Teratoma
Jump to navigation
Jump to search
Teratoma is a common germ cell tumour. Most are benign. Some are malignant. Some are quite weird.
| Teratoma | |
|---|---|
| Diagnosis in short | |
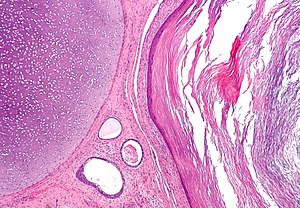 Mature teratoma. H&E stain. | |
|
| |
| LM | classically all three germ layers: endoderm (skin, (mature) CNS), mesoderm (muscle, bone, connective tissue, blood), ectoderm (internal organs) |
| Subtypes | mature teratoma, immature teratoma, strumal carcinoid, struma ovarii, fetus in fetu (subtype of mature teratoma) |
| LM DDx | mixed germ cell tumour, squamous cell carcinoma, epidermoid cyst of the testis (testis only) |
| Gross | may contain identifiable hair and/or teeth, typically cystic and solid |
| Grossing notes | orchiectomy grossing |
| Staging | testicular cancer staging |
| Site | ovary, testis, other |
|
| |
| Associated Dx | ovarian torsion (if large) |
| Symptoms | +/- abdominal pain (ovarian torsion) |
| Prevalence | common - esp. mature teratoma |
| Prognosis | benign or malignant, recurrences with (malignant) teratoma usu. favourable |
| Clin. DDx | malignant mass (germ cell tumour, metastasis) |
General
- May be benign or malignant.
- Are supposed to consists of all three germ layers - this is not always true.
- May be associated with sacral agenesis.[1]
- Teratoma only recurrences of germ cell tumours have good prognosis.[2]
Important note:
- The site of the tumour, age and sex are very important for predicting the behaviour of a teratoma:[3]
- Immature teratomas may have a benign or malignant behaviour.
- Mature teratomas may have a benign or malignant behaviour.
- CNS teratomas are overrepresented in males.[4]
- Intracranial teratomas are usually located in midline locations such as the pineal region, suprasellar cistern, basal ganglia, and thalamus.[5]
Classification
- Mature.
- Common in females.
- Usually benign.
- Mature component may give rise to a malignancy like elsewhere in the body.
- Most common malignancy arising from a mature teratoma: squamous cell carcinoma.
- Immature.
- Uncommon.
- Often malignant.
- Monodermal.
- Rare.
- Highly specialized.
Mature teratoma
Features - three germ cell layers (usually):[6]
- Ectoderm:
- Skin, (mature) CNS.
- Mesoderm:
- Muscle, bone, connective tissue, blood.
- Endoderm:
- Internal organs.
Note:
- May consist of skin only - in which case it is commonly called a dermoid.
DDx:
Images
Fetus in fetu
- Grouped with mature teratoma, as it is considered a well-developed mature teratoma.[7][8]
- It has been suggested they are distinct from teratomas.[9]
- They could be thought of as a parasitic twin.
- It has been suggested they are distinct from teratomas.[9]
Features:
- Discrete mass consisting of mature tissues that form well-developed structures with the normal anatomical relations.
- Separated from teratoma by the presence of a vertebral column.[10]
Immature teratoma
Features:
- Immature if neural tissue is present:[11]
- Vaguely resembles pseudostratified respiratory epithelium.
- Islands of small hyperchromatic cells - "blastema".
- +/-Cartilage.
- +/-Adipocytes.
- +/-Colonic type mucosa.
- +/-Stratified squamous epithelium (skin).
DDx:[12]
Images
Other images:
- Immature teratoma - myxomatous stroma (webpathology.com).
- Immature teratoma - blastema (webpathology.com).
- Immature teratoma - primitive neuroepithelium (webpathology.com).
- Immature teratoma - primitive neuroepithelium (ouhsc.edu).
Grading (immature)
Based on quantity of immature neuroepithelium:[13][14][15]
- G0 - mature teratoma; no immature neuroepithelium.
- G1 - less than one lower power field (LPF) of immature neuroepithelium; LPF defined field at 4X magnification.
- G2 - 1-3 LPFs.
- G3 - more than 3 LPFs.
Note:
- LPF not adequately defined - see LPFitis. Same BS as HPF.
IHC (immature)
Features:
- Primitive neuroepithelium:[16]
- Neuron-specific enolase (NSE) +ve.
- Neuron-specific B tubulin +ve.
- Synaptophysin +ve.
Monodermal teratomas
Struma ovarii
Features:
- Thyroid tissue present - colloid is seen.
- May develop pathologies seen in the thyroid gland.
Notes:
- Various quantity requirements:
- Wei et al. state that the thyroid tissue must comprise >50% of the mass or have a thyroid-associated malignancy (e.g. papillary thyroid carcinoma) for the label struma ovarii.[17]
- Nucci and Oliva state the thyroid tissue must be "predominant".[18]
- Benign thyroid tissue is not uncommon in teratomas (5-20%).[17]
Images
Strumal carcinoid
- Has components that suggest:
- Carcinoid (neuroendocrine tumour).
- Nuclei with stippled chromatin (salt-and-pepper chromatin).
- Thyroid - cystic spaces/follicular-like structures.
- Carcinoid (neuroendocrine tumour).
Images
Epidermoid cyst
Some authors consider epidermoid cyst as a monodermal teratoma.[21]
Sign out
Mature teratoma
Mass, Right Ovary, Excision: - Mature teratoma with dermal elements and mature neural tissue. - NEGATIVE for evidence of malignancy.
