Primary biliary cholangitis
Primary biliary cirrhosis, abbreviated PBC, is a rare medical liver disease.
| Primary biliary cholangitis | |
|---|---|
| Diagnosis in short | |
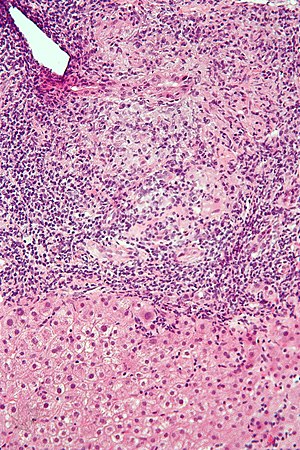 Primary biliary cirrhosis. H&E stain. | |
|
| |
| LM | "florid duct lesion": intraepithelial lymphocytes - in bile duct, bile duct epithelial cells with eosinophilic cytoplasm; plasma cells; +/-granulomas (close to bile duct); +/-"garland" cirrhosis -- has irregular border |
| LM DDx | sarcoidosis, primary sclerosing cholangitis, viral hepatitis, autoimmune hepatitis, drug-induced liver disease, Hodgkin's lymphoma |
| Site | liver - see medical liver diseases |
|
| |
| Associated Dx | other autoimmune conditions, e.g. celiac disease, Sjögren syndrome |
| Clinical history | woman, middle age |
| Symptoms | pruritis |
| Blood work | AMA +ve |
General
Epidemiology:
- Female>male (~9:1).[1]
- Usually middle age.
- Associated with other autoimmune conditions (Sjögren syndrome, progressive systemic sclerosis, celiac disease).
Etiology:
- Autoimmune.
Serology:
- AMA +ve.[2]
Classic presentation:
- Pruritis.
Pathophysiology:
- Septal bile duct attacked.
Treatment:
- Ursodeoxycholic acid.
- May be indication for transplant.
Microscopic
Features:
- "Florid duct lesion":[3]
- Intraepithelial lymphocytes - in bile duct - key feature.
- Bile duct epithelial cells with eosinophilic cytoplasm.[4]
- Plasma cells.
- Granulomas - close to bile duct.
- Seen in classic presentation -- often not present or poorly formed.
- Focal damage (may be missed on biopsy -- due to sampling).
- "Garland" cirrhosis -- has irregular border (unlike in EtOH).
- Garland originally "wreath of flowers" (in French).[5]
Notes:
- PAS stain useful for examining basement membrane... which is lost in PBC.
- Lobular inflammation should be minimal.
- May cause cholestatic picture.[6]
DDx:[7]
- Sarcoidosis (if granulomas present).
- Primary sclerosing cholangitis.
- Viral hepatitis.
- Autoimmune hepatitis.
- Drug-induced liver disease.
- Hodgkin's lymphoma.[8]
Images
www:
Primary biliary cirrhosis. Inflamed triads [arrows] amid undisturbed hepatocytes (Row 1 Left 40X). Granuloma in portal triad (Row 1 Right 400X). Florid duct lesion (Row 2 Left 400X). Triad missing interlobular bile duct (Row 2 Right 400X).
Primary biliary cirrhosis. AMA positive. Viral serology/ANA negative. No definite granulomas. Ill defined triads, inflamed lobule (Row 1 Left 40X). Triad without a bile duct. Macrophages & occasional lymphocytes without epithelioid cells needed for granuloma and space where bile duct likely once was [cyan arrowhead] (Row 1 Right 400X). PAS without diastase shows triad lacking bile duct and piecemeal necrosis (Row 2 Left 200X). PAS with diastase shows bile duct/proliferating bile ductules with epithelial injury and hepatocytes with ballooning degeneration (Row 2 Right 400X). Trichrome shows space of Disse collagenization and periportal fibrosis without definite bridging (Row 3 Left 100X). Iron stain shows isolated focus of hepatocytes with cytoplasmic blue granules (Row 3 Right 200X).
