Fungi
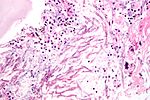
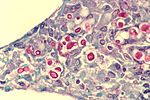
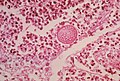
Fungi (aspergillus). H&E stain.
Fungi (singular fungus) are microorganisms that are occasionally seen by pathologists.
Overview
- There are lots of 'em. Below are a few of 'em.
Terminology:[1]
- Hyphae = microscopic filamentous growth (of fungi) -- single cell.
- Mycelial = filamentous network of hyphae.
- Septae/septation = hyphae may be subdivided by septae -- if they aren't they are one mass of protoplasm. (?)
- Dimorphism = exist in two forms; e.g. single cell (yeast) and mycelial growth.
- Pseudohyphae = looks like hyphae --but branching pattern is created by separate cells.[2]
Tissue invasive fungi
Typically:[3]
Summary table
| Name (disease) | Kingdom | Size | Shape | Stains | Other (microscopic) | Clinical | References | Image |
|---|---|---|---|---|---|---|---|---|
| Aspergillus (aspergillosis) | Fungi | ? | Hyphae that branching with 45 degrees angle |
PAS-D | Fruiting heads when aerobic | ? Immunosuppression | [4] | |
| Zygomycota (zygomycosis); more specific Mucorales (mucormycosis) |
Fungi | ? | Branching hyphae with variable width | ? | Granulomata assoc. | Diabetes, immunodeficient | [4] | |
| Coccidioides, usually C. immitis (coccidioidomycosis) |
Fungi | Large - 20-60 micrometers, endospores 1-5 micrometers |
Spherules | Stains? | Other? | Immunodeficient | [4] | Coccidioidomycosis (med.sc.edu) |
| Histoplasma (histoplasmosis) | Fungi | 2-5 micrometers | Spherical | GMS | Intracellular (unlike candida), granulomata | Source: soil with bird droppings | [4] | |
| Blastomyces (blastomycosis) | Fungi | 5-15 micrometres | Spherical (yeast) | Stains? | Granulomas, broad-based budding yeast | Habitat: Northeast America, Africa | [4][5] | |
| Paracoccidioides (paracoccidioidomycosis) | Fungi | 6-60 micrometres | Spherical (yeast) | Stains? | Multiple budding "steering wheel" appearance | Clinical??? | [4] | |
| Pneumocystis jirovecii (pneumocystis carinii pneumonia; abbrev. PCP) | Fungi (previously thought to be a protozoan) | 7-8 micrometres | "Dented ping-pong ball" | GMS | Usually in clusters of alveolar casts with a honeycomb appearance | HIV/AIDS associated | [6] | |
| Cryptococcus (cryptococcosis) | Fungi | 5-15 micrometres | Yeast | GMS | Prominent (i.e. thick polysaccharide) capsule | HIV/AIDS associated, most common CNS fungus | [4] |
Notes:
- Bold text = key features.
Specific fungi
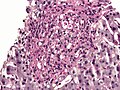
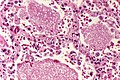
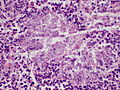
Histoplasmosis
General
- Organism: Histoplasma.
- Specific organism: Histoplasma capulatum.
- Typical location: lung.
- Common in immunosuppressed individuals, e.g. HIV/AIDS population.
- Extrapulmonary or disseminated histoplasmosis is considered to be AIDS-defining.[7]
Microscopic
Features:
- Often in yeast form - in tissue, spherical, 2-5 micrometres.[8]
- Intracellular[9] - may be within macrophages that form a granuloma.
- Nice bright red on PAS-D.
- Have a "central dot".[10]
- Nice bright red on PAS-D.
Images
Histoplasmosis - granuloma - PASD stain. (WC)
Histoplasmosis - PASD stain. (WC)
Histoplasmosis - GMS stain. (WC)
www:
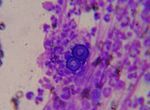
Coccidioidomycosis
General
- Organism: Coccidioides.
