Endometrioid endometrial carcinoma
Jump to navigation
Jump to search
- AKA endometrioid endometrial adenocarcinoma.
General
- Good prognosis - usually.
- Women in 40s & 50s.
- Associated with estrogen excess.
- Typical patient is obese.
Gross
- Thickened endometrium.
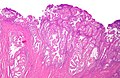
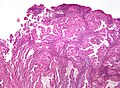
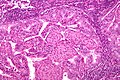
Microscopic
Features:
- Atypical (ovoid) glands with - one of the following four:[1][2][3]
- Desmoplastic stromal response.
- Confluent cribriform growth. †
- Extensive papillary growth. †
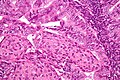
- Severe cytologic atypia. †
- Squamous metaplasia - very common.
- Look for squamous morules:
- Ball of cells with an intensely eosinophilic cytoplasm - key feature.
- Central nucleus.
- Intercellular bridges - may be hard to find.
- +/-Dyskeratotic cells.
- Look for squamous morules:
Notes:
- † There is a size cut-off for criteria 2, 3 and 4: > 2.1 mm.[2]
- Dyskeratosis = abnormal keratinization;[4] classically have intensely eosinophilic cytoplasm +/- nuclear fragmentation (karyorrhexis) - see: several dyskeratotic cells.
- Squamous metaplasia != neoplastic -- it may occur due to hormones.[5]
- Squamous morules in endometrioid endometrial carcinoma - not associated with HPV infection.[6]
DDx:
- Complex endometrial hyperplasia with atypia.
- Complex endometrial hyperplasia.
- Microglandular hyperplasia of the cervix.
- Endocervical adenocarcinoma.
- Serous carcinoma of the endometrium - esp. if high-grade nuclear features are present diffusely.
- Clear cell carcinoma of the endometrium - esp. when clear cells present.
Images
www:
IHC
- Vimentin +ve.
- ER +ve.
- PR +ve.
Others:
- p16 -ve -- positive in serous endometrial carcinoma[7] and endocervical adenocarcinoma.
- CEA -ve.
Sign out
ENDOMETRIUM, BIOPSY: - ENDOMETRIOID ENDOMETRIAL ADENOCARCINOMA, FIGO GRADE I/III.
Micro
The sections show endometrium with complex, fused and cribriform glands with scant intervening stroma over a region measuring greater than 2.1 millimetres. Focally, a desmoplastic stroma is also identified. No nuclear atypia is appreciated.
Endocervical versus endometrial - biopsy
The foamy histiocytes in the stroma and lack of desmoplasia slightly favour an endometrial origin; however, the lesion would be best classified with an excisional specimen and in conjunction with the clinical impression.
See also
- [[Endometrial carcinoma
References
- ↑ Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 239. ISBN 978-0443069208.
- ↑ 2.0 2.1 Kurman, RJ.; Norris, HJ. (Jun 1982). "Evaluation of criteria for distinguishing atypical endometrial hyperplasia from well-differentiated carcinoma.". Cancer 49 (12): 2547-59. PMID 7074572.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Endometrium_11protocol.pdf. Accessed on: 12 January 2012.
- ↑ URL: http://dictionary.reference.com/browse/dyskeratosis. Accessed on: 5 September 2011.
- ↑ Miranda, MC.; Mazur, MT. (May 1995). "Endometrial squamous metaplasia. An unusual response to progestin therapy of hyperplasia.". Arch Pathol Lab Med 119 (5): 458-60. PMID 7748076.
- ↑ Chinen, K.; Kamiyama, K.; Kinjo, T.; Arasaki, A.; Ihama, Y.; Hamada, T.; Iwamasa, T. (Sep 2004). "Morules in endometrial carcinoma and benign endometrial lesions differ from squamous differentiation tissue and are not infected with human papillomavirus.". J Clin Pathol 57 (9): 918-26. doi:10.1136/jcp.2004.017996. PMID 15333650.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedpmid17581420