Difference between revisions of "Endometrioid endometrial carcinoma"
m (→General) |
|||
| Line 17: | Line 17: | ||
| Site = [[endometrium]] - see ''[[endometrial carcinoma]]'' | | Site = [[endometrium]] - see ''[[endometrial carcinoma]]'' | ||
| Assdx = [[obesity]] | | Assdx = [[obesity]] | ||
| Syndromes = | | Syndromes = [[Lynch syndrome]], [[Cowden syndrome]] | ||
| Clinicalhx = | | Clinicalhx = | ||
| Signs = [[abnormal uterine bleeding]] (AUB) | | Signs = [[abnormal uterine bleeding]] (AUB) | ||
Revision as of 00:06, 23 January 2014
| Endometrioid endometrial carcinoma | |
|---|---|
| Diagnosis in short | |
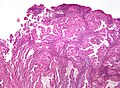
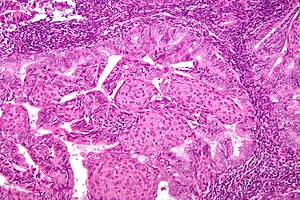 Endometrioid endometrial adenocarcinoma. H&E stain. | |
|
| |
| Synonyms | endometrioid endometrial adenocarcinoma |
| LM DDx | complex endometrial hyperplasia, microglandular hyperplasia of the cervix, endocervical adenocarcinoma, serous carcinoma of the endometrium - esp. for high-grade tumours, clear cell carcinoma of the endometrium, simple endometrial hyperplasia, endometrium with squamous morules |
| IHC | ER +ve, PR +ve, vimentin +ve, p16 -ve, CEA -ve |
| Gross | endometrial thickening |
| Site | endometrium - see endometrial carcinoma |
|
| |
| Associated Dx | obesity |
| Syndromes | Lynch syndrome, Cowden syndrome |
|
| |
| Signs | abnormal uterine bleeding (AUB) |
| Prevalence | common |
| Prognosis | good - esp. low-grade |
| Treatment | usu. total hysterectomy |
Endometrioid endometrial carcinoma, abbreviated EEC, is the most common type of endometrial carcinoma. It is strongly associated with obesity.
It is also known as endometrioid endometrial adenocarcinoma.
General
- Good prognosis - usually.
- Women in 40s & 50s.
- Associated with estrogen excess.
- Typical patient is obese.
Associated syndromes:
Gross
- Thickened endometrium.
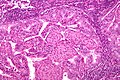
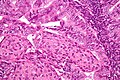
Microscopic
Features:
- Atypical (ovoid) glands with - one of the following four:[3][4][5]
- Desmoplastic stromal response.
- Confluent cribriform growth. †
- Extensive papillary growth. †
- Severe cytologic atypia. †
- Squamous metaplasia - very common.
- Look for squamous morules:
- Ball of cells with an intensely eosinophilic cytoplasm - key feature.
- Central nucleus.
- Intercellular bridges - may be hard to find.
- +/-Dyskeratotic cells.
- Look for squamous morules:
Notes:
- † There is a size cut-off for criteria 2, 3 and 4: > 2.1 mm.[4]
- Dyskeratosis = abnormal keratinization;[6] classically have intensely eosinophilic cytoplasm +/- nuclear fragmentation (karyorrhexis) - see: several dyskeratotic cells.
- Squamous metaplasia != neoplastic -- it may occur due to hormones.[7]
- Squamous morules in endometrioid endometrial carcinoma - not associated with HPV infection.[8]
DDx:
- Complex endometrial hyperplasia with atypia.
- Complex endometrial hyperplasia.
- Microglandular hyperplasia of the cervix.
- Endocervical adenocarcinoma.
- Serous carcinoma of the endometrium - esp. if high-grade nuclear features are present diffusely.
- Clear cell carcinoma of the endometrium - esp. when clear cells present.
Grading
- FIGO system most commonly used.
- Based on gland formation & adjusted by nuclear pleomorphism.
