Difference between revisions of "Columnar dysplasia of the esophagus"
Jump to navigation
Jump to search
(redirect) |
m (touch) |
||
| (8 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = High-grade_columnar_dysplasia_of_the_esophagus_-_alt_--_intermed_mag.jpg | |||
| Width = | |||
| Caption = High-grade columnar dysplasia of the esophagus. [[H&E stain]]. | |||
| Synonyms = columnar dysplasia, [[esophageal dysplasia]] (nonspecific term) | |||
| Micro = | |||
| Subtypes = low-grade, high-grade | |||
| LMDDx = [[intestinal metaplasia of the esophagus]], [[esophageal adenocarcinoma]], [[basal crypt dysplasia]] | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[esophagus]] - distal | |||
| Assdx = [[Barrett's esophagus]], [[esophageal adenocarcinoma]], [[GERD]] | |||
| Syndromes = | |||
| Clinicalhx = [[GERD]] | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = uncommon | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = pre-malignant (benign) | |||
| Other = | |||
| ClinDDx = | |||
| Tx = low-grade: followup with biopsy; high-grade: resection (surgery, endoscopic mucosal resection) | |||
}} | |||
'''Columnar dysplasia of the esophagus''' is a pre-malignant lesion the [[esophagus]] associated with [[Barrett's esophagus]]. It is considered the precursor of [[esophageal adenocarcinoma]]. | |||
It is also known as '''esophageal columnar dysplasia''' (abbreviated '''ECD'''),<ref name=pmid21809994>{{Cite journal | last1 = Feng | first1 = W. | last2 = Zhou | first2 = Z. | last3 = Peters | first3 = JH. | last4 = Khoury | first4 = T. | last5 = Zhai | first5 = Q. | last6 = Wei | first6 = Q. | last7 = Truong | first7 = CD. | last8 = Song | first8 = SW. | last9 = Tan | first9 = D. | title = Expression of insulin-like growth factor II mRNA-binding protein 3 in human esophageal adenocarcinoma and its precursor lesions. | journal = Arch Pathol Lab Med | volume = 135 | issue = 8 | pages = 1024-31 | month = Aug | year = 2011 | doi = 10.5858/2009-0617-OAR2 | PMID = 21809994 }}</ref> | |||
'''dysplasia in the columnar-lined esophagus''',<ref>{{Cite journal | last1 = Levine | first1 = DS. | title = Management of dysplasia in the columnar-lined esophagus. | journal = Gastroenterol Clin North Am | volume = 26 | issue = 3 | pages = 613-34 | month = Sep | year = 1997 | doi = | PMID = 9309409 }}</ref> | |||
and '''columnar epithelial dysplasia'''.<ref name=pmid3825997>{{Cite journal | last1 = Hamilton | first1 = SR. | last2 = Smith | first2 = RR. | title = The relationship between columnar epithelial dysplasia and invasive adenocarcinoma arising in Barrett's esophagus. | journal = Am J Clin Pathol | volume = 87 | issue = 3 | pages = 301-12 | month = Mar | year = 1987 | doi = | PMID = 3825997 }}</ref> | |||
==General== | |||
*Arises in the setting of ''[[Barrett esophagus]]''. | |||
*Precursor of [[esophageal adenocarcinoma]]. | |||
===Classification=== | |||
#Indefinite for dysplasia. | |||
#*[[Diagnosis]] used in the context of uncertainty (like ''[[gynecologic cytopathology|ASCUS]]'' and ''[[prostate gland|ASAP]]''); the classic reason for its use is: the surface (epithelium) cannot be seen (which precludes assessment of maturation); may be used in the context of inflammation. | |||
#Low grade dysplasia. | |||
#High grade dysplasia. | |||
===Management=== | |||
Low grade dysplasia & indefinite for dysplasia: | |||
