Difference between revisions of "Leydig cell tumour"
Jump to navigation
Jump to search
(more) |
(→IHC) |
||
| (11 intermediate revisions by the same user not shown) | |||
| Line 4: | Line 4: | ||
| Width = | | Width = | ||
| Caption = Leydig cell tumour. [[H&E stain]]. | | Caption = Leydig cell tumour. [[H&E stain]]. | ||
| Synonyms = interstitial cell tumour | |||
| Micro = cytoplasmic vacuolization, cytoplasm -- clear to eosinophilic, +/-''Reinke crystals'' (cylindrical crystalloid -- eosinophilic cytoplasmic bodies), +/-[[nucleoli]] common, round nuclei | | Micro = cytoplasmic vacuolization, cytoplasm -- clear to eosinophilic, +/-''Reinke crystals'' (cylindrical crystalloid -- eosinophilic cytoplasmic bodies), +/-[[nucleoli]] common, round nuclei | ||
| Subtypes = | | Subtypes = benign (common), malignant (rare) | ||
| LMDDx = [[spermatocytic | | LMDDx = [[spermatocytic tumour]] (testis only), [[pregnancy luteoma]] (females only), [[Sertoli-Leydig cell tumour]], [[Leydig cell hyperplasia]] | ||
| Stains = | | Stains = | ||
| IHC = inhibin-alpha +ve, calretinin +ve, melan A +ve | | IHC = inhibin-alpha +ve, calretinin +ve, melan A +ve | ||
| Line 24: | Line 25: | ||
| Rads = | | Rads = | ||
| Endoscopy = | | Endoscopy = | ||
| Prognosis = usu. benign | | Prognosis = usu. benign, occasionally malignant | ||
| Other = | | Other = | ||
| ClinDDx = other testicular tumours | | ClinDDx = other testicular tumours | ||
}} | }} | ||
'''Leydig cell tumour''', also known as '''interstitial cell tumour''', is an uncommon benign sex cord-stromal tumour, typically seen in the [[testis]]. | '''Leydig cell tumour''' (abbreviated '''LCT'''), also known as '''interstitial cell tumour''', is an uncommon benign sex cord-stromal tumour, typically seen in the [[testis]]. | ||
''Interstitial cell tumour'' should '''not''' be confused with ''[[renomedullary interstitial cell tumour]]''. | ''Interstitial cell tumour'' should '''not''' be confused with ''[[renomedullary interstitial cell tumour]]''. | ||
| Line 59: | Line 60: | ||
*Nucleoli common. | *Nucleoli common. | ||
*Round nuclei. | *Round nuclei. | ||
Features of malignancy in Leydig cell tumours:<ref name=pmid21691571>{{Cite journal | last1 = Vasilakaki | first1 = T. | last2 = Michalis | first2 = L. | last3 = Skafida | first3 = E. | last4 = Arkoumani | first4 = E. | last5 = Delliou | first5 = E. | last6 = Grammatoglou | first6 = X. | last7 = Kontovourkis | first7 = P. | last8 = Papamichail | first8 = V. | last9 = Stamatiou | first9 = K. | title = An unusual case of unilateral malignant leydig cell tumour of the testis. | journal = Case Rep Oncol | volume = 4 | issue = 1 | pages = 132-5 | month = Jan | year = 2011 | doi = 10.1159/000326800 | PMID = 21691571 }}</ref><ref name=pmid9808128>{{Cite journal | last1 = Cheville | first1 = JC. | last2 = Sebo | first2 = TJ. | last3 = Lager | first3 = DJ. | last4 = Bostwick | first4 = DG. | last5 = Farrow | first5 = GM. | title = Leydig cell tumor of the testis: a clinicopathologic, DNA content, and MIB-1 comparison of nonmetastasizing and metastasizing tumors. | journal = Am J Surg Pathol | volume = 22 | issue = 11 | pages = 1361-7 | month = Nov | year = 1998 | doi = | PMID = 9808128 }}</ref> | |||
*Large size (4.7 cm in metastatic LCT vs. 2.6 cm in nonmetastatic LCT<ref name=pmid9808128/>). | |||
*Infiltrative margins. | |||
*Lymphovascular invasion. | |||
*Necrosis. | |||
*Nuclear atypia. | |||
*Mitoses (>3/10 HPF). | |||
