Difference between revisions of "Epithelial-myoepithelial carcinoma"
Jump to navigation
Jump to search
(split out) |
(+infobox) |
||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
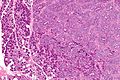
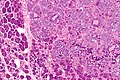
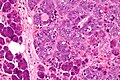
| Image = Epithelial-myoepithelial carcinoma - very high mag.jpg | |||
| Width = | |||
| Caption = Epithelial-myoepithelial carcinoma. [[H&E stain]]. | |||
| Micro = biphasic tumour with (1) epithelial layer, and (2) myoepithelial layer; variable architecture (solid, cystic, tubular, papillary); +/- spindle cells | |||
| Subtypes = | |||
| LMDDx = [[adenoid cystic carcinoma]] (tubular variant), [[pleomorphic adenoma]], tubular variant. | |||
| Stains = | |||
| IHC = CAM5.2 +ve (epithelial comp.), p63 +ve (myoepithelial comp.) | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[salivary gland]] - usually parotid gland | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = | |||
| Signs = salivary gland mass | |||
| Symptoms = | |||
| Prevalence = very rare | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = | |||
| Other = | |||
| ClinDDx = other [[salivary gland]] masses | |||
}} | |||
Epithelial-myoepithelial carcinoma, abbreviated '''EMCa''', is a rare malignant [[salivary gland]] tumour. | Epithelial-myoepithelial carcinoma, abbreviated '''EMCa''', is a rare malignant [[salivary gland]] tumour. | ||
Revision as of 13:11, 30 July 2013
| Epithelial-myoepithelial carcinoma | |
|---|---|
| Diagnosis in short | |
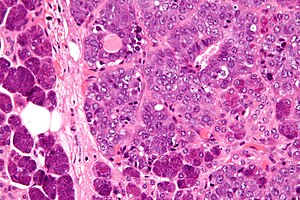 Epithelial-myoepithelial carcinoma. H&E stain. | |
|
| |
| LM | biphasic tumour with (1) epithelial layer, and (2) myoepithelial layer; variable architecture (solid, cystic, tubular, papillary); +/- spindle cells |
| LM DDx | adenoid cystic carcinoma (tubular variant), pleomorphic adenoma, tubular variant. |
| IHC | CAM5.2 +ve (epithelial comp.), p63 +ve (myoepithelial comp.) |
| Site | salivary gland - usually parotid gland |
|
| |
| Signs | salivary gland mass |
| Prevalence | very rare |
| Clin. DDx | other salivary gland masses |
Epithelial-myoepithelial carcinoma, abbreviated EMCa, is a rare malignant salivary gland tumour.
General
- Rare ~1% of salivary gland tumours.[1]
- Female:male = 1.5:1.[2]
- Usu. older people - 50s or 60s.
- Usu. parotid gland ~ 60% of cases.[2]
- Prognosis: usually good; 5-year and 10-year survival over 90% and 80% respectively.[2]
Notes:
- Most common malignant component in carcinoma ex pleomorphic adenoma.
- May be the same tumour as adenomyoepithelioma of the breast.[3]
Microscopic
Features:
- Biphasic tumour:[2]
- Epithelial layer.
- Myoepithelial layer - key feature.
- Architecture: variable (solid, cystic, tubular, papillary).
- +/-Spindle cells.
- Basement membrane-like material; may mimic adenoid cystic carcinoma.
Notes:
- Usually few mitoses.
DDx:
- Adenoid cystic carcinoma (tubular variant).
- Pleomorphic adenoma, tubular variant.
- Has focal epithelial-myoepithelial carcinoma-like areas.
Images
www:
IHC
- CAM5.2 +ve -- epithelial component.
- p63 +ve -- myoepithelial component.
See also
References
- ↑ Tralongo, V.; Daniele, E.. "Epithelial-myoepithelial carcinoma of the salivary glands: a review of literature.". Anticancer Res 18 (1B): 603-8. PMID 9568184.
- ↑ 2.0 2.1 2.2 2.3 Seethala, RR.; Barnes, EL.; Hunt, JL. (Jan 2007). "Epithelial-myoepithelial carcinoma: a review of the clinicopathologic spectrum and immunophenotypic characteristics in 61 tumors of the salivary glands and upper aerodigestive tract.". Am J Surg Pathol 31 (1): 44-57. doi:10.1097/01.pas.0000213314.74423.d8. PMID 17197918.
- ↑ Seifert, G. (Sep 1998). "Are adenomyoepithelioma of the breast and epithelial-myoepithelial carcinoma of the salivary glands identical tumours?". Virchows Arch 433 (3): 285-8. PMID 9769134.
- ↑ [http://www.pathologyimagesinc.com/sgt-cytopath/epith-myoepith-ca/cytopathology/fs-emc-cytopath-feat.html "Cytopathologic Features of Epithelial-myoepithelial Carcinoma"]. http://www.pathologyimagesinc.com/sgt-cytopath/epith-myoepith-ca/cytopathology/fs-emc-cytopath-feat.html. Retrieved January 18, 2011.