*Follow-up. | |||
High grade dysplasia: | |||
*[[Endoscopic mucosal resection]] (EMR).<ref name=pmid19306943>{{cite journal |author=Sampliner RE |title=Endoscopic Therapy for Barrett's Esophagus |journal=Clin. Gastroenterol. Hepatol. |volume= |issue= |pages= |year=2009 |month=March |pmid=19306943 |doi=10.1016/j.cgh.2009.03.011 |url=}}</ref> | |||
*Surgical resection (esophagectomy). | |||
==Microscopic== | |||
Features to assess:<ref name=Ref_GLP46>{{Ref GLP|46}}</ref> | |||
# Lack of surface maturation - very common, occasionally absent.<ref name=pmid16625087>{{Cite journal | last1 = Lomo | first1 = LC. | last2 = Blount | first2 = PL. | last3 = Sanchez | first3 = CA. | last4 = Li | first4 = X. | last5 = Galipeau | first5 = PC. | last6 = Cowan | first6 = DS. | last7 = Ayub | first7 = K. | last8 = Rabinovitch | first8 = PS. | last9 = Reid | first9 = BJ. | title = Crypt dysplasia with surface maturation: a clinical, pathologic, and molecular study of a Barrett's esophagus cohort. | journal = Am J Surg Pathol | volume = 30 | issue = 4 | pages = 423-35 | month = Apr | year = 2006 | doi = | PMID = 16625087 }}</ref> | |||
#*Lack of lighter staining at surface. | |||
#*Nuclear crowding at surface. | |||
#*Nuclei at the surface not smaller. | |||
# Architecture - esp. at low power. | |||
#* Glands not round. | |||
#** Low-grade feature: gland budding. | |||
#** High-grade features: cribriforming, cystic dilation, necrotic debris. | |||
#* Gland density: | |||
#** Increased & round - think low-grade dysplasia. | |||
#** Increased & irregular - think high-grade dysplasia. | |||
# Cytology, esp. at high magnification. | |||
#* Nuclear abnormalities in: size, staining, shape. | |||
#* Loss of "nuclear polarity" = high-grade feature | |||
#** Loss of palisaded appearance, rounding-up of nuclei. | |||
# Inflammation, erosions & ulceration. | |||
#* Marked inflammation should prompt consideration of knocking down the diagnosis one step, i.e. low-grade becomes indefinite ''or'' high-grade becomes low-grade. | |||
Negatives: | |||
#No desmoplasia. | |||
#*Stromal fibrotic reaction to the tumour. | |||
#**Desmoplasia is rare in the superficial esophagus.<ref name=Ref_GLP49>{{Ref GLP|49}}</ref> | |||
#No single cells. | |||
#No extensive back-to-back glands. | |||
Notes: | |||
*Changes similar to those see in colorectal tubular adenomas; however, what would be low-grade dysplasia in the rectum is high-grade dysplasia in the esophagus. | |||
*Presence of goblet cells suggests it is not dysplasia.<ref>GAG. January 2009.</ref> | |||
*Desmoplasia present = invasive adenocarcinoma.<ref name=Ref_GLP54>{{Ref GLP|54}}</ref> | |||
*Some literature suggests community pathologists should ''not'' make this call, i.e. it should be diagnosed by an expert.<ref name=pmid10385717>{{Cite journal | last1 = Alikhan | first1 = M. | last2 = Rex | first2 = D. | last3 = Khan | first3 = A. | last4 = Rahmani | first4 = E. | last5 = Cummings | first5 = O. | last6 = Ulbright | first6 = TM. | title = Variable pathologic interpretation of columnar lined esophagus by general pathologists in community practice. | journal = Gastrointest Endosc | volume = 50 | issue = 1 | pages = 23-6 | month = Jul | year = 1999 | doi = | PMID = 10385717 }}</ref> | |||
DDx: | |||
*[[Intestinal metaplasia of the esophagus]]. | |||