*High Ki-67 (18.6% in metastatic LCT vs. 1.2% cm in nonmetastatic LCT<ref name=pmid9808128/>). | |||
DDx: | DDx: | ||
*[[Spermatocytic | *[[Spermatocytic tumour]] (previously ''spermatocytic seminoma'') - may have eosinophilic cytoplasm. | ||
*[[Pregnancy luteoma]] - occurs during pregnancy, as the name implies. | *[[Pregnancy luteoma]] - occurs during pregnancy, as the name implies. | ||
*Leydig cell hyperplasia. | *[[Leydig cell hyperplasia]]. | ||
*[[Granular cell tumour]].<ref name=pmid17284120/> | *[[Granular cell tumour]].<ref name=pmid17284120/> | ||
| Line 74: | Line 84: | ||
www: | www: | ||
*[http://path.upmc.edu/cases/case404.html Leydig cell tumour - several images (upmc.edu)]. | *[http://path.upmc.edu/cases/case404.html Leydig cell tumour - several images (upmc.edu)]. | ||
*[http://www.webpathology.com/image.asp?case=38&n=3 Reinke crystals (webpathology.com)]. | |||
*[https://www.pinterest.com/pin/520447300659777928/ Reinke crystals (pinterest.com)]. | |||
*[https://www.pinterest.com/pin/499829258616698163/ Reinke crystals (pinterest.com)]. (???) | |||
==IHC== | ==IHC== | ||
| Line 82: | Line 95: | ||
**Expressed in [[melanoma]], [[adrenal gland|adrenal tissue]], steroid-secreting tumours. | **Expressed in [[melanoma]], [[adrenal gland|adrenal tissue]], steroid-secreting tumours. | ||
*Vimentin +ve.<ref name=pmid17284120/> | *Vimentin +ve.<ref name=pmid17284120/> | ||
*[[SALL4]] -ve (10 of 10 cases).<ref name=pmid19390421>{{cite journal |authors=Cao D, Li J, Guo CC, Allan RW, Humphrey PA |title=SALL4 is a novel diagnostic marker for testicular germ cell tumors |journal=Am J Surg Pathol |volume=33 |issue=7 |pages=1065–77 |date=July 2009 |pmid=19390421 |doi=10.1097/PAS.0b013e3181a13eef |url=}}</ref> | |||
==Sign out== | |||
<pre> | |||
Mass of Right Testicle, Radical Orchiectomy: | |||
- Leydig cell tumour. | |||
Comment: | |||
The tumour consists of polygonal cells with abundant eosinophilic | |||
cytoplasm, round nuclei with prominent nucleoli. | |||
Features suggestive of malignancy are absent. | |||
The tumour stains with calretinin, Melan A and inhibin. It is | |||
negative for AE1/AE3, and OCT4. This supports the diagnosis | |||
of Leydig cell tumour. | |||
</pre> | |||
==See also== | ==See also== | ||
Latest revision as of 20:31, 31 January 2022
Leydig cell tumour (abbreviated LCT), also known as interstitial cell tumour, is an uncommon benign sex cord-stromal tumour, typically seen in the testis.
| Leydig cell tumour | |
|---|---|
| Diagnosis in short | |
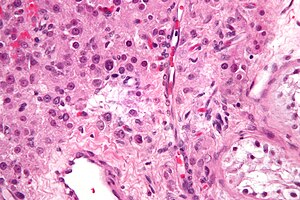 Leydig cell tumour. H&E stain. | |
|
| |
| Synonyms | interstitial cell tumour |
|
| |
| LM | cytoplasmic vacuolization, cytoplasm -- clear to eosinophilic, +/-Reinke crystals (cylindrical crystalloid -- eosinophilic cytoplasmic bodies), +/-nucleoli common, round nuclei |
| Subtypes | benign (common), malignant (rare) |
| LM DDx | spermatocytic tumour (testis only), pregnancy luteoma (females only), Sertoli-Leydig cell tumour, Leydig cell hyperplasia |
| IHC | inhibin-alpha +ve, calretinin +ve, melan A +ve |
| Gross | solid, red/tan |
| Grossing notes | orchiectomy grossing |
| Site | testis, ovary (rare) |
|
| |
| Prevalence | uncommon |
| Blood work | +/-elevated testosterone (rarely elevated estradiol) |
| Prognosis | usu. benign, occasionally malignant |
| Clin. DDx | other testicular tumours |
Interstitial cell tumour should not be confused with renomedullary interstitial cell tumour.
