Difference between revisions of "Adrenal cortical adenoma"
Jump to navigation
Jump to search
(tweak) |
|||
| Line 90: | Line 90: | ||
==References== | ==References== | ||
{{ | {{Reflist|2}} | ||
[[Category:Adrenal gland]] | [[Category:Adrenal gland]] | ||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
Revision as of 06:01, 9 May 2015
| Adrenal cortical adenoma | |
|---|---|
| Diagnosis in short | |
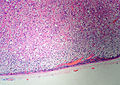
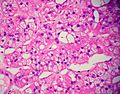
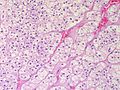
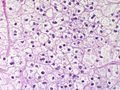
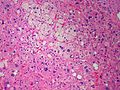
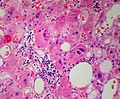
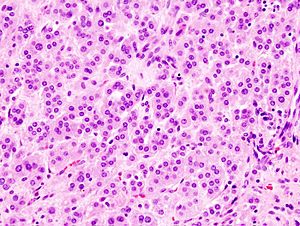 Adrenal cortical adenoma. H&E stain. | |
| LM DDx | adrenal cortical nodule, adrenal cortical hyperplasia, adrenal cortical carcinoma |
| Site | adrenal gland |
|
| |
| Prevalence | relatively common |
| Radiology | adrenal mass, HU<10 |
| Prognosis | benign |
Adrenal cortical adenoma, also adrenocortical adenoma and adrenal adenoma, is a relatively common benign pathology of the adrenal gland.
General
Epidemiology:
- Often an incidental finding.
Pathologic/clinical:
- May be hormonally active.
- Can be a cause of hypertension.[1]
- Radiologists are good at identifying adenomas, as they are usually lipid rich and have a characteristic low HU signal (<10 HU[2]).
Indications for excision:[4][5]
- Lesions >30 mm.
- Hormonally active.
- Non-incidental finding. (???)
- Adrenal vein sampling (AVS) suggestive of adenoma.[1]
Notes:
- Cushing disease is due to the ACTH over-production by the pituitary.
- In cortisol producing tumours (Cushing syndrome): atrophy of the non-hyperplastic cortex (due to feedback inhibition from the pituitary gland).
Microscopic
Classic features:
- Well-defined cell borders.
- Clear cells (abundant, finely vacuolated cytoplasm)
- Polygonal pink cells.
- Most of the nuclei are bland, central and round.
- May have foci of necrosis/degeneration and nuclear atypia.
Note:
- In aldosterone producing tumours:
- May extend outside of the capsule (should not be diagnosed as adrenal cortical carcinoma).
- No atrophy of non-hyperplastic cortex.
- May show spironolactone bodies if hypertension treated with spironolactone prior to surgery.
DDx:
- Adrenal cortical nodule.[6]
- Adrenal cortical hyperplasia.
- Hyperplasia is multifocal.[7]
- Adrenal cortical carcinoma.
Images
See also
References
- ↑ 1.0 1.1 1.2 Myint, KS.; Watts, M.; Appleton, DS.; Lomas, DJ.; Jamieson, N.; Taylor, KP.; Coghill, S.; Brown, MJ. (Jun 2008). "Primary hyperaldosteronism due to adrenal microadenoma: a curable cause of refractory hypertension.". J Renin Angiotensin Aldosterone Syst 9 (2): 103-6. doi:10.3317/jraas.2008.015. PMID 18584586.
- ↑ Tenenbaum, F.; Lataud, M.; Groussin, L. (Apr 2014). "[Update in adrenal imaging].". Presse Med 43 (4 Pt 1): 410-9. doi:10.1016/j.lpm.2014.02.002. PMID 24636681.
- ↑ Fujiwara, M.; Murao, K.; Imachi, H.; Yoshida, K.; Muraoka, T.; Ohyama, T.; Kushida, Y.; Haba, R. et al. (Oct 2010). "Misdiagnosis of two cases of primary aldosteronism owing to failure of computed tomography to detect adrenal microadenoma.". Am J Med Sci 340 (4): 335-7. doi:10.1097/MAJ.0b013e3181e95587. PMID 20881759.
- ↑ Luton, JP.; Martinez, M.; Coste, J.; Bertherat, J. (Jul 2000). "Outcome in patients with adrenal incidentaloma selected for surgery: an analysis of 88 cases investigated in a single clinical center.". Eur J Endocrinol 143 (1): 111-7. PMID 10870039.
- ↑ Liu, XK.; Liu, XJ.; Dong, X.; Kong, CZ. (Jun 2008). "[Clinical research about treatment for adrenal incidentalomas]". Zhonghua Wai Ke Za Zhi 46 (11): 832-4. PMID 19035218.
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 200. ISBN 978-0443066856.
- ↑ IAV. 18 February 2009.