Difference between revisions of "Langerhans cell histiocytosis"
Jump to navigation
Jump to search
m (→See also: wikify) |
(→Images) |
||
| (28 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
'''Langerhans cell histiocytosis''', abbreviated '''LCH''', is a rare | [[Image:Langerhans cell histiocytosis - very high mag.jpg|thumb|right|Langerhans cell histiocytosis. [[H&E stain]]. (WC/Nephron)]] | ||
'''Langerhans cell histiocytosis''', abbreviated '''LCH''', is a rare disorder of tissue macrophages. It broadly fits into the category of ''[[histiocytoses]]''. It used to known as ''eosinophilic granuloma''. | |||
It has been referred to by several eponyms - '''Hand-Schüller-Christian disease''', '''Abt-Letterer-Siwe disease''' or '''Letterer-Siwe disease''', and '''histiocytosis X'''. | |||
===Microscopic | This article deals with LCH in general. A separate article exists for ''[[pulmonary Langerhans cell histiocytosis]]''. | ||
Features: | |||
==General== | |||
===Overview=== | |||
LCH is really four (or three) diseases (depending on how one classifies it) - that happen to share the same histology:<ref name=Ref_PCPBoD8_338-9>{{Ref PCPBoD8|338-9}}</ref><ref name=pmid16295427>{{Cite journal | last1 = Chhabra | first1 = UD. | last2 = Desai | first2 = SS. | last3 = Jambhekar | first3 = NA. | title = Langerhans' cell histiocytosis: a clinicopathological study of 50 cases. | journal = Indian J Pathol Microbiol | volume = 47 | issue = 3 | pages = 370-6 | month = Jul | year = 2004 | doi = | PMID = 16295427 }}</ref> | |||
{| class="wikitable sortable" | |||
! Disease | |||
! Other name(s) | |||
! Prognosis | |||
! Demographic | |||
! Location | |||
! Risks/cause | |||
|- | |||
| [[Pulmonary Langerhans cell histiocytosis]] | |||
| Eosinophilic granuloma | |||
| good with smoking cessation | |||
| adults - smokers | |||
| lung only; typically upper lung field | |||
| due to smoking | |||
|- | |||
| Multifocal multisystem Langerhans cell histiocytosis | |||
| multisystem LCH, Letterer-Siwe disease | |||
| outcome dependent on organ involved,<ref name=pmid21351807>{{Cite journal | last1 = Minkov | first1 = M. | title = Multisystem Langerhans cell histiocytosis in children: current treatment and future directions. | journal = Paediatr Drugs | volume = 13 | issue = 2 | pages = 75-86 | month = Apr | year = 2011 | doi = 10.2165/11538540-000000000-00000 | PMID = 21351807 }}</ref> natural history 2 year survival, 50% five year survival with treatment | |||
| usu. children < 2 years old, rarely adults<ref name=pmid22470214>{{Cite journal | last1 = Garg | first1 = A. | last2 = Kumar | first2 = P. | title = Multisystem Langerhans cell histiocytosis in adult. | journal = Indian J Dermatol | volume = 57 | issue = 1 | pages = 58-60 | month = Jan | year = 2012 | doi = 10.4103/0019-5154.92683 | PMID = 22470214 }}</ref> | |||
| multiple systems (skin, spleen, liver, lung, bone marrow) | |||
| possibly genetic ‡ | |||
|- | |||
| Unifocal Langerhans cell histiocytosis † | |||
| Eosinophilic granuloma | |||
| may spontaneously regress, may cure with surgery | |||
| children (?) | |||
| bone only | |||
| possibly genetic ‡ | |||
|- | |||
| Multifocal unisystem Langerhans cell histiocytosis † | |||
| multifocal LCH, eosinophilic granuloma, Hand-Schuller-Christian syndrome = bone defect, diabetes insipidus & exopthalmos | |||
| may spontaneously regress, may cure with surgery (?) | |||
| children (?) | |||
| usu. bone; may be in: skin, lungs, stomach | |||
| possibly genetic ‡ | |||
|} | |||
Note: | |||
* † Robbins lumps these groups together. | |||