*[[Esophageal adenocarcinoma]]. | |||
===Images=== | |||
No dysplasia - only intestinal metaplasia: | |||
*[http://www.nature.com/nrgastro/journal/v6/n8/fig_tab/nrgastro.2009.103_F4.html Intestinal metaplasia (nature.com)]. | |||
====Indefinite for columnar dysplasia==== | |||
www: | |||
*[http://www.nature.com/nrgastro/journal/v6/n8/fig_tab/nrgastro.2009.103_F8.html Indefinite for columnar dysplasia (nature.com)]. | |||
*[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1861756/figure/fig6/ Indefinite for columnar dysplasia (nih.gov)].<ref name=pmid17021130/> | |||
====Low-grade columnar dysplasia==== | |||
<gallery> | |||
Image: Low-grade columnar dysplasia of the esophagus -- low mag.jpg | LGD - low mag. (WC) | |||
Image: Low-grade columnar dysplasia of the esophagus -- intermed mag.jpg | LGD - intermed. mag. (WC) | |||
Image: Low-grade columnar dysplasia of the esophagus -- high mag.jpg | LGD - high mag. (WC) | |||
Image: Low-grade columnar dysplasia of the esophagus -- very high mag.jpg | LGD - very high mag. (WC) | |||
</gallery> | |||
www: | |||
*[http://www.nature.com/nrgastro/journal/v6/n8/fig_tab/nrgastro.2009.103_F5.html Low-grade columnar dysplasia (nature.com)].<ref name=pmid19581906>{{Cite journal | last1 = Odze | first1 = RD. | title = Barrett esophagus: histology and pathology for the clinician. | journal = Nat Rev Gastroenterol Hepatol | volume = 6 | issue = 8 | pages = 478-90 | month = Aug | year = 2009 | doi = 10.1038/nrgastro.2009.103 | PMID = 19581906 }}</ref> | |||
*[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1861756/figure/fig2/ Low-grade columnar dysplasia (nih.gov)].<ref name=pmid17021130>{{Cite journal | last1 = Odze | first1 = RD. | title = Diagnosis and grading of dysplasia in Barrett's oesophagus. | journal = J Clin Pathol | volume = 59 | issue = 10 | pages = 1029-38 | month = Oct | year = 2006 | doi = 10.1136/jcp.2005.035337 | PMID = 17021130 }}</ref> | |||
====High-grade columnar dysplasia==== | |||
<gallery> | |||
Image: High-grade columnar dysplasia of the esophagus -- low mag.jpg | HGD - low mag. | |||
Image: High-grade columnar dysplasia of the esophagus -- intermed mag.jpg | HGD - intermed. mag. | |||
Image: High-grade columnar dysplasia of the esophagus - alt -- intermed mag.jpg | HGD - intermed. mag. | |||
Image: High-grade columnar dysplasia of the esophagus -- high mag.jpg | HGD - high mag. | |||
</gallery> | |||
www: | |||
*[http://www.nature.com/nrgastro/journal/v6/n8/fig_tab/nrgastro.2009.103_F6.html High-grade columnar dysplasia (nature.com)].<ref name=pmid19581906/> | |||
*[http://www.nature.com/ajg/journal/v104/n10/fig_tab/ajg2009390f3.html High-grade columnar dysplasia (nature.com)].<ref name=pmid19623166>{{Cite journal | last1 = Riddell | first1 = RH. | last2 = Odze | first2 = RD. | title = Definition of Barrett's esophagus: time for a rethink--is intestinal metaplasia dead? | journal = Am J Gastroenterol | volume = 104 | issue = 10 | pages = 2588-94 | month = Oct | year = 2009 | doi = 10.1038/ajg.2009.390 | PMID = 19623166 }}</ref> | |||
*[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1861756/figure/fig3/ High-grade columnar dysplasia (nih.gov)].<ref name=pmid17021130/> | |||
==Sign out== | |||
<pre> | |||
ESOPHAGUS, DISTAL, BIOPSY: | |||
- LOW-GRADE COLUMNAR EPITHELIAL DYSPLASIA, SEE COMMENT. | |||
