Difference between revisions of "Myopericytoma"
Jump to navigation
Jump to search
(→Microscopic: more images) |
(fix sp) |
||
| (2 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | | Name = {{PAGENAME}} | ||
| Image = Myopericytoma_-_high_mag.jpg | | Image = Myopericytoma_-_high_mag.jpg | ||
| Width = | | Width = | ||
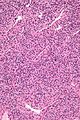
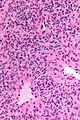
| Caption = Myopericytoma. [[H&E stain]]. | | Caption = Myopericytoma. [[H&E stain]]. | ||
| Micro = | | Micro = fascicular pattern (may be subtle) with compressed blood vessels (often thin walled & branching), increased peri-vascular cellularity; high cellularity; small bland unequally spaced epithelioid/spindle cells with moderate eosinophilic cytoplasm | ||
| Subtypes = | | Subtypes = | ||
| LMDDx = [[solitary fibrous tumour]], [[vascular tumours]] | | LMDDx = [[solitary fibrous tumour]], [[vascular tumours]] | ||
| Line 37: | Line 37: | ||
==Microscopic== | ==Microscopic== | ||
Features:<ref name=pmid21474507>{{cite journal |author=Edgecombe A, Peterson RA, Shamji FM, Commons S, Sekhon H, Gomes MM |title=Myopericytoma: a pleural-based spindle cell neoplasm off the beaten path |journal=Int. J. Surg. Pathol. |volume=19 |issue=2 |pages=247–51 |year=2011 |month=April |pmid=21474507 |doi=10.1177/1066896910381897 |url=}}</ref><ref name=Ref_WMSP615>{{Ref WMSP|615}}</ref> | Features:<ref name=pmid21474507>{{cite journal |author=Edgecombe A, Peterson RA, Shamji FM, Commons S, Sekhon H, Gomes MM |title=Myopericytoma: a pleural-based spindle cell neoplasm off the beaten path |journal=Int. J. Surg. Pathol. |volume=19 |issue=2 |pages=247–51 |year=2011 |month=April |pmid=21474507 |doi=10.1177/1066896910381897 |url=}}</ref><ref name=Ref_WMSP615>{{Ref WMSP|615}}</ref> | ||
* | *Fascicular pattern - may be subtle - with: | ||
**Compressed blood vessels, often thin walled & branching. | **Compressed blood vessels, often thin walled & branching. | ||
**Increased peri-vascular cellularity. | **Increased peri-vascular cellularity. | ||
| Line 50: | Line 50: | ||
*[[Solitary fibrous tumour]]. | *[[Solitary fibrous tumour]]. | ||
*[[Vascular tumours]]. | *[[Vascular tumours]]. | ||
*[[Angioleiomyoma]].<ref name=pmid16330949>{{cite journal |author=Mentzel T, Dei Tos AP, Sapi Z, Kutzner H |title=Myopericytoma of skin and soft tissues: clinicopathologic and immunohistochemical study of 54 cases |journal=Am. J. Surg. Pathol. |volume=30 |issue=1 |pages=104–13 |year=2006 |month=January |pmid=16330949 |doi= |url=}}</ref> | |||
===Images=== | ===Images=== | ||
Latest revision as of 05:27, 26 October 2015
| Myopericytoma | |
|---|---|
| Diagnosis in short | |
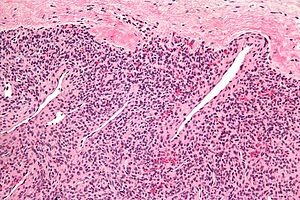 Myopericytoma. H&E stain. | |
|
| |
| LM | fascicular pattern (may be subtle) with compressed blood vessels (often thin walled & branching), increased peri-vascular cellularity; high cellularity; small bland unequally spaced epithelioid/spindle cells with moderate eosinophilic cytoplasm |
| LM DDx | solitary fibrous tumour, vascular tumours |
| IHC | SMA +ve, H-caldesmon +ve, CD34 +ve (focal), EMA -ve, AE1/AE3 -ve |
| Site | soft tissue |
|
| |
| Prevalence | uncommon |
| Prognosis | benign |
Myopericytoma, also glomangiopericytoma, is a rare perivascular soft tissue tumour.
General
- Usually benign.
- Typically in the distal extremities.[1]
- Used to be classified as hemangiopericytoma (AKA solitary fibrous tumour).
Microscopic
- Fascicular pattern - may be subtle - with:
- Compressed blood vessels, often thin walled & branching.
- Increased peri-vascular cellularity.
- Cellular lesion:
- Small bland unequally spaced epithelioid/spindle cells.
- Moderate eosinophilic cytoplasm.
Notes:
- Features overlap with myofibroma.[4]
DDx:
Images
IHC
- SMA +ve.
- H-caldesmon +ve.
- CD34 +ve (focal).
Others:[6]
- AE1/AE3 -ve.
- EMA -ve.
See also
- Glomus tumour - the other perivascular tumour.
- Soft tissue lesions.
References
- ↑ Zidane A, Arsalane A, Harkat A, et al. (November 2010). "[Myopericytoma: an uncommon chest wall tumor]" (in French). Rev Mal Respir 27 (9): 1089–91. doi:10.1016/j.rmr.2010.09.017. PMID 21111282.
- ↑ Edgecombe A, Peterson RA, Shamji FM, Commons S, Sekhon H, Gomes MM (April 2011). "Myopericytoma: a pleural-based spindle cell neoplasm off the beaten path". Int. J. Surg. Pathol. 19 (2): 247–51. doi:10.1177/1066896910381897. PMID 21474507.
- ↑ 3.0 3.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 615. ISBN 978-0781765275.
- ↑ Dray MS, McCarthy SW, Palmer AA, et al. (January 2006). "Myopericytoma: a unifying term for a spectrum of tumours that show overlapping features with myofibroma. A review of 14 cases". J. Clin. Pathol. 59 (1): 67–73. doi:10.1136/jcp.2005.028704. PMC 1860256. PMID 16394283. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1860256/.
- ↑ Mentzel T, Dei Tos AP, Sapi Z, Kutzner H (January 2006). "Myopericytoma of skin and soft tissues: clinicopathologic and immunohistochemical study of 54 cases". Am. J. Surg. Pathol. 30 (1): 104–13. PMID 16330949.
- ↑ 6.0 6.1 URL: http://e-immunohistochemistry.info/web/Myopericytoma.htm. Accessed on: 6 May 2011.