* ‡ Incompletely understood. Somatic BRAF mutations identified in approximately half of the individuals.<ref name=pmid20519626>{{Cite journal | last1 = Badalian-Very | first1 = G. | last2 = Vergilio | first2 = JA. | last3 = Degar | first3 = BA. | last4 = MacConaill | first4 = LE. | last5 = Brandner | first5 = B. | last6 = Calicchio | first6 = ML. | last7 = Kuo | first7 = FC. | last8 = Ligon | first8 = AH. | last9 = Stevenson | first9 = KE. | title = Recurrent BRAF mutations in Langerhans cell histiocytosis. | journal = Blood | volume = 116 | issue = 11 | pages = 1919-23 | month = Sep | year = 2010 | doi = 10.1182/blood-2010-04-279083 | PMID = 20519626 }}</ref><ref name=pmid22017623>{{Cite journal | last1 = Badalian-Very | first1 = G. | last2 = Vergilio | first2 = JA. | last3 = Degar | first3 = BA. | last4 = Rodriguez-Galindo | first4 = C. | last5 = Rollins | first5 = BJ. | title = Recent advances in the understanding of Langerhans cell histiocytosis. | journal = Br J Haematol | volume = 156 | issue = 2 | pages = 163-72 | month = Jan | year = 2012 | doi = 10.1111/j.1365-2141.2011.08915.x | PMID = 22017623 }}</ref> | |||
===Clinical presentation=== | |||
Features - dependent on subtype:<ref name=Ref_PCPBoD8_338-9>{{Ref PCPBoD8|338-9}}</ref> | |||
*May present with fever, anemia, bone pain, bone fracture, diabetes insipidus, exophthalmos. | |||
*Can be an incidental finding. | |||
==Microscopic== | |||
Features:<ref name=pmid16295427/> | |||
*Langerhans cells histiocytes - '''key feature'''. | *Langerhans cells histiocytes - '''key feature'''. | ||
**Clusters of cells (histiocytes) with a reniform (kidney-shaped) nucleus and abundant foamy cytoplasm. | **Clusters of cells (histiocytes) with a reniform (kidney-shaped) nucleus and abundant foamy cytoplasm. | ||
***Nucleus may look like a "coffee bean", i.e. have nuclear grooves (similar to those in [[papillary thyroid carcinoma]]) -- appearance dependent on the rotation of the nucleus.<ref>BN. 15 March 2011.</ref> | ***Nucleus may look like a "[[coffee bean nucleus|coffee bean]]", i.e. have nuclear grooves (similar to those in [[papillary thyroid carcinoma]]) -- appearance dependent on the rotation of the nucleus.<ref>BN. 15 March 2011.</ref> May be called "buttock cells". | ||
***Chromatin pattern: fine granular, light gray. | ***Chromatin pattern: fine granular, light gray. | ||
*+/-Eosinophils - often prominent. | *+/-Eosinophils - often prominent. | ||
*+/-Fibrosis - common. | |||
*+/-Other inflammatory cells - neutrophils, plasma cells (uncommon). | |||
*+/-Multinucleated giant cells - uncommon. | |||
DDx: | |||
*[ | *[[Kimura disease]] - eosinophilia. | ||
*[ | *See ''[[lymph node pathology]]''. | ||
*See ''[[Long_power_list#Many_eosinophils|lesions with many eosinophils]]''. | |||
===Images=== | |||
<gallery> | |||
* | Image:Langerhans cell histiocytosis - very low mag.jpg| LCH - very low mag. (WC/Nephron) | ||
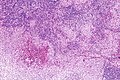
Image:Langerhans cell histiocytosis - low mag.jpg| LCH - low mag. (WC/Nephron) | |||
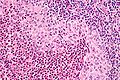
Image:Langerhans cell histiocytosis - intermed mag.jpg| LCH - intermed. mag. (WC/Nephron) | |||
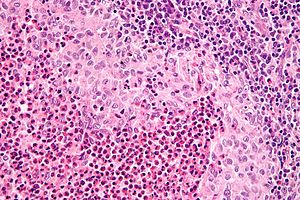
Image:Langerhans cell histiocytosis - very high mag.jpg| LCH - very high mag. (WC/Nephron) | |||
</gallery> | |||
====www==== | |||
*[http://path.upmc.edu/cases/case533.html LCH - several images (upmc.edu)]. | |||
==IHC== | |||
*CD1a +ve. | *CD1a +ve. | ||
*S100 +ve. | *S100 +ve. | ||
*CD207 ([[AKA]] Langerin) +ve.<ref name=omim604862>{{OMIM|604862}}</ref> | |||
==Molecular== | |||
*Commonly have BRAF mutations ~ 40-70% of cases.<ref name=pmid26980021>{{Cite journal | last1 = Alayed | first1 = K. | last2 = Medeiros | first2 = LJ. | last3 = Patel | first3 = KP. | last4 = Zuo | first4 = Z. | last5 = Li | first5 = S. | last6 = Verma | first6 = S. | last7 = Galbincea | first7 = J. | last8 = Cason | first8 = RC. | last9 = Luthra | first9 = R. | title = BRAF and MAP2K1 mutations in Langerhans cell histiocytosis: a study of 50 cases. | journal = Hum Pathol | volume = | issue = | pages = | month = Feb | year = 2016 | doi = 10.1016/j.humpath.2015.12.029 | PMID = 26980021 }}</ref> | |||