- COLUMNAR EPITHELIUM WITH GOBLET CELL METAPLASIA. | |||
- REACTIVE SQUAMOUS EPITHELIUM. | |||
COMMENT: | |||
This was reviewed with Dr. X and they agree with the diagnosis. | |||
</pre> | |||
====Alternate==== | |||
<pre> | |||
ESOPHAGUS, 30 CM, BIOPSY: | |||
- LOW-GRADE COLUMNAR DYSPLASIA WITH INTESTINAL METAPLASIA AND MILD CHRONIC | |||
INFLAMMATION. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
==See also== | |||
*[[Esophagus]]. | |||
*[[Esophageal adenocarcinoma]]. | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Esophagus]] | |||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
Latest revision as of 06:25, 14 January 2015
| Columnar dysplasia of the esophagus | |
|---|---|
| Diagnosis in short | |
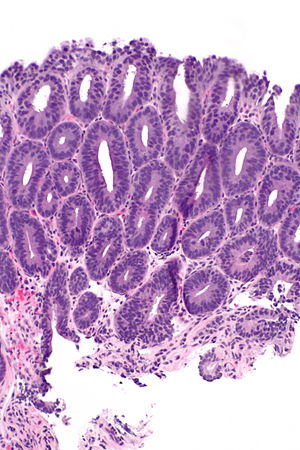 High-grade columnar dysplasia of the esophagus. H&E stain. | |
|
| |
| Synonyms | columnar dysplasia, esophageal dysplasia (nonspecific term) |
| Subtypes | low-grade, high-grade |
| LM DDx | intestinal metaplasia of the esophagus, esophageal adenocarcinoma, basal crypt dysplasia |
| Site | esophagus - distal |
|
| |
| Associated Dx | Barrett's esophagus, esophageal adenocarcinoma, GERD |
| Clinical history | GERD |
| Prevalence | uncommon |
| Prognosis | pre-malignant (benign) |
| Treatment | low-grade: followup with biopsy; high-grade: resection (surgery, endoscopic mucosal resection) |
Columnar dysplasia of the esophagus is a pre-malignant lesion the esophagus associated with Barrett's esophagus. It is considered the precursor of esophageal adenocarcinoma.
It is also known as esophageal columnar dysplasia (abbreviated ECD),[1] dysplasia in the columnar-lined esophagus,[2] and columnar epithelial dysplasia.[3]
General
- Arises in the setting of Barrett esophagus.
- Precursor of esophageal adenocarcinoma.
Classification
- Indefinite for dysplasia.
- Low grade dysplasia.
- High grade dysplasia.
Management
Low grade dysplasia & indefinite for dysplasia:
- Follow-up.
High grade dysplasia:
- Endoscopic mucosal resection (EMR).[4]
- Surgical resection (esophagectomy).
Microscopic
Features to assess:[5]
- Lack of surface maturation - very common, occasionally absent.[6]
- Lack of lighter staining at surface.
- Nuclear crowding at surface.
- Nuclei at the surface not smaller.
- Architecture - esp. at low power.
- Glands not round.
- Low-grade feature: gland budding.
- High-grade features: cribriforming, cystic dilation, necrotic debris.
- Gland density:
- Increased & round - think low-grade dysplasia.
- Increased & irregular - think high-grade dysplasia.
- Glands not round.
- Cytology, esp. at high magnification.
- Nuclear abnormalities in: size, staining, shape.
- Loss of "nuclear polarity" = high-grade feature
- Loss of palisaded appearance, rounding-up of nuclei.
- Inflammation, erosions & ulceration.
- Marked inflammation should prompt consideration of knocking down the diagnosis one step, i.e. low-grade becomes indefinite or high-grade becomes low-grade.
Negatives:
- No desmoplasia.
- Stromal fibrotic reaction to the tumour.
- Desmoplasia is rare in the superficial esophagus.[7]
- Stromal fibrotic reaction to the tumour.
- No single cells.
- No extensive back-to-back glands.
Notes:
- Changes similar to those see in colorectal tubular adenomas; however, what would be low-grade dysplasia in the rectum is high-grade dysplasia in the esophagus.
