = 5 | pages = 584-6 | month = Nov | year = 1990 | doi = | PMID = 2234878 }}</ref> | *+/-Ulceration.<ref name=pmid2234878>{{Cite journal | last1 = Hay | first1 = KD. | last2 = Greig | first2 = DE. | title = Propolis allergy: a cause of oral mucositis with ulceration. | journal = Oral Surg Oral Med Oral Pathol | volume = 70 | issue = 5 | pages = 584-6 | month = Nov | year = 1990 | doi = | PMID = 2234878 }}</ref> | ||
Image: | |||
*[http://lupusimages.com/browser/detail/2488/histopathology-hyperparakeratosis-with-interface-mucositis Interface mucositis with parakeratosis in lupus (lupusimages.com)]. | |||
=Odontogenic tumours and cysts= | =Odontogenic tumours and cysts= | ||
| Line 96: | Line 99: | ||
===General=== | ===General=== | ||
*Benign. | *Benign. | ||
*Sexually transmitted.<ref name=Ref_HaNP246>{{Ref HaNP| | *Sexually transmitted.<ref name=Ref_HaNP246>{{Ref HaNP|246}}</ref> | ||
*Typically seen in young adults. | *Typically seen in young adults. | ||
===Gross=== | ===Gross=== | ||
*Polypoid projection with a broad base. | *Polypoid projection with a broad base. | ||
*Usually palate or labia.<ref name=Ref_HaNP246>{{Ref HaNP| | *Usually palate or labia.<ref name=Ref_HaNP246>{{Ref HaNP|246}}</ref> | ||
===Microscopic=== | ===Microscopic=== | ||
| Line 108: | Line 111: | ||
*No hyperkeratosis. | *No hyperkeratosis. | ||
DDx:<ref name=Ref_HaNP246>{{Ref HaNP| | DDx:<ref name=Ref_HaNP246>{{Ref HaNP|246}}</ref> | ||
*[[Squamous papilloma]] - thinner papillary projections, often branch. | *[[Squamous papilloma]] - thinner papillary projections, often branch. | ||
*[[Verruca vulgaris]] - church spire-like projections, hyperkeratosis and parakeratosis. | *[[Verruca vulgaris]] - church spire-like projections, hyperkeratosis and parakeratosis. | ||
| Line 126: | Line 129: | ||
*[[AKA]] ''focal fibrous hyperplasia'', [[AKA]] ''peripheral ossifying fibroma, [[AKA]] ''fibroid epulis'' (old term), [[AKA]] ''fibroepithelial polyp''.<ref name=Ref_Sternberg5_775>{{Ref Sternberg5|775}}</ref> | *[[AKA]] ''focal fibrous hyperplasia'', [[AKA]] ''peripheral ossifying fibroma, [[AKA]] ''fibroid epulis'' (old term), [[AKA]] ''fibroepithelial polyp''.<ref name=Ref_Sternberg5_775>{{Ref Sternberg5|775}}</ref> | ||
*[[AKA]] ''oral fibroma''.<ref>URL: [http://emedicine.medscape.com/article/1080948-overview#aw2aab6b3 http://emedicine.medscape.com/article/1080948-overview#aw2aab6b3]. Accessed on: 20 August 2012.</ref><ref name=Ref_HaNP240>{{Ref HaNP|240}}</ref> | *[[AKA]] ''oral fibroma''.<ref>URL: [http://emedicine.medscape.com/article/1080948-overview#aw2aab6b3 http://emedicine.medscape.com/article/1080948-overview#aw2aab6b3]. Accessed on: 20 August 2012.</ref><ref name=Ref_HaNP240>{{Ref HaNP|240}}</ref> | ||
{{Main|Oral fibroma}} | |||
=Pigmented lesions of the oral cavity= | =Pigmented lesions of the oral cavity= | ||
| Line 295: | Line 278: | ||
*[[Odontogenic tumours and cysts]]. | *[[Odontogenic tumours and cysts]]. | ||
*[[Tongue]]. | *[[Tongue]]. | ||
*[[Tonsil]]. | |||
=References= | =References= | ||
Latest revision as of 18:17, 2 May 2017
Oral pathology is a domain of dentistry. In the context of anatomical pathology, it can be lumped with head and neck pathology. Oral lesions and oral cavity redirect here.
Normal
Normal oral mucosa
- Buccal mucosa redirect here.
Microscopic
- Non-keratinized squamous mucosa.
- No pigmentation.
- No inflammation.
Reactive
Benign leukoplakia
General
- Very common finding.
- Biopsied as it may be malignant.
Microscopic
Features:
- Hyperkeratosis.
- Parakeratosis.
- No nuclear atypia.
- No pigmentation.
- No significant inflammation.
DDx:
- Dysplasia.
- Squamous cell carcinoma.
- Benign alveolar ridge keratosis.
