Difference between revisions of "Oligodendroglioma"
Jump to navigation
Jump to search
| Line 15: | Line 15: | ||
| Gross = | | Gross = | ||
| Grossing = | | Grossing = | ||
| Site = [[neuropathology tumours]] - | | Site = [[neuropathology tumours]] - cerebral hemispheres, posterior fossa (rare), spinal cord (very rare) | ||
| Assdx = | | Assdx = | ||
| Syndromes = | | Syndromes = | ||
| Line 30: | Line 30: | ||
| Tx = | | Tx = | ||
}} | }} | ||
'''Oligodendroglioma''' is [[CNS tumour]] that is typically in the | '''Oligodendroglioma''' is [[CNS tumour]] that is typically in the cerebral hemispheres. | ||
==General== | ==General== | ||
| Line 37: | Line 37: | ||
Usual location: | Usual location: | ||
* | *Cerebral hemispheres- most often frontal lobe. | ||
*Intramedullary spinal cord. | *Posterior fossa (rare) | ||
*Intramedullary spinal cord (very rare). | |||
Prognosis by flavours (average survival):<ref name=Ref_PSNP98>{{Ref PSNP|98}}</ref> | Prognosis by flavours (average survival):<ref name=Ref_PSNP98>{{Ref PSNP|98}}</ref> | ||
Revision as of 16:07, 15 November 2014
| Oligodendroglioma | |
|---|---|
| Diagnosis in short | |
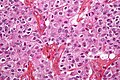
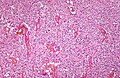
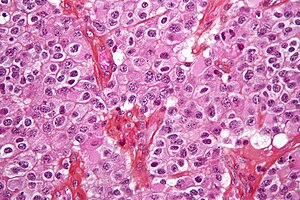 Oligodendroglioma. H&E stain. | |
|
| |
| LM | highly cellular lesion composed of cells resembling fried eggs (oligodendrocytes) with a round nucleus (important), distinct cell borders, +/-clear cytoplasm - useful feature (if present), acutely branched capillary sized vessels ("chicken-wire" like appearance), calcifications |
| LM DDx | neurocytoma, clear cell variant of ependymoma, seminoma / dysgerminoma / germinoma |
| Site | neuropathology tumours - cerebral hemispheres, posterior fossa (rare), spinal cord (very rare) |
|
| |
| Prognosis | moderate - dependent on grade |
Oligodendroglioma is CNS tumour that is typically in the cerebral hemispheres.
General
- Do not arise from oligodendrocytes.
- Arise from glial precursor cells.
Usual location:
- Cerebral hemispheres- most often frontal lobe.
- Posterior fossa (rare)
- Intramedullary spinal cord (very rare).
Prognosis by flavours (average survival):[1]
- WHO grade II: 10-15 years.
- WHO grade III: 3-5 years.
Microscopic
Features:
- Highly cellular lesion composed of:
- Cells resembling fried eggs (oligodendrocytes) with:
- Round nucleus - key feature.
- Distinct cell borders.
- Moderate-to-marked nuclear atypia.
- Clear cytoplasm - useful feature (if present).
- Some oligodendrogliomas have eosinophilic cytoplasm with focal perinuclear clearing.
- Acutely branched capillary sized vessels - "chicken-wire" like appearance.
- Abundant, delicate appearing; may vaguely resemble a paraganglioma at low power.
- Cells resembling fried eggs (oligodendrocytes) with:
- Calcifications - important feature.[2]
Note:
- Tumour cells may be plasmacytoid, i.e. have a plasma cell-like appearance.[3]
DDx:
- Neurocytoma also have perinuclear clearing and well-defined cellular borders.
- Pineocytomatous/neurocytic rosettes = (irregular) rosette with a large meshwork of fibers (neuropil) at the centre.
Notes:
- Few neural tumours have round nuclei - DDx:
- Oligodendroglioma.
- Lymphoma.
- Clear cell variant of ependymoma.
- Germ cell tumour (germinoma/dysgerminoma/seminoma).
Images
www:
- Oligodendroglioma - several images (upmc.edu).
- Oligodendroglioma with plasmacytoid cells (frontalcortex.com).
Histologic grading
Come in two flavours:
- WHO grade II.
- This is most oligodendrogliomas.
- WHO grade III.
IHC
Features:
- MAP-2 +ve.[4]
- GFAP -ve.
- Some subtypes +ve - should not be used to distinguish.[5]
- EMA +ve.
- IDH-1 -ve. (???).
- p53 -ve.
- Useful for differentiating astrocytoma vs. oligodendroglioma.
- Ki-67.
Molecular pathology
Losses of 1p and 19q both helps with diagnosis and is prognostic:[6]
- Greater chemosensitivity
- Better prognosis.
See also
References
- ↑ 1.0 1.1 Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 98. ISBN 978-0443069826.
- ↑ URL: http://www.emedicine.com/radio/topic481.htm.
- ↑ Aldape, K.; Burger, PC.; Perry, A. (Feb 2007). "Clinicopathologic aspects of 1p/19q loss and the diagnosis of oligodendroglioma.". Arch Pathol Lab Med 131 (2): 242-51. doi:10.1043/1543-2165(2007)131[242:CAOQLA]2.0.CO;2. PMID 17284109.
- ↑ Suzuki SO, Kitai R, Llena J, Lee SC, Goldman JE, Shafit-Zagardo B (May 2002). "MAP-2e, a novel MAP-2 isoform, is expressed in gliomas and delineates tumor architecture and patterns of infiltration". J. Neuropathol. Exp. Neurol. 61 (5): 403–12. PMID 12025943.
- ↑ Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 98. ISBN 978-0443069826.
- ↑ Fontaine D, Vandenbos F, Lebrun C, Paquis V, Frenay M (2008). "[Diagnostic and prognostic values of 1p and 19q deletions in adult gliomas: critical review of the literature and implications in daily clinical practice]" (in French). Rev. Neurol. (Paris) 164 (6-7): 595–604. doi:10.1016/j.neurol.2008.04.002. PMID 18565359.