Block letters
CYST ("DERMOID"), RIGHT OVARY, CYSTECTOMY:
- MATURE CYSTIC TERATOMA.
CYST, LEFT OVARY, CYSTECTOMY: - MATURE CYSTIC TERATOMA. - NEGATIVE FOR MALIGNANCY.
Residual germ cell tumour
ANTERIOR CAVAL MASS, RESECTION: - RESIDUAL MATURE TERATOMA, COMPLETELY EXCISED IN THE PLANE OF SECTION.
Micro
The sections show ovarian parenchyma with a lesion consisting of benign dermal, gastrointestinal and neural elements. The neural elements show focal degenerative changes with macrophages, and giant cells. Siderophages are present. The lesion is excised in the planes of section.
See also
References
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 176450
- ↑ Michael, H.; Lucia, J.; Foster, RS.; Ulbright, TM. (Feb 2000). "The pathology of late recurrence of testicular germ cell tumors.". Am J Surg Pathol 24 (2): 257-73. PMID 10680894.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/GermCell_11protocol.pdf. Accessed on: 29 April 2012.
- ↑ Zygourakis, CC.; Davis, JL.; Kaur, G.; Ames, CP.; Gupta, N.; Auguste, KI.; Parsa, AT. (Jan 2015). "Management of central nervous system teratoma.". J Clin Neurosci 22 (1): 98-104. doi:10.1016/j.jocn.2014.03.039. PMID 25150764.
- ↑ Lee, YH.; Park, EK.; Park, YS.; Shim, KW.; Choi, JU.; Kim, DS. (Dec 2009). "Treatment and outcomes of primary intracranial teratoma.". Childs Nerv Syst 25 (12): 1581-7. doi:10.1007/s00381-009-0974-8. PMID 19693515.
- ↑ Moore, Keith L.; Persaud, T.V.N. (2002). The Developing Human: Clinically Oriented Embryology (7th ed.). Saunders. pp. 83. ISBN 978-0721694122.
- ↑ Heifetz, SA.; Alrabeeah, A.; Brown, BS.; Lau, H. (1988). "Fetus in fetu: a fetiform teratoma.". Pediatr Pathol 8 (2): 215-26. PMID 3045784.
- ↑ Basu, A.; Jagdish, S.; Iyengar, KR.; Basu, D. (Oct 2006). "Fetus in fetu or differentiated teratomas?". Indian J Pathol Microbiol 49 (4): 563-5. PMID 17183856.
- ↑ Basu, A.; Jagdish, S.; Iyengar, KR.; Basu, D. (Oct 2006). "Fetus in fetu or differentiated teratomas?". Indian J Pathol Microbiol 49 (4): 563-5. PMID 17183856.
- ↑ Majhi, AK.; Saha, K.; Karmakar, M.; Sinha Karmakar, K.; Sen, A.; Das, S. (2007). "Fetus in fetu--a mystery in medicine.". ScientificWorldJournal 7: 252-7. doi:10.1100/tsw.2007.56. PMID 17334616.
- ↑ RS. 2 May 2010.
- ↑ Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 34. ISBN 978-0781767798.
- ↑ Harms D, Zahn S, Göbel U, Schneider DT (2006). "Pathology and molecular biology of teratomas in childhood and adolescence". Klin Padiatr 218 (6): 296–302. doi:10.1055/s-2006-942271. PMID 17080330.
- ↑ Ulbright TM (February 2005). "Germ cell tumors of the gonads: a selective review emphasizing problems in differential diagnosis, newly appreciated, and controversial issues". Mod. Pathol. 18 Suppl 2: S61–79. doi:10.1038/modpathol.3800310. PMID 15761467. http://www.nature.com/modpathol/journal/v18/n2s/full/3800310a.html.
- ↑ O'Connor DM, Norris HJ (October 1994). "The influence of grade on the outcome of stage I ovarian immature (malignant) teratomas and the reproducibility of grading". Int. J. Gynecol. Pathol. 13 (4): 283–9. PMID 7814189.
- ↑ Craver RD, Lipscomb JT, Suskind D, Velez MC (October 2001). "Malignant teratoma of the thyroid with primitive neuroepithelial and mesenchymal sarcomatous components". Ann Diagn Pathol 5 (5): 285–92. doi:10.1053/adpa.2001.27918. PMID 11598856.
- ↑ 17.0 17.1 Wei, S.; Baloch, ZW.; LiVolsi, VA. (Sep 2015). "Pathology of Struma Ovarii: A Report of 96 Cases.". Endocr Pathol. doi:10.1007/s12022-015-9396-1. PMID 26374222.
- ↑ Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 524. ISBN 978-0443069208.
- ↑ Gorin, I.; Sastre-Garau, X. (Jun 2008). "Strumal carcinoid tumor of the ovary.". J Clin Oncol 26 (16): 2780-1. doi:10.1200/JCO.2008.16.1620. PMID 18509188.
- ↑ Tamsen, A.; Mazur, MT. (Feb 1992). "Ovarian strumal carcinoid in association with multiple endocrine neoplasia, type IIA.". Arch Pathol Lab Med 116 (2): 200-3. PMID 1346363.
- ↑ Aneiros-Fernandez, J.; Arias-Santiago, S.; Cancela-Diez, B.; O'Valle, F.; Cachaza, JA. (Dec 2010). "Intratesticular epidermoid cyst: a rare tumor.". J Clin Med Res 2 (6): 281-3. doi:10.4021/jocmr474w. PMID 22043263.