CSF cytopathology
Revision as of 06:44, 7 May 2015 by Jensflorian (talk | contribs) (meningeosis neoplastica restructured)
CSF cytopathology is a subset of CNS cytopathology, which is a subset of cytopathology.
This article deal only with cerebrospinal fluid (CSF) cytopathology. An introduction to cytopathology is in the cytopathology article.
In many institutions, CSF specimens get triaged/rapidly assessed as:
- They are small specimens ~ usually 1-10 ml.
- The procedure to obtain them is non-trivial, i.e. not pleasant for the patient and not risk free.
- Lymphoma is a common malignancy of malignancies found in the CSF.
In many institutions, all CSF specimens are stat.
Cerebrospinal fluid
Normal
- Paucicellular.
- <12/3 cells
Gobs of anuclear material:
- Protein vs. white mater.
Bark-like flaky material:
- Contaminant.
Fluffy/smudged large cells (~2-3x RBC dia.) with an indistinct nucleus:
- Degenerated white cells.
- Should prompt a comment about "degeneration", if the population is dominant.
Routine processing
- Cytospin - if no abnormality at triage.
- The cellularity of the cytospin will appear to be increased (artifact).
Images
Hemorrhage
- Xanthochromatous specimen
- Can be artificial -> due punctuation.
Cytology
- Mostly RBC.
- Neutrophils can be increased.
- +/-Erythro- and Siderophages (usu. after 3-4d).
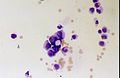
Acute bacterial meningitis
Main article: Meningitis
Cytology
- Neutrophils - none should be present normally.[1][2]
- If the tap is traumatic (i.e. fibrin is present) the finding may be uninterpretable.
- Neutrophils may be present in early exsudative phase of viral meningitis.
- Cell count usually above 1000/µl.
Viral meningitis
Main article: Meningitis
General
- Positive viral culture.
Cytology
- Polymorphous population of lymphocytes.[1]
Mollaret's meningitis
General
- Rare aseptic meningitis.
- Suspected to be caused by HSV1 and HSV2.[3]
Clinical:
- Recurrent meningismus, headache, +/-fever.[3]
Cytology
Features:
- Mollaret cells - described as monocytoid cells[1] (look like monocytes[4] - but do not phagocytose), and large endothelial cells.[3]
- Features - large cells with: abundant cytoplasm, footprint-shaped" nucleus.
- Mollaret cells not pathognomonic.[3]
- Mixed population of inflammatory cells[1] (PMNs, monocytes, plasma cells, lymphocytes); usually lymphocyte predominant.[3]
Image:
Meningeosis neoplastica
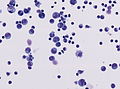
CNS lymphoma
Histology:[1]
- Too many cells - key feature.
- Not diagnostic... but should raise suspicion.
- Single cells (as typical of lymphoma/leukemia).
- Large lymphocytes - >2x RBC diameter.
- +/-Nuclear atypia.
- Radial segmentation - a completely cleaved nucleus/quasi-binucleation.
Notes:
- Massive karyorrhexis (nuclear fragmentation) is suggestive of lymphoma[1] - not common.
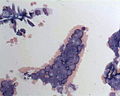
Meningeosis carcinomatosa
Histology:
- abnormal cell size / giant multinuclear cells.
- unusual nuclear/cytoplasm ratio.
- hyperchromatic nuclei.
- prominent nucleoli.
- atypical mitoses.
- cell clustering.
Notes:
- cell count can be normal.
- accompanied by granulocytes and monocytes.
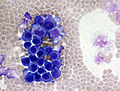
Non-lymphoid, non-epithelial neoplasm
- Non-lymphoid, non-epithelial neoplasms are rarely found in the CSF.
- Ependymomas and medulloblastomas have a higher rate of dissemination than other primary brain tumors.
Meningeosis gliomatosa (Astrocytoma/Glioblastoma):
- May vaguely resemble a neuroendocrine tumour:
- Small cell clusters.
- Nuclear moulding.
- Cells somewhat larger than small cell carcinoma.
- Scant cytoplasm.
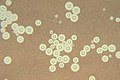
CNS fungal infections
- Cryptococcus is the most common.[5]
Cryptococcosis
Main article: Cryptococcosis
- AKA cryptococcus infection
General
- Usu. immunocompromised host.
Microscopic
Microscopic appearance:
- Yeast:[5]
- Round/ovoid 5-15 micrometres.
- Thick mucopolysacchardie capsule + refractile centre.
- "Target-like" shape/"bull's eye" appearance.
- "Tear drop-shapped" budding pattern (useful to differentiate from Blastomyces, Histoplasma).
Images:
- Cryptococcus in lung FNA - Field stain (WC).
- Crytococcosis - mucicarmine stain (WC).
- Crytococcosis - methenamine silver stain (WC).
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 681 (Q25). ISBN 978-1416025887.
- ↑ MUN. 4 November 2010.
- ↑ 3.0 3.1 3.2 3.3 3.4 http://emedicine.medscape.com/article/1169489-overview
- ↑ http://www.mondofacto.com/facts/dictionary?monocytoid+cell
- ↑ 5.0 5.1 Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 682. ISBN 978-1416025887.