Preliminary grade based on gland formation:[9][10][11][12]
- Grade 1: <5% solid component.
- Grade 2: 5-50% solid component.
- Grade 3: >50% solid component.
Modifiers/adjustment:
- High grade nuclei upgrades cancer by one; high grade nuclei = increased size, irregular large nucleoli, irregular chromatin pattern (clumped, coarse).[13]
Images
www:
IHC
- Vimentin +ve.
- ER +ve.
- PR +ve.
Others:
- p16 -ve -- positive in serous endometrial carcinoma[14] and endocervical adenocarcinoma.
- CEA -ve.
Sign out
ENDOMETRIUM, BIOPSY: - ENDOMETRIOID ENDOMETRIAL ADENOCARCINOMA, FIGO GRADE I/III.
Micro
The sections show endometrium with complex, fused and cribriform glands with scant intervening stroma over a region measuring greater than 2.1 millimetres. Focally, a desmoplastic stroma is also identified. No nuclear atypia is appreciated.
Endocervical versus endometrial - biopsy
The foamy histiocytes in the stroma and lack of desmoplasia slightly favour an endometrial origin; however, the lesion would be best classified with an excisional specimen and in conjunction with the clinical impression.
See also
References
- ↑ Lax, SF. (Jan 2002). "[Dualistic model of molecular pathogenesis in endometrial carcinoma].". Zentralbl Gynakol 124 (1): 10-6. doi:10.1055/s-2002-20303. PMID 11873308.
- ↑ Karamurzin, Y.; Soslow, RA.; Garg, K. (Apr 2013). "Histologic evaluation of prophylactic hysterectomy and oophorectomy in Lynch syndrome.". Am J Surg Pathol 37 (4): 579-85. doi:10.1097/PAS.0b013e3182796e27. PMID 23426126.
- ↑ Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 239. ISBN 978-0443069208.
- ↑ 4.0 4.1 Kurman, RJ.; Norris, HJ. (Jun 1982). "Evaluation of criteria for distinguishing atypical endometrial hyperplasia from well-differentiated carcinoma.". Cancer 49 (12): 2547-59. PMID 7074572.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Endometrium_11protocol.pdf. Accessed on: 12 January 2012.
- ↑ URL: http://dictionary.reference.com/browse/dyskeratosis. Accessed on: 5 September 2011.
- ↑ Miranda, MC.; Mazur, MT. (May 1995). "Endometrial squamous metaplasia. An unusual response to progestin therapy of hyperplasia.". Arch Pathol Lab Med 119 (5): 458-60. PMID 7748076.
- ↑ Chinen, K.; Kamiyama, K.; Kinjo, T.; Arasaki, A.; Ihama, Y.; Hamada, T.; Iwamasa, T. (Sep 2004). "Morules in endometrial carcinoma and benign endometrial lesions differ from squamous differentiation tissue and are not infected with human papillomavirus.". J Clin Pathol 57 (9): 918-26. doi:10.1136/jcp.2004.017996. PMID 15333650.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1087-8. ISBN 0-7216-0187-1.
- ↑ URL: http://www.pathologyoutlines.com/uterus.html#endometrialcarc.
- ↑ URL: http://www.emedicine.com/med/topic2832.htm.
- ↑ Ayhan A, Taskiran C, Yuce K, Kucukali T (January 2003). "The prognostic value of nuclear grading and the revised FIGO grading of endometrial adenocarcinoma". Int. J. Gynecol. Pathol. 22 (1): 71–4. PMID 12496701.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 240. ISBN 978-0470519035.
- ↑ Chiesa-Vottero, AG.; Malpica, A.; Deavers, MT.; Broaddus, R.; Nuovo, GJ.; Silva, EG. (Jul 2007). "Immunohistochemical overexpression of p16 and p53 in uterine serous carcinoma and ovarian high-grade serous carcinoma.". Int J Gynecol Pathol 26 (3): 328-33. doi:10.1097/01.pgp.0000235065.31301.3e. PMID 17581420.