Gastroesophageal reflux disease
Jump to navigation
Jump to search
The printable version is no longer supported and may have rendering errors. Please update your browser bookmarks and please use the default browser print function instead.
| Gastroesophageal reflux disease | |
|---|---|
| Diagnosis in short | |
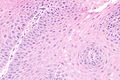
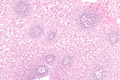
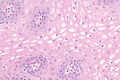
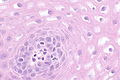
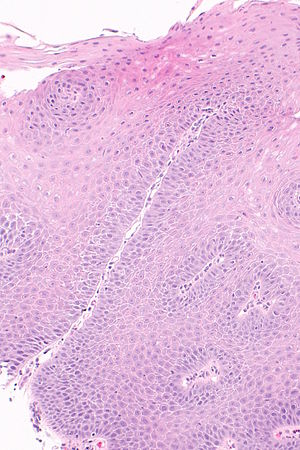 Micrograph showing histology compatible with gastroesophageal reflux disease. H&E stain. | |
|
| |
| LM | basal cell hyperplasia (> 3 cells thick or >15% of epithelial thickness), papillae elongated (papillae reach into the top 1/3 of the epithelial layer), inflammation, esp. eosinophils, lymphocytes with convoluted nuclei ("squiggle cells"), +/-intraepithelial edema, +/-apoptotic cells, +/-glycogenation |
| LM DDx | intestinal metaplasia (Barrett's esophagus), eosinophilic esophagitis, acute esophagitis |
| Site | esophagus |
|
| |
| Associated Dx | obesity, Barrett's esophagus |
| Prevalence | common |
| Endoscopy | erythema, erosions, +/-ulceration. |
| Prognosis | benign |
| Clin. DDx | eosinophilic esophagitis, acute esophagitis |
| Treatment | proton pump inhibitors |
Gastroesophageal reflux disease, abbreviated GERD, is a common pathology of the esophagus. It is occasionally abbreviated GORD (gastro-oesophageal reflux disease).
Reflux esophagitis redirects here. It technically isn't a synonym.[1][2]
General
Clinical:
- Usually chest pain
- +/-Abdominal pain.
- +/-Vomiting.
- +/-Blood loss.
Treatment:
- Treated with proton pump inhibitors (PPIs).
DDx (clinical):
Gross
- Erythema.
- Erosions.
- +/-Ulceration.
Note:
- Many be graded using Savary-Miller classification or Los Angeles classification.[3]
Images:
Los Angeles classification for GERD
Features:[4]
| Classification | Description |
|---|---|
| A | mucosal break <=5 mm, not beyond the tops of two (adjacent) mucosal folds |
| B | mucosal break >5 mm, not beyond the tops of two (adjacent) mucosal folds |
| C | mucosa break beyond the tops of two mucosal folds but <75% of the esophageal circumference |
| D | mucosal break >=75% of the esophageal circumference |
Note:
- Correlation with histology is poor; mucosal breaks are seen rarely.[3]
Microscopic
Features:
- Basal cell hyperplasia;[5] > 3 cells thick or >15% of epithelial thickness.
- Papillae elongated; papillae reach into the top 1/3 of the epithelial layer.[6]
- Inflammation, esp. eosinophils, lymphocytes with convoluted nuclei ("squiggle cells").
- +/-Intraepithelial edema.
- +/-Apoptotic cells.[7]
- +/-Glycogen - cytoplasm cleared (white).[8]
Notes:
- Intraepithelial cells with irregular nuclear contours, "squiggle cells" (T lymphocytes[9]), may mimic neutrophils.
- Changes may be focal.
- PPI effect may be seen in a concurrent gastric biopsy.
- Perinuclear clearing may be seen.[10]
DDx:
- Eosinophilic esophagitis - characterized by similar histomorphologic features. The key difference is: more eosinophils.
- Barrett's esophagus - intestinal metaplasia may be minimal.
Images
www:
Stains
- Oil red O stain +ve in macrophages from bronchoalveolar lavage specimens.[12]
Sign out
Poorly oriented
ESOPHAGUS, BIOPSY: - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, INTRAEPITHELIAL EDEMA AND RARE INTRAEPITHELIAL EOSINOPHILS -- COMPATIBLE WITH GASTROESOPHAGEAL REFLUX.