Sign out
BUCCAL MUCOSA, RIGHT, BIOPSY: - SQUAMOUS MUCOSA WITH A COMPACT KERATIN LAYER AND PARAKERATOSIS. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Micro
The sections show a squamous mucosa with a layer of compact keratin, parakeratosis, and focal hypergranulosis. There is no inflammation at the interface. Epidermal intercellular bridges are easily seen. There is no significant nuclear atypia. Mitoses are not evident.
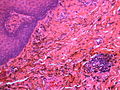
Oral contact mucositis
General
- Inflammatory reaction of irritative agent, e.g. cinnamon-flavoured chewing gum.[1]
- Similar to contact dermatitis.[2]
Note:
- Oral mucositis be seen in the context of radiation treatment.[3]
Microscopic
Features:
- +/-Ulceration.[2]
Image:
Odontogenic tumours and cysts
Oral infections
Oral candidiasis
General
- Due to candida - a fungus.
- May be associated with immunodeficiency, e.g. AIDS, organ transplant/immunosuppression.
Forms:[4]
- Pseudomembranous (thrush).
- Erythematous.
- Hyperplastic.
Microscopic
- See candidiasis.
Hairy leukoplakia
General
Features:[4]
Gross
- White confluent patches (icing sugar) - usu. tongue.
DDx:
- See leukoplakia.
Images:
Microscopic
Features:[7]
- Hyperkeratosis (thicker stratum corneum).[8]
- Acanthosis (thicker stratum spinosum).[9]
- "Balloon cells" in upper stratum spinosum - perinuclear clearing.
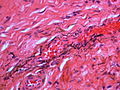
Oral condyloma
General
- Benign.
- Sexually transmitted.[10]
- Typically seen in young adults.
Gross
- Polypoid projection with a broad base.
- Usually palate or labia.[10]
Microscopic
Features:
- Broad papillary projections with rounded contours.
- No hyperkeratosis.
DDx:[10]
- Squamous papilloma - thinner papillary projections, often branch.
- Verruca vulgaris - church spire-like projections, hyperkeratosis and parakeratosis.
- Squamous cell carcinoma.
Image:
Sign out
LESION, PALATE, EXCISION: - ORAL CONDYLOMA.
Oral neoplasms
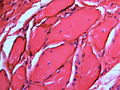
Peripheral fibroma
- AKA focal fibrous hyperplasia, AKA peripheral ossifying fibroma, AKA fibroid epulis (old term), AKA fibroepithelial polyp.[12]
- AKA oral fibroma.[13][14]
Pigmented lesions of the oral cavity
A brief DDx of pigmented lesions:[15]
- Diffuse & bilateral:
- Peutz-Jeghers syndrome.
- Addison's disease.
- Drug-induced - typically OCP or tetracycline, usu. has an irregular distribution.[16]
- Smoker's melanosis.
- Focal:
- Vascular lesions.
- Amalgam tattoo.
- Melanocytic lesions.
- Melanotic macule.
- Blue nevus.
- Malignant melanoma - classically hard palate.[16]
Melanotic macule
General
- Benign.
- Clinically apparent lesion.
Gross
Image:
Microscopic
Features - either or both of the following:[17]
- Pigmented basal cell layer.
- Pigment incontinence - (dermal) macrophages with pigment (melanin).
DDx:
- Focal melanosis - not clinically apparent, i.e. history does not say pigmented lesion.
Image:
Stains
- Fontana-Masson stain +ve.
- Prussian blue stain -ve.
Sign out
LESION, BUCCAL MUCOSA (LEFT), BIOPSY: - MELANOTIC MACUOLE. - NEGATIVE FOR DYSPLASIA. - NEGATIVE FOR MALIGNANCY.
Micro
The sections show a non-keratinized squamous mucosa. The squamous epithelium has no significant pathology and does not have noticeable pigmentation. The subepithelial tissue has pigmented macrophages (melanophages) and is otherwise unremarkable.
A Fontana-Masson stain marks the pigment (confirming it is melanin). A Prussian blue stain is negative.
Smoker's melanosis
General
- Benign.
- Seen in ~20% of smokers.[15]
- Presence of find (smoking) dose-dependent, i.e. longer heavier smokers are more likely to have it.
Gross
- Typically labial gingvia or buccal mucosa.[15]
Microscopic
Features:
- Basal melanosis.
- +/-Melanin incontinence.
Image:
Intramucosal melanocytic nevus
- Abbreviated IMN.
- AKA intramucosal melanocytic nevus.
General
- Most common oral nevus.[18]
- Second most common is the blue nevus.
- Essentially an intradermal melanocytic nevus.
Microscopic
Features:
- Symmetrical lesion.
- "Matures" with depth
- Less cellular with depth
- Less nuclear atypia with depth.
- Smaller cells with depth.
- Smaller nests with depth.
- Rare mitoses (superficial).
- No deep mitoses.