General
- Arises from the interstitial cell.
- May be associated with increased testosterone.
- Can be malignant in adults.[1]
- May be seen in the ovary.[2]
Clinical:[1]
- +/-Elevated testosterone.
- Rarely elevated estradiol.
- ACTH low.
Gross
- Solid, lobulated.
- Red/tan.
- Typically 3-5 cm.[1]
Image:
Microscopic
Features:[3]
- Vacuolization (cytoplasm) - key feature.
- Cytoplasm - clear to eosinophilic - important.
- Usually eosinophilic.
- Reinke crystals - classic finding, usually not present.
- Cylindrical crystalloid eosinophilic cytoplasmic bodies.
- Nucleoli common.
- Round nuclei.
Features of malignancy in Leydig cell tumours:[4][5]
- Large size (4.7 cm in metastatic LCT vs. 2.6 cm in nonmetastatic LCT[5]).
- Infiltrative margins.
- Lymphovascular invasion.
- Necrosis.
- Nuclear atypia.
- Mitoses (>3/10 HPF).
- High Ki-67 (18.6% in metastatic LCT vs. 1.2% cm in nonmetastatic LCT[5]).
DDx:
- Spermatocytic tumour (previously spermatocytic seminoma) - may have eosinophilic cytoplasm.
- Pregnancy luteoma - occurs during pregnancy, as the name implies.
- Leydig cell hyperplasia.
- Granular cell tumour.[1]
Images
www:
IHC
Sign out
Mass of Right Testicle, Radical Orchiectomy: - Leydig cell tumour. Comment: The tumour consists of polygonal cells with abundant eosinophilic cytoplasm, round nuclei with prominent nucleoli. Features suggestive of malignancy are absent. The tumour stains with calretinin, Melan A and inhibin. It is negative for AE1/AE3, and OCT4. This supports the diagnosis of Leydig cell tumour.
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Al-Agha, OM.; Axiotis, CA. (Feb 2007). "An in-depth look at Leydig cell tumor of the testis.". Arch Pathol Lab Med 131 (2): 311-7. doi:10.1043/1543-2165(2007)131[311:AILALC]2.0.CO;2. PMID 17284120.
- ↑ Yetkin, DO.; Demirsoy, ET.; Kadioglu, P. (Apr 2011). "Pure leydig cell tumour of the ovary in a post-menopausal patient with severe hyperandrogenism and erythrocytosis.". Gynecol Endocrinol 27 (4): 237-40. doi:10.3109/09513590.2010.490611. PMID 20518640.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 581. ISBN 978-0443066771.
- ↑ Vasilakaki, T.; Michalis, L.; Skafida, E.; Arkoumani, E.; Delliou, E.; Grammatoglou, X.; Kontovourkis, P.; Papamichail, V. et al. (Jan 2011). "An unusual case of unilateral malignant leydig cell tumour of the testis.". Case Rep Oncol 4 (1): 132-5. doi:10.1159/000326800. PMID 21691571.
- ↑ 5.0 5.1 5.2 Cheville, JC.; Sebo, TJ.; Lager, DJ.; Bostwick, DG.; Farrow, GM. (Nov 1998). "Leydig cell tumor of the testis: a clinicopathologic, DNA content, and MIB-1 comparison of nonmetastasizing and metastasizing tumors.". Am J Surg Pathol 22 (11): 1361-7. PMID 9808128.
- ↑ URL: http://www.antibodybeyond.com/reviews/cell-markers/leydig-cell-marker.htm. Accessed on: 18 May 2010.
- ↑ Bar-Shira Maymon B, Yavetz H, Yogev L, et al. (2005). "Detection of calretinin expression in abnormal immature Sertoli cells in non-obstructive azoospermia". Acta Histochem. 107 (2): 105–12. doi:10.1016/j.acthis.2005.02.002. PMID 15950053.
- ↑ Yao DX, Soslow RA, Hedvat CV, Leitao M, Baergen RN (September 2003). "Melan-A (A103) and inhibin expression in ovarian neoplasms". Appl. Immunohistochem. Mol. Morphol. 11 (3): 244–9. PMID 12966351.
- ↑ Cao D, Li J, Guo CC, Allan RW, Humphrey PA (July 2009). "SALL4 is a novel diagnostic marker for testicular germ cell tumors". Am J Surg Pathol 33 (7): 1065–77. doi:10.1097/PAS.0b013e3181a13eef. PMID 19390421.