Difference between revisions of "Glomus tumour"
(+SO) |
|||
| (21 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Glomus_tumour_-_2_-_very_high_mag.jpg | |||
| Width = | |||
| Caption = Glomus tumour. [[H&E stain]]. | |||
| Micro = sheets of equally-spaced cells ("cookie cutter appearance"), polygonal cells +/-identifiable cellular borders, thin-walled blood vessels, moderate clear cytoplasm | |||
| Subtypes = | |||
| LMDDx = | |||
| Stains = | |||
| IHC = SMA +ve (100%), desmin usu. -ve, CD34 -ve, S-100 -ve | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[skin]]/soft tissue - classically subungal (under the nail) | |||
| Assdx = | |||
| Syndromes = +/-[[neurofibromatosis 1]] | |||
| Clinicalhx = | |||
| Signs = | |||
| Symptoms = [[painful skin lesion]], cold intolerance, point tenderness | |||
| Prevalence = uncommon | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = usu. good (benign), rarely malignant | |||
| Other = | |||
| ClinDDx = | |||
| Tx = excision | |||
}} | |||
'''Glomus tumours''', also known as '''glomangioma''', are painful, perivascular tumour that are classically periungual. | '''Glomus tumours''', also known as '''glomangioma''', are painful, perivascular tumour that are classically periungual. | ||
It should not be confused with ''[[paraganglioma]]'', which were once called glomus tumour. | It should '''not''' be confused with ''[[paraganglioma]]'', which were once called glomus tumour. | ||
This tumour is classified as a ''perivascular tumour'' (also ''pericytic tumour'') which is a subset of [[soft tissue tumours]]. | This tumour is classified as a ''perivascular tumour'' (also ''pericytic tumour'') which is a subset of [[soft tissue tumours]]. | ||
| Line 8: | Line 38: | ||
*Tumour derived from smooth muscle cell.<ref name=pmid18788860>{{cite journal |author=Gombos Z, Zhang PJ |title=Glomus tumor |journal=Arch. Pathol. Lab. Med. |volume=132 |issue=9 |pages=1448–52 |year=2008 |month=September |pmid=18788860 |doi=10.1043/1543-2165(2008)132[1448:GT]2.0.CO;2 |url=}}</ref> | *Tumour derived from smooth muscle cell.<ref name=pmid18788860>{{cite journal |author=Gombos Z, Zhang PJ |title=Glomus tumor |journal=Arch. Pathol. Lab. Med. |volume=132 |issue=9 |pages=1448–52 |year=2008 |month=September |pmid=18788860 |doi=10.1043/1543-2165(2008)132[1448:GT]2.0.CO;2 |url=}}</ref> | ||
*Usually benign. | *Usually benign. | ||
**Malignant variant exists - extremely rare. | **Malignant variant exists (known as ''glomangiosarcoma'') - extremely rare.<ref>{{cite journal |authors=Alhroub OA, Mahameed SA, Abdelhafez MO, Alhroub A, Hour H, Hasasna N, Kamal N |title=A case of malignant glomus tumor (glomangiosarcoma) of the nasal cavity |journal=J Surg Case Rep |volume=2022 |issue=1 |pages=rjab641 |date=January 2022 |pmid=35096369 |pmc=8791658 |doi=10.1093/jscr/rjab641 |url=}}</ref> | ||
*May be associated with [[neurofibromatosis 1]].<ref name=pmid25426397>{{cite journal |authors=Harrison B, Sammer D |title=Glomus tumors and neurofibromatosis: a newly recognized association |journal=Plast Reconstr Surg Glob Open |volume=2 |issue=9 |pages=e214 |date=September 2014 |pmid=25426397 |pmc=4229273 |doi=10.1097/GOX.0000000000000144 |url=}}</ref><ref name=pmid24685357>{{cite journal |authors=Kumar MG, Emnett RJ, Bayliss SJ, Gutmann DH |title=Glomus tumors in individuals with neurofibromatosis type 1 |journal=J Am Acad Dermatol |volume=71 |issue=1 |pages=44–8 |date=July 2014 |pmid=24685357 |doi=10.1016/j.jaad.2014.01.913 |url=}}</ref> | |||