- Presence of goblet cells suggests it is not dysplasia.[8]
- Desmoplasia present = invasive adenocarcinoma.[9]
- Some literature suggests community pathologists should not make this call, i.e. it should be diagnosed by an expert.[10]
DDx:
Images
No dysplasia - only intestinal metaplasia:
Indefinite for columnar dysplasia
www:
Low-grade columnar dysplasia
www:
High-grade columnar dysplasia
www:
- High-grade columnar dysplasia (nature.com).[12]
- High-grade columnar dysplasia (nature.com).[13]
- High-grade columnar dysplasia (nih.gov).[11]
Sign out
ESOPHAGUS, DISTAL, BIOPSY: - LOW-GRADE COLUMNAR EPITHELIAL DYSPLASIA, SEE COMMENT. - COLUMNAR EPITHELIUM WITH GOBLET CELL METAPLASIA. - REACTIVE SQUAMOUS EPITHELIUM. COMMENT: This was reviewed with Dr. X and they agree with the diagnosis.
Alternate
ESOPHAGUS, 30 CM, BIOPSY: - LOW-GRADE COLUMNAR DYSPLASIA WITH INTESTINAL METAPLASIA AND MILD CHRONIC INFLAMMATION. - NEGATIVE FOR MALIGNANCY.
See also
References
- ↑ Feng, W.; Zhou, Z.; Peters, JH.; Khoury, T.; Zhai, Q.; Wei, Q.; Truong, CD.; Song, SW. et al. (Aug 2011). "Expression of insulin-like growth factor II mRNA-binding protein 3 in human esophageal adenocarcinoma and its precursor lesions.". Arch Pathol Lab Med 135 (8): 1024-31. doi:10.5858/2009-0617-OAR2. PMID 21809994.
- ↑ Levine, DS. (Sep 1997). "Management of dysplasia in the columnar-lined esophagus.". Gastroenterol Clin North Am 26 (3): 613-34. PMID 9309409.
- ↑ Hamilton, SR.; Smith, RR. (Mar 1987). "The relationship between columnar epithelial dysplasia and invasive adenocarcinoma arising in Barrett's esophagus.". Am J Clin Pathol 87 (3): 301-12. PMID 3825997.
- ↑ Sampliner RE (March 2009). "Endoscopic Therapy for Barrett's Esophagus". Clin. Gastroenterol. Hepatol.. doi:10.1016/j.cgh.2009.03.011. PMID 19306943.
- ↑ Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 46. ISBN 978-0443066573.
- ↑ Lomo, LC.; Blount, PL.; Sanchez, CA.; Li, X.; Galipeau, PC.; Cowan, DS.; Ayub, K.; Rabinovitch, PS. et al. (Apr 2006). "Crypt dysplasia with surface maturation: a clinical, pathologic, and molecular study of a Barrett's esophagus cohort.". Am J Surg Pathol 30 (4): 423-35. PMID 16625087.
- ↑ Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 49. ISBN 978-0443066573.
- ↑ GAG. January 2009.
- ↑ Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 54. ISBN 978-0443066573.
- ↑ Alikhan, M.; Rex, D.; Khan, A.; Rahmani, E.; Cummings, O.; Ulbright, TM. (Jul 1999). "Variable pathologic interpretation of columnar lined esophagus by general pathologists in community practice.". Gastrointest Endosc 50 (1): 23-6. PMID 10385717.
- ↑ 11.0 11.1 11.2 Odze, RD. (Oct 2006). "Diagnosis and grading of dysplasia in Barrett's oesophagus.". J Clin Pathol 59 (10): 1029-38. doi:10.1136/jcp.2005.035337. PMID 17021130.
- ↑ 12.0 12.1 Odze, RD. (Aug 2009). "Barrett esophagus: histology and pathology for the clinician.". Nat Rev Gastroenterol Hepatol 6 (8): 478-90. doi:10.1038/nrgastro.2009.103. PMID 19581906.
- ↑ Riddell, RH.; Odze, RD. (Oct 2009). "Definition of Barrett's esophagus: time for a rethink--is intestinal metaplasia dead?". Am J Gastroenterol 104 (10): 2588-94. doi:10.1038/ajg.2009.390. PMID 19623166.