- Specific organism: Coccidioides immitis.
- Usu. from soil.
- Typical locations: lung, oral cavity.[11]
- +/-Immunodeficiency.[12]
- Predominantly southwest USA and Mexico.[13]
Microscopic
Features:
- Forms spherules 60-80 μm in size.[8]
- Contain endospores 1-5 μm in diameter.
Notes:
- Spherules may be described as a "bag of marbles".
Images
www:
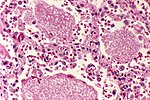
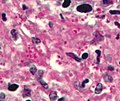
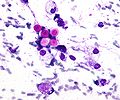
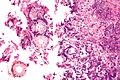
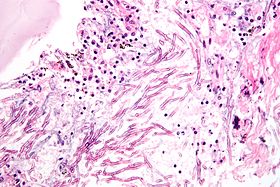
Pneumocystis pneumonia
Main article: Pneumonia
- Abbreviated PCP.
- AKA Pneumocystis jirovecii pneumonia.
General
- Organism: pneumocystis,
- Specific organism: Pneumocystis jirovecii[15] (used to be called Pneumocystis carinii).
- May be spelled Pneumocystis jiroveci.
- Fungus... used to be considered a parasite.
- Typical location: lung.
Clinical:
- Opportunistic infection - typically in HIV +ve individuals.
- May have subtle findings on chest X-ray.
Microscopic
Features:
- Form frothy aggregates that take the shape of the alveoli they sit within, i.e. they form "alveolar casts".
- "Dented ping-pong ball" appearance.[8] **Remember PCP = ping-pong.
- Approximately 7-8 μm in size.
Images
www:
Stains
- GMS stain +ve.
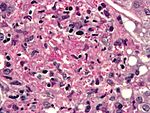
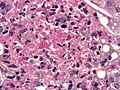
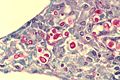
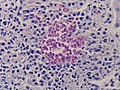
Cryptococcosis
General
- Organism: Cryptococcus.
- Specific organism: C. neoformans.
- Opportunistic infection.
- Typical location: lung.
- Most common fungus seen in CSF specimens.[4]
Trivia:
- Crypto- = hidden/invisible.[16]
- Why the name? A. The capsule is almost invisible.
Gross
Features (brain):
- Small cystic spaces, often diffuse.
- Known as "soap bubble brain".
Image:
Microscopic
Features:
- Yeast:
- Usually accompanied by very little inflammation.[17]
Notes:
- May be confused with corpora amylacea in the CNS, esp. as they (like cryptococci) stain for methenamine silver, Alcian blue, and PAS.[18]
Images
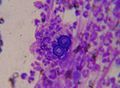
Cryptococcosis - cytology - Field stain. (WC)
www:
Cryptosporidiosis
General
- Caused by cryptosporidium.
- Fecal-oral transmission.
- Usu. in immunoincompetent individuals, e.g. HIV/AIDS.
Microscopic
Features:
- Uniform spherical nodules 2-4 micrometres in diameter, typical location - GI tract brush border.
- Bluish staining of brush border key feature - low power.
Images
www:
- Schematic picture of cryptosporidium & bowel (tulane.edu).
- Micrograph of cryptosporidiosis (brown.edu).
Notes:
- Cryptosporidium parvum?[19]
Candidiasis
- In the context of pap tests see: Gynecologic_cytopathology#Candida.
General
- Commonly Candida albicans.
- Yeast forms.
- Locations: oral cavity, vagina.
Microscopic
Features:
- Dimorphic - seen in two forms:
Notes:
- May be described as "sticks and stones".
Images
www:
Stains
Features:
- PAS +ve.
- Methenamine silver +ve.
Blastomycosis
General
- Usually Blastomyces dermatitidis - fungus.