Clinical: | Clinical - classic triad:<ref name=pmid36590779>{{cite journal |authors=Dhingra M, Niraula BB, Regmi A, Bansal S, Singh V, Phulware RH |title=Glomus Tumour of Hand--A Commonly Misdiagnosed Pathology: A Case Series |journal=J West Afr Coll Surg |volume=12 |issue=4 |pages=39–45 |date=2022 |pmid=36590779 |pmc=9802603 |doi=10.4103/jwas.jwas_171_22 |url=}}</ref> | ||
*[[ | *Pain - see ''[[painful skin lesion]]s''. | ||
*Point tenderness. | |||
*Cold intolerance. | |||
==Gross== | ==Gross== | ||
| Line 25: | Line 58: | ||
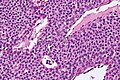
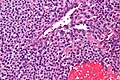
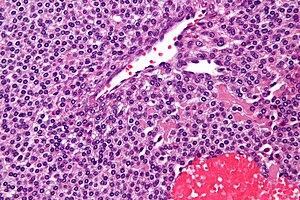
Features:<ref name=ouhsc>URL: [http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/Z0B003-PQ01-M.htm http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/Z0B003-PQ01-M.htm]. Accessed on: 19 October 2010.</ref> | Features:<ref name=ouhsc>URL: [http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/Z0B003-PQ01-M.htm http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/Z0B003-PQ01-M.htm]. Accessed on: 19 October 2010.</ref> | ||
*Sheets of equally-spaced cells ("cookie cutter appearance") - '''key feature'''. | *Sheets of equally-spaced cells ("cookie cutter appearance") - '''key feature'''. | ||
*Polygonal cells | *Polygonal cells +/- identifiable cellular borders. | ||
*Thin-walled blood vessels. | *Thin-walled blood vessels. | ||
**May vaguely resemble antlers ([[staghorn vessels]]). | **May vaguely resemble antlers ([[staghorn vessels]]). | ||
| Line 33: | Line 66: | ||
*No significant nuclear atypia. | *No significant nuclear atypia. | ||
*The regular cell spacing is called "cookie cutter appearance". It looks like the cells were created with a cookie cutter; the spacing between cell is equal and they all look very similar. | *The regular cell spacing is called "cookie cutter appearance". It looks like the cells were created with a cookie cutter; the spacing between cell is equal and they all look very similar. | ||
*Should be perivascular - abut endothelial cells. | |||
*Myxoid matrix common.<ref name=pmid25614464>{{cite journal |authors=Mravic M, LaChaud G, Nguyen A, Scott MA, Dry SM, James AW |title=Clinical and histopathological diagnosis of glomus tumor: an institutional experience of 138 cases |journal=Int J Surg Pathol |volume=23 |issue=3 |pages=181–8 |date=May 2015 |pmid=25614464 |pmc=4498398 |doi=10.1177/1066896914567330 |url=}}</ref> | |||
DDx - Why it is not a(n) ...<ref name=ouhsc>URL: [http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/Z0B003-PQ01-M.htm http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/Z0B003-PQ01-M.htm]. Accessed on: 19 October 2010.</ref> | |||
*[[Spiradenoma]] - also vascular and 'blue' but epithelial, often on the head (or at least chest and up). | |||
*Solid and cystic hidradenoma - epithelial and less 'blue' | |||
*[[Angiosarcoma]] - has nuclear atypia. | |||
*[[Dermatofibroma]] - spindle cell lesion. | |||
*[[Capillary hemangioma]] - no epithelioid cells, more blood vessels. | |||
===Images=== | |||
<gallery> | |||
Image:Glomus_tumour_-_intermed_mag.jpg | Glomus tumour - intermed. mag. (WC) | |||
Image:Glomus tumour - high mag.jpg | Glomus tumour - high mag. (WC) | |||
Image:Glomus tumour - very high mag.jpg | Glomus tumour - very high mag. (WC) | |||
Image:Glomus_tumour_-_2_-_very_high_mag.jpg | Glomus tumour - very high mag. (WC) | |||
</gallery> | |||
www: | |||
*[http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/Z0B003-PQ01-M.htm Glomus tumour (ouhsc.edu)]. | *[http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/Z0B003-PQ01-M.htm Glomus tumour (ouhsc.edu)]. | ||
==IHC== | |||
