Difference between revisions of "Atrophic endometrium"
(→Images) |
|||
| Line 63: | Line 63: | ||
===Images=== | ===Images=== | ||
<gallery> | <gallery> | ||
Image: Inactive endometrial epithelium -- intermed mag.jpg | Inactive endometrium - intermed. mag. | Image: Inactive endometrial epithelium -- intermed mag.jpg | Inactive endometrium - intermed. mag. (WC) | ||
Image: Inactive endometrial epithelium -- high mag.jpg | Inactive endometrium - high mag. | Image: Inactive endometrial epithelium -- high mag.jpg | Inactive endometrium - high mag. (WC) | ||
</gallery> | |||
<gallery> | |||
Image: Nonproliferative endometrial epithelium -- intermed mag.jpg | IE - intermed. mag. (WC) | |||
Image: Nonproliferative endometrial epithelium -- high mag.jpg | IE - high mag. (WC) | |||
Image: Nonproliferative endometrial epithelium - alt -- high mag.jpg | IE - high mag. (WC) | |||
Image: Nonproliferative endometrial epithelium - alt 2 -- high mag.jpg | IE - high mag. (WC) | |||
Image: Nonproliferative endometrial epithelium -- very high mag.jpg | IE - very high mag. (WC) | |||
</gallery> | </gallery> | ||
www: | www: | ||
Revision as of 00:38, 20 December 2013
| Atrophic endometrium | |
|---|---|
| Diagnosis in short | |
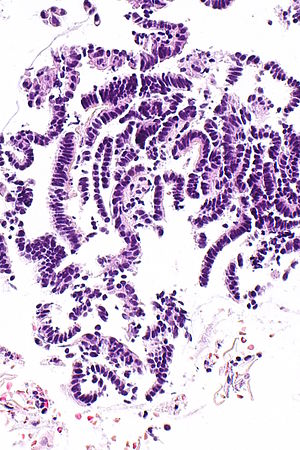 Inactive endometrial epithelium. H&E stain. | |
|
| |
| LM | nonproliferative endometrial epithelium, +/-benign stroma with normal gland-to-stroma ratio, no nuclear atypia |
| LM DDx | type 2 endometrial carcinomas, esp. serous endometrial carcinoma, proliferative phase endometrium |
| Site | endometrium |
|
| |
| Clinical history | postmenopausal |
| Other | normal postmenopausal finding |
| Clin. DDx | atrophy, endometrial hyperplasia, endometrial carcinoma, other gynecologic cancers |
Atrophic endometrium, also inactive endometrium, is the normal finding in postmenopausal women.
It is also known as atrophy of the endometrium and endometrial atrophy.
An introduction to the endometrium is found in the endometrium article.
General
- Endometrium of normal postmenopausal women.
- Menopause typically happens at around 50 years old.
- Very common diagnosis.
- Atrophy may be associated with bleeding and therefore biopsied to rule-out hyperplasia and malignancy.
Gross
- Thin endometrium.
Microscopic
Features:
- Glands - small columnar cells:
- Moderate quantity of eosinophilic cytoplasm.
- Ovoid (palisaded) nuclei +/- nuclear pseudostratification.[1]
- Eosinophilic cytoplasm.
- No mitoses.
- Architecture:
- +/-Cystic dilation.
Notes:
- If a woman is truly postmenopausal, mitoses in the glandular epithelium is pathologic until demonstrated otherwise.
- The exceptions are benign endometrial polyp, uterine prolapse, and possibly inflammation (e.g. the person has had several biopsy attempts and was seeded with pathogens).
DDx:
- Proliferative phase endometrium - esp. if there is pseudostratification.
- Serous carcinoma of the endometrium.
Images
www:
Sign out
ENDOMETRIUM, BIOPSY: - NON-PROLIFERATIVE ENDOMETRIUM. - BENIGN SQUAMOUS EPITHELIUM WITH METAPLASTIC CHANGE. - SCANT ENDOCERVICAL MUCOSA WITH REACTIVE CHANGES.
ENDOMETRIUM, BIOPSY: - NON-PROLIFERATIVE ENDOMETRIUM. - BENIGN STRIPPED ENDOCERVICAL EPITHELIUM. - NEGATIVE FOR HYPERPLASIA AND NEGATIVE FOR MALIGNANCY.
Micro
The sections show small fragments of endometrium. The gland-to-stroma ratio is normal. The glands are small and round, and have a pseudostratified epithelium.
Mitotic figures are not identified within the glands or stroma. No stromal condensation is apparent. No secretions are in the glands. No nuclear atypia is apparent.
Scant benign endocervical tissue (stripped epithelium and mucosa) is present.
Limited stroma
ENDOMETRIUM, BIOPSY: - STRIPPED NONPROLIFERATIVE ENDOMETRIAL EPITHELIUM; NO APPRECIABLE STROMA PRESENT. - SCANT ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS. - MINUTE FRAGMENTS OF SQUAMOUS EPITHELIUM WITHOUT APPARENT PATHOLOGY.
ENDOMETRIUM, BIOPSY: - SCANT STRIPPED NON-PROLIFERATIVE ENDOMETRIAL EPITHELIUM. - VERY SMALL FRAGMENT OF ENDOMETRIAL STROMA. - TUBAL METAPLASTIC EPITHELIUM.
ENDOMETRIUM, ASPIRATION: - SMALL FRAGMENTS OF NONPROLIFERATIVE ENDOMETRIAL EPITHELIUM ATTACHED TO A VERY SMALL AMOUNT OF STROMA. - MINUTE BENIGN FRAGMENT OF SQUAMOUS EPITHELIUM. - MUCOUS AND INFLAMMATORY CELLS. COMMENT: The sample is scant given the history of 'thickened endometrium'.
Micro
The sections show stripped endometrial epithelium and stripped tubal-type epithelium. No mitotic activity is identified. No nuclear atypia is apparent. A small fragment of definite endometrial stroma is present. The gland-to-stroma ratio cannot be assessed due to the limited stroma.
See also
References
- ↑ 1.0 1.1 McCluggage, WG. (Aug 2006). "My approach to the interpretation of endometrial biopsies and curettings.". J Clin Pathol 59 (8): 801-12. doi:10.1136/jcp.2005.029702. PMC 1860448. PMID 16873562. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1860448/. Cite error: Invalid
<ref>tag; name "pmid16873562" defined multiple times with different content