**The ''[[BRAF V600E mutation|V600E mutation]]'' is the most common BRAF mutation.<ref name=pmid27094161>{{Cite journal | last1 = Tatsuno | first1 = M. | last2 = Shioda | first2 = Y. | last3 = Iwafuchi | first3 = H. | last4 = Yamazaki | first4 = S. | last5 = Iijima | first5 = K. | last6 = Takahashi | first6 = C. | last7 = Ono | first7 = H. | last8 = Uchida | first8 = K. | last9 = Okamura | first9 = O. | title = BRAF V600 mutations in Langerhans cell histiocytosis with a simple and unique assay. | journal = Diagn Pathol | volume = 11 | issue = 1 | pages = 39 | month = | year = 2016 | doi = 10.1186/s13000-016-0489-z | PMID = 27094161 }}</ref> | |||
**MAP2K1 mutations are often found in the cases without BRAF mutations.<ref name=pmid26980021/><ref>{{Cite journal | last1 = Chakraborty | first1 = R. | last2 = Hampton | first2 = OA. | last3 = Shen | first3 = X. | last4 = Simko | first4 = SJ. | last5 = Shih | first5 = A. | last6 = Abhyankar | first6 = H. | last7 = Lim | first7 = KP. | last8 = Covington | first8 = KR. | last9 = Trevino | first9 = L. | title = Mutually exclusive recurrent somatic mutations in MAP2K1 and BRAF support a central role for ERK activation in LCH pathogenesis. | journal = Blood | volume = 124 | issue = 19 | pages = 3007-15 | month = Nov | year = 2014 | doi = 10.1182/blood-2014-05-577825 | PMID = 25202140 }}</ref> | |||
==Electron microscopy== | |||
*[[Birbeck granules]]. | |||
Etiology: | |||
*Cell membrane invagination.<ref>URL: [http://path.upmc.edu/cases/case147/micro.html http://path.upmc.edu/cases/case147/micro.html]. Accessed on: 7 January 2012.</ref> | |||
Appearance: | |||
*Electron dense, cytoplasmic tennis racket-like body. | |||
Images: | |||
*[http://path.upmc.edu/cases/case147/micro.html LCH (upmc.edu)]. | |||
*[http://path.upmc.edu/cases/case298/images/fig09.jpg Birbeck granule - perfect 'tennis racket' (upmc.edu)].<ref>URL: [http://path.upmc.edu/cases/case298.html http://path.upmc.edu/cases/case298.html]. Accessed on: 14 January 2012.</ref> | |||
==See also== | ==See also== | ||
| Line 32: | Line 112: | ||
[[Category:Haematopathology]] | [[Category:Haematopathology]] | ||
[[Category:Diagnosis]] | |||
Latest revision as of 03:32, 25 April 2016
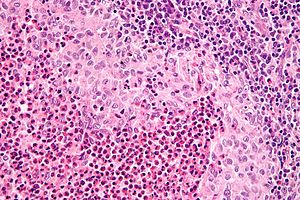
Langerhans cell histiocytosis. H&E stain. (WC/Nephron)
Langerhans cell histiocytosis, abbreviated LCH, is a rare disorder of tissue macrophages. It broadly fits into the category of histiocytoses. It used to known as eosinophilic granuloma.
It has been referred to by several eponyms - Hand-Schüller-Christian disease, Abt-Letterer-Siwe disease or Letterer-Siwe disease, and histiocytosis X.
This article deals with LCH in general. A separate article exists for pulmonary Langerhans cell histiocytosis.
General
Overview
LCH is really four (or three) diseases (depending on how one classifies it) - that happen to share the same histology:[1][2]
| Disease | Other name(s) | Prognosis | Demographic | Location | Risks/cause |
|---|---|---|---|---|---|
| Pulmonary Langerhans cell histiocytosis | Eosinophilic granuloma | good with smoking cessation | adults - smokers | lung only; typically upper lung field | due to smoking |
| Multifocal multisystem Langerhans cell histiocytosis | multisystem LCH, Letterer-Siwe disease | outcome dependent on organ involved,[3] natural history 2 year survival, 50% five year survival with treatment | usu. children < 2 years old, rarely adults[4] | multiple systems (skin, spleen, liver, lung, bone marrow) | possibly genetic ‡ |
| Unifocal Langerhans cell histiocytosis † | Eosinophilic granuloma | may spontaneously regress, may cure with surgery | children (?) | bone only | possibly genetic ‡ |
| Multifocal unisystem Langerhans cell histiocytosis † | multifocal LCH, eosinophilic granuloma, Hand-Schuller-Christian syndrome = bone defect, diabetes insipidus & exopthalmos | may spontaneously regress, may cure with surgery (?) | children (?) | usu. bone; may be in: skin, lungs, stomach | possibly genetic ‡ |
Note:
- † Robbins lumps these groups together.