Features:<ref name=pmid9362106>{{cite journal |author=Hatori M, Aiba S, Kato M, Kamiya N, Kokubun S |title=Expression of CD34 in glomus tumors |journal=Tohoku J. Exp. Med. |volume=182 |issue=3 |pages=241–7 |year=1997 |month=July |pmid=9362106 |doi= |url=}}</ref> | Features:<ref name=pmid9362106>{{cite journal |author=Hatori M, Aiba S, Kato M, Kamiya N, Kokubun S |title=Expression of CD34 in glomus tumors |journal=Tohoku J. Exp. Med. |volume=182 |issue=3 |pages=241–7 |year=1997 |month=July |pmid=9362106 |doi= |url=}}</ref> | ||
*SMA +ve ~ 100%. | *SMA +ve ~ 100%. | ||
| Line 48: | Line 95: | ||
Others: | Others: | ||
*S100 -ve. | *S100 -ve. | ||
*Calponin +ve. | |||
* | |||
==Sign out== | ==Sign out== | ||
| Line 65: | Line 107: | ||
===Micro=== | ===Micro=== | ||
The sections show a tumour composed of | The sections show a tumour composed of polygonal cells with moderately distinct cellular borders and moderate cytoplasm. The tumour cell nuclei are round and have round nucleoli seen with the 10x objective. Thin-walled blood vessels with bland endothelial cells are found within the tumour. Tumour cells are identified immediately adjacent to the endothelial cells. No mitotic activity is apparent. Focal nuclear enlargement is present; however, no significant nuclear atypia is identified. | ||
==See also== | ==See also== | ||
Latest revision as of 18:42, 26 January 2023
| Glomus tumour | |
|---|---|
| Diagnosis in short | |
 Glomus tumour. H&E stain. | |
|
| |
| LM | sheets of equally-spaced cells ("cookie cutter appearance"), polygonal cells +/-identifiable cellular borders, thin-walled blood vessels, moderate clear cytoplasm |
| IHC | SMA +ve (100%), desmin usu. -ve, CD34 -ve, S-100 -ve |
| Site | skin/soft tissue - classically subungal (under the nail) |
|
| |
| Syndromes | +/-neurofibromatosis 1 |
|
| |
| Symptoms | painful skin lesion, cold intolerance, point tenderness |
| Prevalence | uncommon |
| Prognosis | usu. good (benign), rarely malignant |
| Treatment | excision |
Glomus tumours, also known as glomangioma, are painful, perivascular tumour that are classically periungual.
It should not be confused with paraganglioma, which were once called glomus tumour.
This tumour is classified as a perivascular tumour (also pericytic tumour) which is a subset of soft tissue tumours.
General
- Tumour derived from smooth muscle cell.[1]
- Usually benign.
- Malignant variant exists (known as glomangiosarcoma) - extremely rare.[2]
- May be associated with neurofibromatosis 1.[3][4]
Clinical - classic triad:[5]
- Pain - see painful skin lesions.
- Point tenderness.
- Cold intolerance.
Gross
Location:
- Classically subungual (under the nail).[6]
- Reported in almost very site imaginable.
- Most common GI site: stomach.[7]
Appearance (extradigital tumours):[6]
- Purplish papule.
Microscopic
Features:[8]
- Sheets of equally-spaced cells ("cookie cutter appearance") - key feature.
- Polygonal cells +/- identifiable cellular borders.
- Thin-walled blood vessels.
- May vaguely resemble antlers (staghorn vessels).
- Moderate clear cytoplasm.
Notes:
- No significant nuclear atypia.
- The regular cell spacing is called "cookie cutter appearance". It looks like the cells were created with a cookie cutter; the spacing between cell is equal and they all look very similar.
- Should be perivascular - abut endothelial cells.
- Myxoid matrix common.[9]
DDx - Why it is not a(n) ...[8]
- Spiradenoma - also vascular and 'blue' but epithelial, often on the head (or at least chest and up).
- Solid and cystic hidradenoma - epithelial and less 'blue'
- Angiosarcoma - has nuclear atypia.