- May be in the oral cavity.[11]
Microscopic
Features:
- Broad-based budding yeast -- is Blastomyces.[21]
- The interface between two separating fungi, i.e. fungi in the process of reproducing, is very large.
DDx:
Images
www:
- Blastomycosis - budding (pathguy.com).
- Blastomycosis - with broad budding (lahey.org).
- Blastomyces (med.sc.edu).
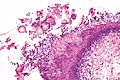
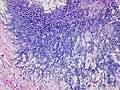
Mucormycosis
General
- Causative organism: Mucorales.
- Kingdom: Fungi.
- AKA Zygomycota (zygomycosis).
- Associated with diabetes, immunodeficiency.
Microscopic
Features:[4]
- Branching hyphae with variable width.
- Granulomata associated.
Notes:
- Not septated.
- Branching angle typically ~90 degrees.
DDx:
Images
Zygomycosis - cytology. (WC)
www:
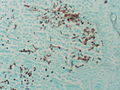
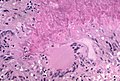
Aspergillosis
General
- Due to Aspergillus.
- Fungus.
- Associated with immunosuppression/immunodeficiency.
- Rarely in immune competent individuals.[22]
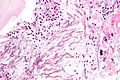
Microscopic
Features:
- Hyphae that branching with 45 degrees angle - key feature.[4]
- Uniform width - typically ~3-5 μm.
- Septated - often difficult to see.
- "Fruiting heads" when aerobic - uncommon.
- Spherical structures ~50 micrometres in diameter with radially arranged structures (like spokes of a wheel) +/- an empty centre in the plane of section.
DDx:
- Mucormycosis - irregular width.
- Scedosporium prolificans - in immunoincompetent individuals.[23]
Images
Aspergillus - cytology. (WC)
www:
Stains
- PAS-D +ve.
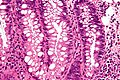
Microsporidiosis
General
- A group of (extremely) small intracellular microorganisms - classified as fungi.[25]
- Human pathogenic organisms in this group include: Enterocytozoon bieneusi, Encephalitozoon hellem, and Encephalitozoon intestinalis.[26]
- Important in the context of HIV/AIDS,[27] and solid organ transplant recipients.
- May be seen in immune competent individuals.[26]
Clinical:[26]
- Diarrhea.
- Weight loss.
- Abdominal pain.
Microscopic
Features:
- Partial villus atrophy (villous blunting) and crypt hyperplasia.[26]
- Small intracellular microorganisms ~ 1.0-4.0 μm.
Images:
EM
- Small intracellular microorganisms ~ 1.0-4.0 μm.[25]
Image:
See also
References
- ↑ http://www.fungionline.org.uk/1intro/3growth_forms.html
- ↑ http://pathmicro.med.sc.edu/mycology/mycology-3.htm
- ↑ CM 17 Apr 2009.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 682. ISBN 978-1416025887.
- ↑ http://pathmicro.med.sc.edu/mycology/mycology-6.htm
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 684. ISBN 978-1416025887.
- ↑ Schneider E, Whitmore S, Glynn KM, Dominguez K, Mitsch A, McKenna MT (December 2008). "Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years--United States, 2008". MMWR Recomm Rep 57 (RR-10): 1–12. PMID 19052530. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5710a1.htm.
- ↑ 8.0 8.1 8.2 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 103. ISBN 978-0781765275.
- ↑ Gorocica, P.; Taylor, ML.; Alvarado-Vásquez, N.; Pérez-Torres, A.; Lascurain, R.; Zenteno, E. (May 2009). "The interaction between Histoplasma capsulatum cell wall carbohydrates and host components: relevance in the immunomodulatory role of histoplasmosis.". Mem Inst Oswaldo Cruz 104 (3): 492-6. PMID 19547878.