- ‡ Incompletely understood. Somatic BRAF mutations identified in approximately half of the individuals.[5][6]
Clinical presentation
Features - dependent on subtype:[1]
- May present with fever, anemia, bone pain, bone fracture, diabetes insipidus, exophthalmos.
- Can be an incidental finding.
Microscopic
Features:[2]
- Langerhans cells histiocytes - key feature.
- Clusters of cells (histiocytes) with a reniform (kidney-shaped) nucleus and abundant foamy cytoplasm.
- Nucleus may look like a "coffee bean", i.e. have nuclear grooves (similar to those in papillary thyroid carcinoma) -- appearance dependent on the rotation of the nucleus.[7] May be called "buttock cells".
- Chromatin pattern: fine granular, light gray.
- Clusters of cells (histiocytes) with a reniform (kidney-shaped) nucleus and abundant foamy cytoplasm.
- +/-Eosinophils - often prominent.
- +/-Fibrosis - common.
- +/-Other inflammatory cells - neutrophils, plasma cells (uncommon).
- +/-Multinucleated giant cells - uncommon.
DDx:
- Kimura disease - eosinophilia.
- See lymph node pathology.
- See lesions with many eosinophils.
Images
www
IHC
Molecular
- Commonly have BRAF mutations ~ 40-70% of cases.[9]
- The V600E mutation is the most common BRAF mutation.[10]
- MAP2K1 mutations are often found in the cases without BRAF mutations.[9][11]
Electron microscopy
Etiology:
- Cell membrane invagination.[12]
Appearance:
- Electron dense, cytoplasmic tennis racket-like body.
Images:
See also
References
- ↑ 1.0 1.1 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 338-9. ISBN 978-1416054542.
- ↑ 2.0 2.1 Chhabra, UD.; Desai, SS.; Jambhekar, NA. (Jul 2004). "Langerhans' cell histiocytosis: a clinicopathological study of 50 cases.". Indian J Pathol Microbiol 47 (3): 370-6. PMID 16295427.
- ↑ Minkov, M. (Apr 2011). "Multisystem Langerhans cell histiocytosis in children: current treatment and future directions.". Paediatr Drugs 13 (2): 75-86. doi:10.2165/11538540-000000000-00000. PMID 21351807.
- ↑ Garg, A.; Kumar, P. (Jan 2012). "Multisystem Langerhans cell histiocytosis in adult.". Indian J Dermatol 57 (1): 58-60. doi:10.4103/0019-5154.92683. PMID 22470214.
- ↑ Badalian-Very, G.; Vergilio, JA.; Degar, BA.; MacConaill, LE.; Brandner, B.; Calicchio, ML.; Kuo, FC.; Ligon, AH. et al. (Sep 2010). "Recurrent BRAF mutations in Langerhans cell histiocytosis.". Blood 116 (11): 1919-23. doi:10.1182/blood-2010-04-279083. PMID 20519626.
- ↑ Badalian-Very, G.; Vergilio, JA.; Degar, BA.; Rodriguez-Galindo, C.; Rollins, BJ. (Jan 2012). "Recent advances in the understanding of Langerhans cell histiocytosis.". Br J Haematol 156 (2): 163-72. doi:10.1111/j.1365-2141.2011.08915.x. PMID 22017623.
- ↑ BN. 15 March 2011.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 604862
- ↑ 9.0 9.1 Alayed, K.; Medeiros, LJ.; Patel, KP.; Zuo, Z.; Li, S.; Verma, S.; Galbincea, J.; Cason, RC. et al. (Feb 2016). "BRAF and MAP2K1 mutations in Langerhans cell histiocytosis: a study of 50 cases.". Hum Pathol. doi:10.1016/j.humpath.2015.12.029. PMID 26980021.
- ↑ Tatsuno, M.; Shioda, Y.; Iwafuchi, H.; Yamazaki, S.; Iijima, K.; Takahashi, C.; Ono, H.; Uchida, K. et al. (2016). "BRAF V600 mutations in Langerhans cell histiocytosis with a simple and unique assay.". Diagn Pathol 11 (1): 39. doi:10.1186/s13000-016-0489-z. PMID 27094161.
- ↑ Chakraborty, R.; Hampton, OA.; Shen, X.; Simko, SJ.; Shih, A.; Abhyankar, H.; Lim, KP.; Covington, KR. et al. (Nov 2014). "Mutually exclusive recurrent somatic mutations in MAP2K1 and BRAF support a central role for ERK activation in LCH pathogenesis.". Blood 124 (19): 3007-15. doi:10.1182/blood-2014-05-577825. PMID 25202140.
- ↑ URL: http://path.upmc.edu/cases/case147/micro.html. Accessed on: 7 January 2012.
- ↑ URL: http://path.upmc.edu/cases/case298.html. Accessed on: 14 January 2012.