Primary biliary cirrhosis. Two inflamed triads accompany acini with mild steatosis (Row 1 Left 20X). A triad bears a poorly formed granuloma [yellow arrowhead]. A bile duct is also seen [red arrowhead] (Row 1 Right 200X). A triad lacks a bile duct (Row 2 Left 200X). Trichrome of the same triad shows portal fibrosis (Row 2 Right 200X).
Primary biliary cirrhosis with bridging fibrosis. Acini & lobules distorted by inflammation (Row 1 Left 40X) Loose granuloma in triad without duct (Row 1 Right 200X) Well-formed granuloma (Row 2 Left 200X) Piecemeal necrosis, PAS without diastase (Row 2 Right 200X) Damaged bile duct, PAS with diastase (Row 3 Left 400X) Bridging fibrosis, trichrome (Row 3 Right,200X)
Primary biliary cirrhosis with Metavir stage 4 fibrosis (extensive fibrosis/cirrhosis). The patient was AMA positive and ANA negative. A. Inflamed tracts and bridges are intensely inflamed, with odd appearing edges of hepatocytes (arrows), suggestive of a jig saw pattern [40x]. B. Trichrome shows thin fibrous bands bounding regenerative isles (arrows) [Trichrome, 100X]. C. Reticulin shows two cell thick cords and cords lacking orientation, documenting regeneration; black lines about single cells document piecemeal necrosis [100X]. D. Lymphocytes, plasma cells, and macrophages, show piecemeal necrosis, surrounding hepatocytes (cyan arrows), as well as spreading into the lobule (green arrows), with aggregates reflecting spotty necrosis (black arrow). [400X]. E. PAS with diastase highlights a proliferated bile ductule (arrows) with epithelial damage [400X]. F. PAS with diastase shows an arteriole (green arrow) at great distance from an isolated bile ductule at the periphery of the triad (cyan arrow), consistent with loss of bile duct; neutrophils (black arrows) do not prove ascending cholangitis [400X].
Staging PBC
PBC is staged according to Ludwig:[9]
- Stage 1: Portal - inflammation or bile duct abnormalities.
- Stage 2: Periportal - periportal fibrosis (enlargement of portal tracts) +/- inflammation.
- Stage 3: Septal - septal fibrosis +/-inflammation in septa.
- Stage 4: Cirrhosis - nodules of hepatocytes +/- inflammation.
Notes:
- There can be significant variation in staging on biopsy - due to variability of fibrosis in a PBC liver.[10]
- "Worst area" in biopsy specimen is used to determine stage.
See also
References
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 162. ISBN 978-0470519035.
- ↑ Nguyen, DL.; Juran, BD.; Lazaridis, KN. (Oct 2010). "Primary biliary cirrhosis.". Best Pract Res Clin Gastroenterol 24 (5): 647-54. doi:10.1016/j.bpg.2010.07.006. PMID 20955967.
- ↑ Nakanuma, Y.; Harada, K. (Sep 1993). "Florid duct lesion in primary biliary cirrhosis shows highly proliferative activities.". J Hepatol 19 (2): 216-21. PMID 7905494.
- ↑ OA. 11 September 2009.
- ↑ http://dictionary.reference.com/browse/garland
- ↑ Grimm, D.; Thimme, R. (Apr 2011). "[Cholestatic liver diseases].". Ther Umsch 68 (4): 195-9. doi:10.1024/0040-5930/a000150. PMID 21452140.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 163. ISBN 978-0470519035.
- ↑ Vanishing bile duct syndrome and Hodgkin disease: a case series and review of the literature. Pass AK, McLin VA, Rushton JR, Kearney DL, Hastings CA, Margolin JF. J Pediatr Hematol Oncol. 2008 Dec;30(12):976-80. PMID 19131796.
- ↑ PBC. eMedicine.com. URL: http://emedicine.medscape.com/article/171117-diagnosis. Accessed on: 22 September 2009.
- ↑ J Clin Pathol. 1996 July; 49(7): 556-559. Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=500569. Accessed on: September 22, 2009.