Columnar epithelium present
ESOPHAGUS, BIOPSY: - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, INTRAEPITHELIAL EDEMA AND RARE INTRAEPITHELIAL EOSINOPHILS -- COMPATIBLE WITH GASTROESOPHAGEAL REFLUX. - COLUMNAR EPITHELIUM WITH MODERATE CHRONIC INACTIVE INFLAMMATION. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Ulceration present
ESOPHAGUS, DISTAL, BIOPSY: - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, INTRAEPITHELIAL EDEMA, RARE INTRAEPITHELIAL EOSINOPHILS AND EVIDENCE OF ULCERATION -- COMPATIBLE WITH GASTROESOPHAGEAL REFLUX. - COLUMNAR EPITHELIUM WITH MODERATE CHRONIC INACTIVE INFLAMMATION. - NEGATIVE FOR INTESTINAL METAPLASIA. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: PAS-D staining is negative for microorganisms.
BE and GERD present
ESOPHAGUS (DISTAL), BIOPSY: - COLUMNAR EPITHELIUM WITH INTESTINAL METAPLASIA AND MODERATE CHRONIC INFLAMMATION, SEE COMMENT. - SQUAMOUS MUCOSA WITH BASAL CELL HYPERPLASIA, INTRAEPITHELIAL EDEMA AND RARE INTRAEPITHELIAL EOSINOPHILS -- COMPATIBLE WITH GASTROESOPHAGEAL REFLUX. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: The findings are consistent with Barrett's esophagus in the appropriate endoscopic setting.
See also
References
- ↑ Orbelo, DM.; Enders, FT.; Romero, Y.; Francis, DL.; Achem, SR.; Dabade, TS.; Crowell, MD.; Geno, DM. et al. (Jan 2014). "Once-Daily Omeprazole/Sodium Bicarbonate Heals Severe Refractory Reflux Esophagitis with Morning or Nighttime Dosing.". Dig Dis Sci. doi:10.1007/s10620-013-3017-y. PMID 24448652.
- ↑ Karbasi, A.; Ardestani, ME.; Ghanei, M.; Harandi, AA. (Jun 2013). "The association between reflux esophagitis and airway hyper-reactivity in patients with gastro-esophageal reflux.". J Res Med Sci 18 (6): 473-6. PMID 24250694.
- ↑ 3.0 3.1 Genta, RM.; Spechler, SJ.; Kielhorn, AF. (Jan 2011). "The Los Angeles and Savary-Miller systems for grading esophagitis: utilization and correlation with histology.". Dis Esophagus 24 (1): 10-7. doi:10.1111/j.1442-2050.2010.01092.x. PMID 20659145.
- ↑ URL: http://www.sciencedirect.com/science/article/pii/S2212097113700463. Accessed on: 14 April 2015
- ↑ Steiner, SJ.; Kernek, KM.; Fitzgerald, JF. (May 2006). "Severity of basal cell hyperplasia differs in reflux versus eosinophilic esophagitis.". J Pediatr Gastroenterol Nutr 42 (5): 506-9. doi:10.1097/01.mpg.0000221906.06899.1b. PMID 16707971.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 804. ISBN 0-7216-0187-1.
- ↑ Wetscher GJ, Schwelberger H, Unger A, et al. (December 1998). "Reflux-induced apoptosis of the esophageal mucosa is inhibited in Barrett's epithelium". Am. J. Surg. 176 (6): 569–73. PMID 9926792.
- ↑ Vadva MD, Triadafilopoulos G (July 1993). "Glycogenic acanthosis of the esophagus and gastroesophageal reflux". J. Clin. Gastroenterol. 17 (1): 79–83. PMID 8409304.
- ↑ Cucchiara, S.; D'Armiento, F.; Alfieri, E.; Insabato, L.; Minella, R.; De Magistris, TM.; Scoppa, A. (Nov 1995). "Intraepithelial cells with irregular nuclear contours as a marker of esophagitis in children with gastroesophageal reflux disease.". Dig Dis Sci 40 (11): 2305-11. PMID 7587806.
- ↑ URL: http://155.37.5.42/eAtlas/GI/1262.htm. Accessed on: 31 January 2014.
- ↑ Genevay, M.; Rubbia-Brandt, L.; Rougemont, AL. (Jun 2010). "Do eosinophil numbers differentiate eosinophilic esophagitis from gastroesophageal reflux disease?". Arch Pathol Lab Med 134 (6): 815-25. doi:10.1043/1543-2165-134.6.815. PMID 20524860.
- ↑ Hopkins, PM.; Kermeen, F.; Duhig, E.; Fletcher, L.; Gradwell, J.; Whitfield, L.; Godinez, C.; Musk, M. et al. (Aug 2010). "Oil red O stain of alveolar macrophages is an effective screening test for gastroesophageal reflux disease in lung transplant recipients.". J Heart Lung Transplant 29 (8): 859-64. doi:10.1016/j.healun.2010.03.015. PMID 20466562.