- No destruction of surrounding structures.
- No nucleoli.
Sign out
PALATE LESION, PUNCH BIOPSY: - INTRAMUCOSAL MELANOCYTIC NEVUS.
Amalgam tattoo
General
- Benign and common.
- Material from a dental filling.[19]
- May be confused with a melanocytic lesion.
Gross
- Pigmented lesion.
Image:
Microscopic
Features:[20]
- Fine powdery black material in the subepithelial tissue - key feature.
- May be clumped.
- Found between collagen fibres.
- +/-Foreign body-type giant cells - uncommon.
DDx:
Images
www:
Sign out
MOUTH, BIOPSY: - AMALGAM TATTOO. - SQUAMOUS MUCOSA WITH PARAKERATOSIS. - SUBEPITHELIAL CALCIFICATIONS. - NEGATIVE FOR MALIGNANCY.
See also
References
- ↑ Siqueira, AS.; Santos, CC.; Cristino, MR.; Silva, DC.; Pinheiro, Md.; Pinheiro, JJ. (Oct 2009). "Intraoral contact mucositis induced by cinnamon-flavored chewing gum--a case report.". Quintessence Int 40 (9): 719-21. PMID 19862397.
- ↑ 2.0 2.1 Hay, KD.; Greig, DE. (Nov 1990). "Propolis allergy: a cause of oral mucositis with ulceration.". Oral Surg Oral Med Oral Pathol 70 (5): 584-6. PMID 2234878.
- ↑ Lino, MD.; Carvalho, FB.; Oliveira, LR.; Magalhães, EB.; Pinheiro, AL.; Ramalho, LM. (2011). "Laser phototherapy as a treatment for radiotherapy-induced oral mucositis.". Braz Dent J 22 (2): 162-5. PMID 21537592.
- ↑ 4.0 4.1 Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 777. ISBN 0-7216-0187-1.
- ↑ Kanitakis, J.; Zambruno, G.; Marchand, C.; Perret-Liaudet, P.; Hermier, C.; Thivolet, J. (1990). "[Oral hairy leukoplakia in AIDS. Histologic and ultrastructural study of 8 cases].". Ann Dermatol Venereol 117 (5): 345-53. PMID 2169222.
- ↑ Itin, PH.; Lautenschlager, S. (1997). "Viral lesions of the mouth in HIV-infected patients.". Dermatology 194 (1): 1-7. PMID 9031782.
- ↑ URL: http://www.pathologyoutlines.com/oralcavity.html#hairyleukoplakia.
- ↑ URL: http://www.emedicine.com/asp/dictionary.asp?keyword=hyperkeratosis.
- ↑ URL: http://www.emedicine.com/asp/dictionary.asp?keyword=acanthosis.
- ↑ 10.0 10.1 10.2 Thompson, Lester D. R. (2006). Head and Neck Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 246. ISBN 978-0443069604.
- ↑ Reis, HL.; Ferreira, DC.; Forattini, AG.; Souza, PG.; Curvelo, JA.; Passos, MR. (2010). "Genital and oral human papillomavirus infection in a patient from the group of women who have sex with women.". Clinics (Sao Paulo) 65 (12): 1383-5. PMC 3020353. PMID 21340231. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3020353/.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Reuter, Victor E; Stoler, Mark H (2009). Sternberg's Diagnostic Surgical Pathology (5th ed.). Lippincott Williams & Wilkins. pp. 775. ISBN 978-0781779425.
- ↑ URL: http://emedicine.medscape.com/article/1080948-overview#aw2aab6b3. Accessed on: 20 August 2012.
- ↑ Thompson, Lester D. R. (2006). Head and Neck Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 240. ISBN 978-0443069604.
- ↑ 15.0 15.1 15.2 Kauzman, A.; Pavone, M.; Blanas, N.; Bradley, G. (Nov 2004). "Pigmented lesions of the oral cavity: review, differential diagnosis, and case presentations.". J Can Dent Assoc 70 (10): 682-3. PMID 15530266.
- ↑ 16.0 16.1 Beck-Mannagetta, J.; Hutarew, G. (Sep 2012). "[Pigmented lesions of the oral mucosa].". Hautarzt 63 (9): 704-9. doi:10.1007/s00105-012-2351-x. PMID 22956033.
- ↑ 17.0 17.1 Buchner, A.; Hansen, LS. (Sep 1979). "Melanotic macule of the oral mucosa. A clinicopathologic study of 105 cases.". Oral Surg Oral Med Oral Pathol 48 (3): 244-9. PMID 289929.
- ↑ URL: http://emedicine.medscape.com/article/1079272-overview. Accessed on: 10 December 2012.
- ↑ Thompson, Lester D. R. (2006). Head and Neck Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 215. ISBN 978-0443069604.
- ↑ Thompson, Lester D. R. (2006). Head and Neck Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 216. ISBN 978-0443069604.