ELOC-mutated renal cell carcinoma
| ELOC-mutated renal cell carcinoma | |
|---|---|
| Diagnosis in short | |
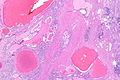
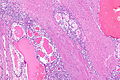
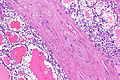
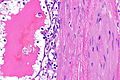
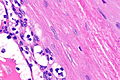
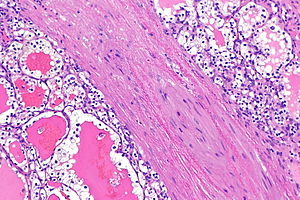 RCC with clear cells and fibromuscular band - morphology compatible with TCEB1 mutation. H&E stain. (WC) | |
|
| |
| Synonyms | TCEB1-mutated renal cell carcinoma (old name) |
|
| |
| LM | clear cells with abundant cytoplasm and basal nuclei (may have luminal nuclei), usually ISUP nucleolar grade 2, fibromuscular bands |
| LM DDx | clear cell renal cell carcinoma, clear cell papillary renal cell tumour (clear cell papillary RCC), renal cell carcinoma with fibromyomatous stroma |
| IHC | CK7 +ve, CD10 +ve, CK34betaE12 -ve |
| Molecular | TCEB1 mutation |
| Site | kidney - see kidney tumours |
|
| |
| Syndromes | possibly tuberous sclerosis - see tuberous sclerosis-associated renal cell carcinoma |
|
| |
| Prevalence | very rare - evolving entity |
| Prognosis | good - based on limited data |
ELOC-mutated renal cell carcinoma is a type of renal cell carcinoma that is morphologically similar to clear cell renal cell carcinoma and clear cell papillary renal cell tumour (previously clear cell papillary renal cell carcinoma).[1] It was formally recognized in the WHO 2022 classification of renal neoplasia.[citation needed]
It was previously known as TCEB1-mutated renal cell carcinoma and renal cell carcinoma with TCEB1 mutation. It should not be confused with TFEB renal cell carcinoma, also known as renal tumour with t(6;11) translocation.
It is unrelated to the previously described renal angiomyoadenomatous tumour[1][2] that was lumped with clear cell papillary renal cell carcinoma in the Vancouver modification of the WHO classification.
General
- Evolving entity.
- TCEB1 (transcription elongation factor B, polypeptide 1) is part of a complex that binds with the product of the VHL gene;[3] thus, it acts as a tumour suppressor.
- Good prognosis - based on limited data.[1]
Gross
- Cystic changes.
Microscopic
Features:
- Clear cells with abundant cytoplasm and basal nuclei.
- Luminal nuclei (like in clear cell tubulopapillary RCC) may be seen.
- Usually ISUP nucleolar grade 2.
- Fibromuscular bands - key feature.
DDx:
- Clear cell renal cell carcinoma.
- Clear cell papillary renal cell tumour (previously clear cell papillary renal cell carcinoma) - have luminal nuclei.
- Tuberous sclerosis-associated renal cell carcinoma.
- Renal cell carcinoma with fibromyomatous stroma has TSC/mTOR pathway mutation.
Images
Morphology compatible
IHC
Features:[1]
- CK7 +ve.
- CD10 +ve.
- Typically negative in clear cell papillary renal cell tumour.
- CK34betaE12 -ve.
- Usually positive in clear cell papillary renal cell tumour.
Others:
- GPNMB -ve.
- TSC1/TSC2/MTOR mutated RCC is GPNMB +ve.[4]
Comparison between some renal tumours with clear cells
| Tumour | CK7 | CD10 | CK34betaE12 (K903) | GPNMB |
|---|---|---|---|---|
| Clear cell renal cell carcinoma | -ve (may be focal) | +ve | -ve | usu. -ve |
| Clear cell papillary renal cell tumour | +ve (diffuse) | -ve | +ve | -ve[4] |
| ELOC-mutated renal cell carcinoma | +ve | +ve | -ve | -ve |
| TSC/mTOR-mutated renal cell carcinoma with fibromyomatous stroma | +ve | +ve | -ve | +ve |
Sign out
Molecular lacking
Right Kidney, Radical Nephrectomy:
- RENAL CELL CARCINOMA with clear cells, cysts and leiomyomatous stroma, see comment.
-- Margin clear.
-- Please see synoptic report for details.
Comment:
The tumour stains as follows:
POSITIVE: CD10 (moderate), EMA (patchy), CAM5.2, CK7 (focal), PAX8 (diffuse).
NEGATIVE: CK34betaE12, CK20.
The differential diagnosis includes: (1) clear cell renal cell carcinoma, (2) RCC with a mTOR pathway mutation, and (3) ELOC-mutated RCC.
See also
- Vancouver classification.
- Renal angiomyoadenomatous tumour (renal cell carcinoma with angioleiomyoma-like stroma).
- Renal cell carcinoma with fibromyomatous stroma.
References
- ↑ 1.0 1.1 1.2 1.3 Hakimi, AA.; Tickoo, SK.; Jacobsen, A.; Sarungbam, J.; Sfakianos, JP.; Sato, Y.; Morikawa, T.; Kume, H. et al. (Jun 2015). "TCEB1-mutated renal cell carcinoma: a distinct genomic and morphological subtype.". Mod Pathol 28 (6): 845-53. doi:10.1038/modpathol.2015.6. PMID 25676555.
- ↑ Michal, M.; Hes, O.; Kuroda, N.; Kazakov, DV.; Hora, M. (Jun 2009). "Difference between RAT and clear cell papillary renal cell carcinoma/clear renal cell carcinoma.". Virchows Arch 454 (6): 719. doi:10.1007/s00428-009-0788-9. PMID 19471960.
- ↑ URL: http://www.omim.org/entry/600788. Accessed on: 12 June 2015.
- ↑ 4.0 4.1 Li H, Argani P, Halper-Stromberg E, Lotan TL, Merino MJ, Reuter VE, Matoso A (November 2023). "Positive GPNMB Immunostaining Differentiates Renal Cell Carcinoma With Fibromyomatous Stroma Associated With TSC1/2/MTOR Alterations From Others". Am J Surg Pathol 47 (11): 1267–1273. doi:10.1097/PAS.0000000000002117. PMID 37661807.