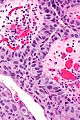
High-grade papillary urothelial carcinoma
| High-grade papillary urothelial carcinoma | |
|---|---|
| Diagnosis in short | |
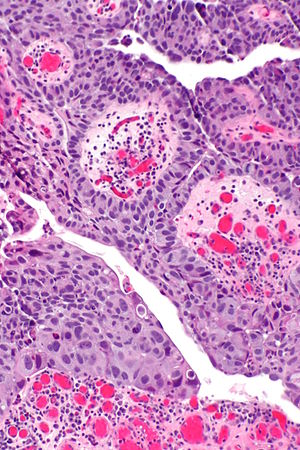 High-grade papillary urothelial carcinoma. H&E stain. | |
|
| |
| LM | papillae with "architectural complexity" (fused papillae, branching of papillae), +/-nuclear pleomorphism, nuclear enlargement - often 4-5x the size of stromal lymphocytes, mitoses (common), +/-invasion into the lamina propria (common) |
| Subtypes | subtype of urothelial carcinoma |
| LM DDx | low-grade papillary urothelial carcinoma, urothelial carcinoma in situ, squamous cell carcinoma |
| IHC | Ki-67 high (>35% of cells), PAX8 -ve |
| Gross | exophytic mass, frond-like appearance, friable |
| Site | urothelium - usu. urinary bladder |
|
| |
| Syndromes | Lynch syndrome |
|
| |
| Signs | hematuria |
| Prevalence | common |
| Prognosis | dependent on stage, usu. moderate |
| Clin. DDx | low-grade papillary urothelial carcinoma |
High-grade papillary urothelial carcinoma, abbreviated HGPUC, is a common form of cancer that arises from the urothelium.
It is also known as high-grade papillary urothelial cell carcinoma, abbreviated HGPUCC.
General
- Aggressive.
- May be associated with Lynch syndrome.[1]
Gross
- Exophytic mass.
- Frond-like appearance.
- Friable.
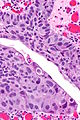
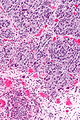
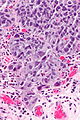
Microscopic
Features:[2]
- "High grade nuclear features":
- Nuclear pleomorphism - often 4-5x the size of stromal lymphocytes.[3]
- Papillae with "architectural complexity":
- Fused papillae - common.
- Branching of papillae common.
- Mitoses - common.
- +/-Invasion into the lamina propria - relatively common.
Note:
- The presence/absence of muscle should be commented on in biopsy specimens.
- Adipose tissue may be seen in the lamina propria; tumour adjacent to adipose tissue on a biopsy does not imply invasion deep to the muscularis propria.[4]
DDx:
- Low grade papillary urothelial carcinoma.
- Prostate carcinoma with pseudopapillae[7] - see urothelial carcinoma-like prostatic carcinoma.
- Should be considered if a urethral tumour.
Images
IHC
- Ki-67:
- p53 +ve - more common in pT2 than pT1 and HGPUC than LGPUC... but not useful to definitively separate.[11]
Molecular
Molecular changes:[12]
- p53.
- p21.
- RB.
- E-cadherin - decreased bad.
- RhoGD12 - increased bad.
- VEGF - increased bad.
Sign out
Urinary Bladder Tumour, Transurethral Resection: - HIGH-GRADE PAPILLARY UROTHELIAL CARCINOMA. -- NEGATIVE for lamina propria invasion. -- NEGATIVE for lymphovascular invasion. -- Please see synoptic report. - Muscularis propria present and NEGATIVE for invasion. - NEGATIVE for (flat) urothelial carcinoma in situ.
Block letters
URINARY BLADDER LESION ("TUMOUR"), TRANSURETHRAL RESECTION:
- HIGH-GRADE PAPILLARY UROTHELIAL CARCINOMA.
- NO LAMINA PROPRIA INVASION APPARENT.
- NEGATIVE FOR LYMPHOVASCULAR INVASION.
- NO MUSCULARIS PROPRIA IDENTIFIED.
Invasion into the lamina propria
Urinary Bladder Tumour, Transurethral Resection: - INVASIVE HIGH-GRADE PAPILLARY UROTHELIAL CARCINOMA with lamina propria invasion. -- Muscularis propria present, NEGATIVE for muscularis propria invasion. -- NEGATIVE for lymphovascular invasion. -- Please see synoptic report.
Block letters
URINARY BLADDER LESION ("TUMOUR"), TRANSURETHRAL RESECTION URINARY BLADDER TUMOUR (TURBT):
- INVASIVE HIGH-GRADE PAPILLARY UROTHELIAL CARCINOMA WITH LAMINA PROPRIA INVASION.
- MUSCULARIS PROPRIA NEGATIVE FOR INVASIVE MALIGNANCY.
- NEGATIVE FOR LYMPHOVASCULAR INVASION.
