Orchiectomy grossing
Jump to navigation
Jump to search
This article deals with orchiectomy grossing.
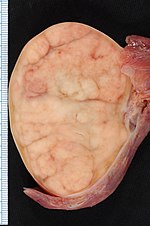
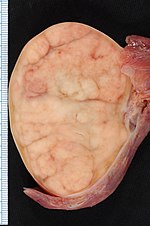
Orchiectomy specimen showing testis replaced by tumour (proven to be seminoma). (WC/Ed Uthman)
Introduction
Orchiectomies are typically done for testicular tumours.
They may be done for chronic pain or to control prostate cancer.
Protocol
Dimensions and weight:
- Laterality: [ left / right ].
- Weight: ___ grams.
- Testis: ___ x ___ x ___ cm.
- Epididymis: ___ x ___ x ___ cm.
- Spermatic cord - length: __ cm, diameter: ___ cm.
- Inking: [colour].
Tumour:
- Size: ___ x ___ x ___ cm.
- Colour: [ tan / white / variable ].
- Firmness: [ firm / soft ].
- Morphology: [solid / cystic / solid and cystic - with ___ % cystic].
- Circumscription: [circumscribed / infiltrative border ].
- Hemorrhage: [ absent / present ].
- Necrosis: [ absent / present ].
- Extension into tunica albuginea: [ not identified / indeterminate / present ].
- Extension into the epididymis: [ not identified / indeterminate / present ].
Other - after sectioning:
- Testicular parenchyma: [ brown-tan, unremarkable / ___ ].
- Spermatic cord: [ unremarkable / ___ ].
Representative sections are submitted as follow:
- Spermatic cord resection margin, en face.
- Spermatic cord mid-section, cross section.
- Spermatic cord close to testis.
- Tumour in relation to epididymis.
- Tumour and rete testis.
- Tumour with testicular coverings.
- Additional tumour sections.
- Testis distant from the tumour.
Protocol notes
- The tumour should be submitted in total if this can be done in less than 10 cassettes.
- Lester's book (2nd Ed.) recommends 1 cassette per cm of maximal tumour dimension.[1]
Staging
Based on AJCC 7th Edition:[2][3]
- pT1 - confined to the testis or epididymis, no lymphovascular invasion.
- pT2 - into tunica vaginalis or lymphovascular invasion.
- pT3 - into spermatic cord.
- pT4 - into the scrotum.
Notes:[3]
- Invasion into the epididymis, rete testis or tunica albuginea does not change the stage.
- Rete testis involvement and hilar involvement may be seen or suspected at the time of cut-up. Both of these are poor prognosticators;[4] however, they are not incorporated into the (AJCC 7th Ed.) staging.
Alternate approaches
See also
Related protocols
References
- ↑ Lester, Susan Carole (2005). Manual of Surgical Pathology (2nd ed.). Saunders. pp. 409. ISBN 978-0443066450.
- ↑ URL: https://en.wikibooks.org/wiki/Radiation_Oncology/Testis/Staging. Accessed on: 15 December 2014.
- ↑ 3.0 3.1 URL: http://www.cancer.org/cancer/testicularcancer/detailedguide/testicular-cancer-staging. Accessed on: 15 December 2014.
- ↑ Yilmaz, A.; Cheng, T.; Zhang, J.; Trpkov, K. (Apr 2013). "Testicular hilum and vascular invasion predict advanced clinical stage in nonseminomatous germ cell tumors.". Mod Pathol 26 (4): 579-86. doi:10.1038/modpathol.2012.189. PMID 23238629.