- ↑ 10.0 10.1 URL: http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/A6I001-PQ01-M.htm. Accessed on: 19 October 2010
- ↑ 11.0 11.1 11.2 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 3. ISBN 978-0781765275.
- ↑ Nguyen, C.; Barker, BM.; Hoover, S.; Nix, DE.; Ampel, NM.; Frelinger, JA.; Orbach, MJ.; Galgiani, JN. (Jul 2013). "Recent advances in our understanding of the environmental, epidemiological, immunological, and clinical dimensions of coccidioidomycosis.". Clin Microbiol Rev 26 (3): 505-25. doi:10.1128/CMR.00005-13. PMID 23824371.
- ↑ Welsh, O.; Vera-Cabrera, L.; Rendon, A.; Gonzalez, G.; Bonifaz, A.. "Coccidioidomycosis.". Clin Dermatol 30 (6): 573-91. doi:10.1016/j.clindermatol.2012.01.003. PMID 23068145.
- ↑ URL: http://library.med.utah.edu/WebPath/EXAM/IMGQUIZ/pufrm.html. Accessed on: 4 December 2011.
- ↑ Redhead, SA.; Cushion, MT.; Frenkel, JK.; Stringer, JR.. "Pneumocystis and Trypanosoma cruzi: nomenclature and typifications.". J Eukaryot Microbiol 53 (1): 2-11. doi:10.1111/j.1550-7408.2005.00072.x. PMID 16441572.
- ↑ URL: http://en.wiktionary.org/wiki/crypto-. Accessed on: 12 April 2012.
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 423 Q29. ISBN 978-1416025887.
- ↑ URL: http://flylib.com/books/en/2.953.1.17/1/. Accessed on: 15 December 2010.
- ↑ http://www.dpd.cdc.gov/dpdx/HTML/Cryptosporidiosis.htm
- ↑ http://pathmicro.med.sc.edu/mycology/mycology-3.htm
- ↑ Veligandla, SR.; Hinrichs, SH.; Rupp, ME.; Lien, EA.; Neff, JR.; Iwen, PC. (Oct 2002). "Delayed diagnosis of osseous blastomycosis in two patients following environmental exposure in nonendemic areas.". Am J Clin Pathol 118 (4): 536-41. doi:10.1309/JEJ0-3N98-C3G8-21DE. PMID 12375640.
- ↑ Sugimura, S.; Yoshida, K.; Oba, H.; Hashiguchi, K.; Nakajima, M.; Moriya, O.; Okimoto, N.; Niki, Y. et al. (Oct 1994). "[Two cases of invasive pulmonary aspergillosis in non-immunocompromised hosts].". Nihon Kyobu Shikkan Gakkai Zasshi 32 (10): 1032-7. PMID 7844909.
- ↑ URL: http://path.upmc.edu/cases/case290.html. Accessed on: 14 January 2012.
- ↑ URL: http://www.ispub.com/journal/the-internet-journal-of-otorhinolaryngology/volume-6-number-1/maxillary-sinus-mycetoma-due-to-aspergillus-niger.html. Accessed on: 27 February 2012.
- ↑ 25.0 25.1 Didier, ES. (Apr 2005). "Microsporidiosis: an emerging and opportunistic infection in humans and animals.". Acta Trop 94 (1): 61-76. doi:10.1016/j.actatropica.2005.01.010. PMID 15777637.
- ↑ 26.0 26.1 26.2 26.3 Didier, ES.; Weiss, LM. (Oct 2011). "Microsporidiosis: not just in AIDS patients.". Curr Opin Infect Dis 24 (5): 490-5. doi:10.1097/QCO.0b013e32834aa152. PMID 21844802.
- ↑ Orenstein, JM.. "Diagnostic pathology of microsporidiosis.". Ultrastruct Pathol 27 (3): 141-9. PMID 12775504.
- ↑ URL: http://wwwnc.cdc.gov/eid/article/18/2/11-1319_article.htm. Accessed on: 2 June 2012.