Invasion into the muscularis propria
URINARY BLADDER LESION ("TUMOUR"), TRANSURETHRAL RESECTION URINARY BLADDER TUMOUR (TURBT):
- INVASIVE HIGH-GRADE PAPILLARY UROTHELIAL CARCINOMA AT LEAST INTO MUSCULARIS PROPRIA.
- LYMPHOVASCULAR INVASION PRESENT.
Low-grade versus high-grade
URINARY BLADDER LESION ("TUMOUR"), TRANSURETHRAL RESECTION URINARY BLADDER TUMOUR (TURBT):
- HIGH-GRADE PAPILLARY UROTHELIAL CARCINOMA, SEE COMMENT.
- NEGATIVE FOR LAMINA PROPRIA INVASION.
- NO MUSCULARIS PROPRIA PRESENT.
COMMENT:
The sections show papillary branching, papillary fusion and scattered large cells (~4-5 a
resting lymphocyte). Atypical for a high-grade lesion is that mitotic activity is scarce
and prominent nucleoli are not present.
Micro
The sections show urothelial mucosa with thick papillary structures. Focally, nuclei are large (~3-4x resting lymphocyte), hyperchromatic and have nucleoli. Mitotic activity is present and focally brisk (4 mitoses in 1 HPF, 1 HPF~0.2376 mm*mm). Umbrella cells are seen only focally.
Alternate
The sections show a small fragment of urothelial mucosa with two papillary structures, enlarged nuclei (~3-4x resting lymphocyte) and moderate nuclear size variation. Mitotic activity is seen focally. Umbrella cells are seen only focally.
A mild lymphocyte-predominant inflammatory infiltrate is present. The lamina propria contains a nest with smaller cells, cystic spaces and no appreciable mitoses (cystitis cystica).
See also
References
- ↑ Hartmann, A.; Dietmaier, W.; Hofstädter, F.; Burgart, LJ.; Cheville, JC.; Blaszyk, H. (Mar 2003). "Urothelial carcinoma of the upper urinary tract: inverted growth pattern is predictive of microsatellite instability.". Hum Pathol 34 (3): 222-7. doi:10.1053/hupa.2003.22. PMID 12673555.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 310. ISBN 978-0781765275.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 161. ISBN 978-0443066771.
- ↑ Bochner, BH.; Nichols, PW.; Skinner, DG. (Mar 1995). "Overstaging of transitional cell carcinoma: clinical significance of lamina propria fat within the urinary bladder.". Urology 45 (3): 528-31. doi:10.1016/S0090-4295(99)80030-2. PMID 7879346.
- ↑ URL: http://surgpathcriteria.stanford.edu/bladder/tcc-papillary-transitional-urothelial-carcinoma/. Accessed on: 27 January 2014.
- ↑ Reis, LO.; Taheri, D.; Chaux, A.; Guner, G.; Mendoza Rodriguez, MA.; Bivalacqua, TJ.; Schoenberg, MP.; Epstein, JI. et al. (Jan 2016). "Significance of a minor high-grade component in a low-grade noninvasive papillary urothelial carcinoma of bladder.". Hum Pathol 47 (1): 20-5. doi:10.1016/j.humpath.2015.09.007. PMID 26520419.>
- ↑ Gordetsky J, Epstein JI (July 2014). "Pseudopapillary features in prostatic adenocarcinoma mimicking urothelial carcinoma: a diagnostic pitfall". Am. J. Surg. Pathol. 38 (7): 941–5. doi:10.1097/PAS.0000000000000178. PMID 24503758.
- ↑ Rajcani, J.; Kajo, K.; Adamkov, M.; Moravekova, E.; Lauko, L.; Felcanova, D.; Bencat, M. (2013). "Immunohistochemical characterization of urothelial carcinoma.". Bratisl Lek Listy 114 (8): 431-8. PMID 23944616.
- ↑ Pich, A.; Chiusa, L.; Comino, A.; Navone, R. (1994). "Cell proliferation indices, morphometry and DNA flow cytometry provide objective criteria for distinguishing low and high grade bladder carcinomas.". Virchows Arch 424 (2): 143-8. PMID 7910097.
- ↑ Mai, KT.; Flood, TA.; Williams, P.; Kos, Z.; Belanger, EC. (Oct 2013). "Mixed low- and high-grade papillary urothelial carcinoma: histopathogenetic and clinical significance.". Virchows Arch 463 (4): 575-81. doi:10.1007/s00428-013-1456-7. PMID 23913166.
- ↑ Koyuncuer, A.. "Immunohistochemical expression of p63, p53 in urinary bladder carcinoma.". Indian J Pathol Microbiol 56 (1): 10-5. doi:10.4103/0377-4929.116141. PMID 23924551.
- ↑ Ehdaie, B.; Theodorescu, D. (Jan 2008). "Molecular markers in transitional cell carcinoma of the bladder: New insights into mechanisms and prognosis.". Indian J Urol 24 (1): 61-7. doi:10.4103/0970-1591.38606. PMC 2684226. PMID 19468362. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2684226/.