Adenosarcoma of the uterus
Jump to navigation
Jump to search
| Adenosarcoma of the uterus | |
|---|---|
| Diagnosis in short | |
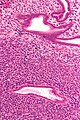
 Uterine adenosarcoma. H&E stain. | |
|
| |
| LM | "Malignant stroma" (stromal with nuclear pleomorphism - typically low grade), benign glands with an abnormal shape and "cambium layer" (increased cellularity around the epithelial elements) |
| LM DDx | benign endometrial polyp, uterine adenofibroma, endometrial stromal sarcoma |
| IHC | CD10 +ve, ER +ve, PR +ve |
| Site | uterus - see uterine tumours |
|
| |
| Clinical history | large age range |
| Signs | vaginal bleeding, mass lesion |
| Prevalence | uncommon |
| Clin. DDx | other causes of AUB |
| Treatment | TAH-BSO |
Adenosarcoma of the uterus is an uncommon tumour that arises from the uterus with benign glands and malignant mesenchymal elements.
General
Features:[1]
- Uncommon.
- May prolapse through cervical os and thus present as cervical polyp.
- Most commonly uterine corpus, occasionally cervix and ovary, rarely in the vagina, fallopian tube, peritoneal surfaces, intestine.
- Large age range<name=pmid9625851/> - may be premenopausal or postmenopausal.
Clinical:[2]
- Most common presentations of Müllerian adenosarcoma (percentages based on series of 41 individuals[3]):
- Vaginal bleeding ~ 70%.
- Pelvic mass ~ 40%.
- Uterine polyp ~ 30%.
- Prognosis (based on series of ~500 individuals[4]):
- Favourable outcome - most detected at an early stage.
- ~80% five year survival for stage I tumours.
- Outcome better than carcinosarcoma.
- Favourable outcome - most detected at an early stage.
Treatment:
- TAH-BSO.
- Tumours are estrogen responsive.
- Chemotherapy (platin-based).[3]
Microscopic
- "Malignant stroma" - key feature.
- Benign glands with an abnormal shape.
- "Cambium layer" = increased cellularity around the epithelial elements.[1][6]
Notes:
- Tumour may vaguely resemble a phyllodes tumour.[1]
- Cambium layer - seen in: adenosarcoma, botryoid RMS.[6]
DDx:
Images
IHC
- CD10 +ve.[1]
- ER +ve.
- PR +ve.
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 McCluggage, WG. (Mar 2010). "Mullerian adenosarcoma of the female genital tract.". Adv Anat Pathol 17 (2): 122-9. doi:10.1097/PAP.0b013e3181cfe732. PMID 20179434.
- ↑ Abu, J.; Ireland, D.; Brown, L. (Apr 2007). "Adenosarcoma of an endometrial polyp in a 27-year-old nulligravida: a case report.". J Reprod Med 52 (4): 326-8. PMID 17506376.
- ↑ 3.0 3.1 Verschraegen, CF.; Vasuratna, A.; Edwards, C.; Freedman, R.; Kudelka, AP.; Tornos, C.; Kavanagh, JJ.. "Clinicopathologic analysis of mullerian adenosarcoma: the M.D. Anderson Cancer Center experience.". Oncol Rep 5 (4): 939-44. PMID 9625851.
- ↑ Arend, R.; Bagaria, M.; Lewin, SN.; Sun, X.; Deutsch, I.; Burke, WM.; Herzog, TJ.; Wright, JD. (Nov 2010). "Long-term outcome and natural history of uterine adenosarcomas.". Gynecol Oncol 119 (2): 305-8. doi:10.1016/j.ygyno.2010.07.001. PMID 20688363.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1089. ISBN 0-7216-0187-1.
- ↑ 6.0 6.1 URL: http://www.medilexicon.com/medicaldictionary.php?t=48297. Accessed on: 9 August 2011.