- Dermatofibroma - spindle cell lesion.
- Capillary hemangioma - no epithelioid cells, more blood vessels.
Images
www:
IHC
Features:[10]
- SMA +ve ~ 100%.
- Desmin usu. -ve.
- CD34 -ve.
- Rarely +ve.
Others:
- S100 -ve.
- Calponin +ve.
Sign out
LESION, RIGHT RING FINGERNAIL, EXCISION: - GLOMUS TUMOUR. COMMENT: The tumour cells are positive for SMA.
Micro
The sections show a tumour composed of polygonal cells with moderately distinct cellular borders and moderate cytoplasm. The tumour cell nuclei are round and have round nucleoli seen with the 10x objective. Thin-walled blood vessels with bland endothelial cells are found within the tumour. Tumour cells are identified immediately adjacent to the endothelial cells. No mitotic activity is apparent. Focal nuclear enlargement is present; however, no significant nuclear atypia is identified.
See also
- Painful skin lesions.
- Myopericytoma - the other perivascular (soft tissue) tumour.
References
- ↑ Gombos Z, Zhang PJ (September 2008). "Glomus tumor". Arch. Pathol. Lab. Med. 132 (9): 1448–52. doi:10.1043/1543-2165(2008)132[1448:GT]2.0.CO;2. PMID 18788860.
- ↑ Alhroub OA, Mahameed SA, Abdelhafez MO, Alhroub A, Hour H, Hasasna N, Kamal N (January 2022). "A case of malignant glomus tumor (glomangiosarcoma) of the nasal cavity". J Surg Case Rep 2022 (1): rjab641. doi:10.1093/jscr/rjab641. PMC 8791658. PMID 35096369. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8791658/.
- ↑ Harrison B, Sammer D (September 2014). "Glomus tumors and neurofibromatosis: a newly recognized association". Plast Reconstr Surg Glob Open 2 (9): e214. doi:10.1097/GOX.0000000000000144. PMC 4229273. PMID 25426397. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4229273/.
- ↑ Kumar MG, Emnett RJ, Bayliss SJ, Gutmann DH (July 2014). "Glomus tumors in individuals with neurofibromatosis type 1". J Am Acad Dermatol 71 (1): 44–8. doi:10.1016/j.jaad.2014.01.913. PMID 24685357.
- ↑ Dhingra M, Niraula BB, Regmi A, Bansal S, Singh V, Phulware RH (2022). "Glomus Tumour of Hand--A Commonly Misdiagnosed Pathology: A Case Series". J West Afr Coll Surg 12 (4): 39–45. doi:10.4103/jwas.jwas_171_22. PMC 9802603. PMID 36590779. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9802603/.
- ↑ 6.0 6.1 Lee, DW.; Yang, JH.; Chang, S.; Won, CH.; Lee, MW.; Choi, JH.; Moon, KC. (Dec 2011). "Clinical and pathological characteristics of extradigital and digital glomus tumours: a retrospective comparative study.". J Eur Acad Dermatol Venereol 25 (12): 1392-7. doi:10.1111/j.1468-3083.2011.03979.x. PMID 21371130.
- ↑ Miettinen, M.; Paal, E.; Lasota, J.; Sobin, LH. (Mar 2002). "Gastrointestinal glomus tumors: a clinicopathologic, immunohistochemical, and molecular genetic study of 32 cases.". Am J Surg Pathol 26 (3): 301-11. PMID 11859201.
- ↑ 8.0 8.1 URL: http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/Z0B003-PQ01-M.htm. Accessed on: 19 October 2010.
- ↑ Mravic M, LaChaud G, Nguyen A, Scott MA, Dry SM, James AW (May 2015). "Clinical and histopathological diagnosis of glomus tumor: an institutional experience of 138 cases". Int J Surg Pathol 23 (3): 181–8. doi:10.1177/1066896914567330. PMC 4498398. PMID 25614464. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4498398/.
- ↑ Hatori M, Aiba S, Kato M, Kamiya N, Kokubun S (July 1997). "Expression of CD34 in glomus tumors". Tohoku J. Exp. Med. 182 (3): 241–7. PMID 9362106.